Physician Liability: Legal Risks of Prescribing Generic Medications
When you prescribe a generic medication, you’re not just choosing a cheaper option-you’re stepping into a legal minefield most doctors don’t talk about. In 2025, more than 90% of prescriptions in the U.S. are filled with generics. That’s not just a cost-saving trend; it’s a liability time bomb. And if something goes wrong, the patient can’t sue the manufacturer. Federal law won’t let them. So who’s left? Physician liability becomes the only target.
Why Generic Drugs Are Legally Different
In 2011, the U.S. Supreme Court ruled in PLIVA v. Mensing that generic drug makers can’t be held responsible for failing to update warning labels. Why? Because federal law forces them to copy the brand-name label exactly. They can’t add new warnings, change dosages, or even tweak the wording-even if new safety data emerges. That rule was reinforced in 2013 with Mutual Pharmaceutical v. Bartlett, where a woman lost 65% of her skin after taking generic sulindac. The court said: no lawsuit against the maker. Not because the drug was safe. But because the law made it impossible for the manufacturer to act. That left patients with nowhere to turn. And over time, lawyers started looking at the person who wrote the prescription: you.Your Legal Duty Isn’t Any Different-But the Risks Are
Legally, your duty to your patient doesn’t change whether you write a brand-name or generic prescription. You still owe them the standard of care: proper diagnosis, appropriate drug selection, adequate warning, and follow-up. But here’s the twist: when you prescribe a brand-name drug, the manufacturer carries the weight of liability. If the label is wrong, the patient sues the company. If the drug causes harm, the company pays. With generics? That safety net is gone. The manufacturer is shielded. So now, if a patient develops Stevens-Johnson syndrome from a generic anticonvulsant, or liver failure from a generic diabetes drug, your name is on the prescription. And in court, your defense isn’t “the manufacturer didn’t warn us.” It’s “did you warn them?”The State-by-State Patchwork You Can’t Ignore
Forty-nine states let pharmacists substitute generics automatically-unless you write “dispense as written” or “do not substitute.” That sounds simple. But in 17 states, the pharmacist doesn’t even have to tell you they made the switch. In 32 states, they have to notify you within 72 hours. That means you could be treating a patient for a reaction to a drug you didn’t even know they got. And it gets messier. In Illinois, courts have ruled that generic manufacturers can be held liable if a drug is inherently dangerous and the label doesn’t reflect known risks. In Alabama? Brand-name manufacturers were briefly held liable for injuries caused by generics-until the state legislature passed a law in 2015 shutting that door. That’s not a national rule. It’s a legal lottery. Your liability depends on where you practice.What’s Changing in the Clinic
Doctors aren’t waiting for lawsuits to happen. They’re changing how they practice. A 2022 AMA survey found 68% of physicians feel more anxious prescribing generics. Forty-two percent admit they sometimes choose the more expensive brand-name drug-not because it’s better, but because they’re scared of being sued later. One doctor in Massachusetts now adds 15 to 20 minutes to every visit just to document warnings. He writes out side effects by hand, reads them to the patient, and has them sign a form. Electronic health records have caught on. Epic Systems updated its platform in 2021 to require a mandatory checkbox: “Discussed generic substitution risks with patient.” If you skip it, the system won’t let you sign the prescription.
Documentation Is Your Best Shield
The difference between a lawsuit and a closed case? Paperwork. A 2023 risk management report found that physicians who document specific, detailed conversations about generic substitution reduce their liability exposure by 58%. Generic notes like “medication discussed” or “patient educated” won’t cut it. You need specifics:- “I explained that [generic name] may cause dizziness and instructed you not to drive or operate machinery until you know how it affects you.”
- “We discussed the risk of severe skin reactions with this medication and agreed to monitor for rash or blistering.”
- “You asked about switching to generic. I advised against it because of your history with warfarin and narrow therapeutic index.”
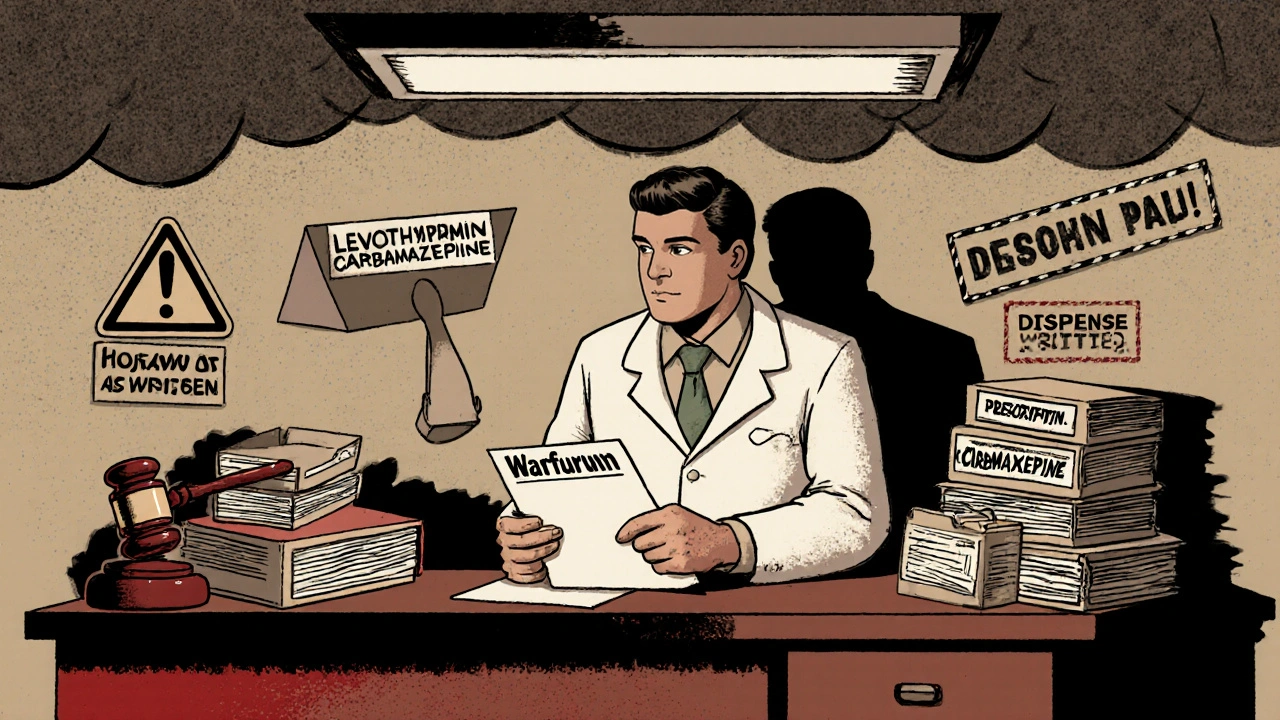
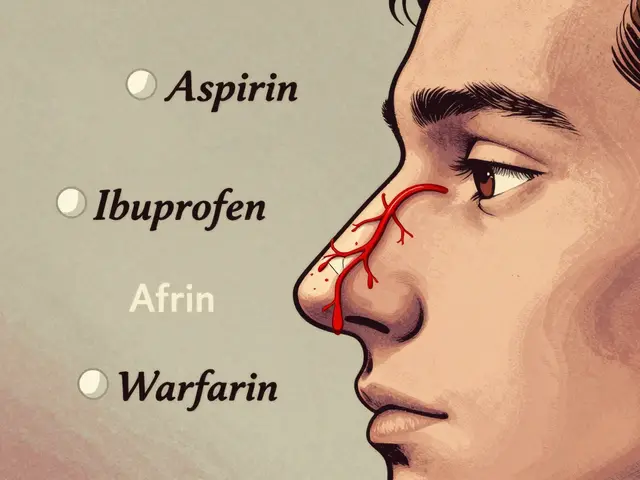
Which Drugs Are Most Dangerous to Substitute?
Not all generics are equal. Some drugs have a narrow therapeutic index-meaning the difference between a safe dose and a toxic one is tiny. For these, substitution can be deadly:- Warfarin - Even small changes in bioavailability can cause dangerous bleeding or clots.
- Levothyroxine - Switching brands can lead to under- or over-treatment of thyroid function, affecting heart rhythm and bone density.
- Anti-epileptics - Carbamazepine, phenytoin, valproate: small variations can trigger seizures.
- Immunosuppressants - Cyclosporine, tacrolimus: transplant patients can reject organs if levels drop.
Insurance and Costs Are Rising
Your malpractice insurance isn’t ignoring this trend. The American Professional Agency reports a 7.3% average premium surcharge for physicians who routinely authorize generic substitutions without documented counseling. That’s not a small fee. That’s hundreds, sometimes thousands, more per year. And it’s not just premiums. Between 2014 and 2019, physician-targeted lawsuits involving generic drugs jumped 37%. The average settlement? $327,500. One case in Texas ended in a $1.2 million payout after a patient developed toxic epidermal necrolysis from a generic antipsychotic. The manufacturer was immune. The doctor wasn’t.
What’s Next? The Legal Tide Is Still Rising
The Supreme Court has refused to revisit the Mensing/Bartlett rulings. But lower courts are carving out exceptions. In March 2023, the 9th Circuit ruled that if a brand-name manufacturer updates its label with new safety warnings, the generic maker has a duty to follow suit. That’s a crack in the immunity wall. Meanwhile, 18 states introduced legislation in 2023 requiring pharmacists to notify physicians within 24 hours of substituting high-risk generics. The AMA is pushing for this as a national standard. If it passes, you’ll get alerts. But until then? You’re still on the hook.What You Can Do Today
You don’t need to stop prescribing generics. They’re safe, effective, and necessary. But you need to protect yourself:- Know your state’s substitution laws-do pharmacists have to notify you? Can you block substitution?
- Use “dispense as written” for high-risk drugs-warfarin, levothyroxine, anticonvulsants, immunosuppressants.
- Document specific counseling-don’t say “medication discussed.” Say exactly what you told the patient.
- Don’t assume the patient understands-many don’t know the difference between brand and generic. Explain it plainly.
- Update your EHR-make sure your system has the mandatory counseling fields turned on.
Final Reality Check
You didn’t create this legal mess. But you’re living in it. The system is broken. Manufacturers are shielded. Patients are hurt. And you’re the only one left with the power-and the responsibility-to prevent harm. The law doesn’t care if you followed guidelines. It doesn’t care if you thought the generic was fine. It only cares if you can prove you warned your patient. And if you can’t? That’s your liability.Can a doctor be sued if a patient has a bad reaction to a generic drug?
Yes. Under federal law, generic drug manufacturers are protected from liability for failure-to-warn claims. If a patient is injured, the only viable legal target is often the prescribing physician. Courts look at whether the doctor properly selected the drug, documented patient counseling, and followed standard care. Without strong documentation, liability is likely.
Is it legal to prescribe brand-name drugs to avoid liability?
Yes, it’s legal. Many physicians now prescribe brand-name drugs-even when generics are available-not because they’re clinically superior, but to reduce their own legal risk. While this increases patient costs, it’s a defensive practice growing in response to the current legal environment. Ethically, it’s debated, but legally, it’s protected.
What should I write in my notes to protect myself?
Avoid vague phrases like “medication discussed.” Instead, write: “I explained that [generic name] may cause [specific side effect], and advised avoiding [specific activity] while taking it. Patient acknowledged understanding and signed consent form.” Specific, dated, and personalized notes are your best legal defense.
Do I need to block generic substitution for all medications?
No. For most medications, generic substitution is safe and appropriate. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, and certain anti-seizure meds-you should always write “dispense as written.” These are the drugs most likely to cause harm if bioavailability shifts even slightly.
Has anything changed since the 2013 Supreme Court rulings?
The core legal protection for generic manufacturers remains unchanged. But in 2023, a federal appeals court created a narrow exception: if a brand-name manufacturer updates its warning label, generic makers must follow suit. This is the first crack in the immunity wall, but it’s limited. For now, physicians still bear the primary responsibility for patient warnings.


15 Comments
Jennifer Walton
November 15 2025It’s not about generics. It’s about a system that outsources risk to the person with the least power. The manufacturer makes billions, the insurer profits, and the doctor gets sued for following the law. We’re not doctors-we’re liability magnets.
Kihya Beitz
November 15 2025So let me get this straight… the pharma bros get a free pass, but if I prescribe a $3 pill and someone sneezes wrong, I’m on the hook? 😂💸
Chris Bryan
November 17 2025Big Pharma bought this law. The FDA’s a puppet. The government lets them poison people and hide behind paperwork. This isn’t medicine-it’s corporate warfare, and we’re the cannon fodder.
Jonathan Dobey
November 17 2025Ah, the tragic irony of neoliberal healthcare: the very mechanism designed to ‘democratize’ access-generic substitution-has become a legal trapdoor for the marginalized practitioner. The state, in its infinite wisdom, has created a paradox where cost-efficiency becomes culpability. We are not healers anymore-we are forensic accountants of informed consent.
ASHISH TURAN
November 18 2025This is why I always write ‘dispense as written’ for warfarin and levothyroxine. No argument. No risk. I’ve seen patients crash because of a 5% bioavailability shift. It’s not paranoia-it’s practice.
Ryan Airey
November 18 2025Doctors who prescribe generics without documenting every breath their patient takes are asking to be sued. This isn’t complicated. If you’re not documenting like your license depends on it, you deserve to lose it.
Hollis Hollywood
November 19 2025I’ve had patients cry in my office because they couldn’t afford the brand-name drug. And now you’re telling me I should charge them more just because I’m scared of a lawsuit? I get the paperwork. I do. But this system makes me feel like I’m choosing between their health and my livelihood. That’s not a choice-it’s a moral collapse.
Aidan McCord-Amasis
November 19 2025Generic = cheaper. Brand = $$$ and legal armor. 🤷♂️💊 #DoctorsDontGetPaidEnough
Adam Dille
November 20 2025I get it. I really do. But I also think we need to stop blaming doctors and start fixing the system. Maybe if manufacturers had to update labels when new data came out, we wouldn’t be in this mess. We’re just the ones holding the bag while the real culprits cash checks.
Katie Baker
November 20 2025Thank you for writing this. I’ve been terrified to prescribe generics lately, but I didn’t know how much I was already doing right. I’ve started handwriting the warnings now-just like you said. It’s slow, but it feels safer.
John Foster
November 21 2025Consider the metaphysical weight of this: we are now required to perform performative acts of consent-not because the patient needs to understand, but because the legal fiction demands it. The ritual of signing a form, the hollow echo of ‘did you understand?’-these are not acts of care. They are sacraments of institutional self-preservation. The patient is no longer a person; they are a liability buffer. And we? We are the priests of this secular religion, blessing the altar of corporate immunity with our signatures and our sleepless nights.
Edward Ward
November 21 2025Wait-so if a brand-name company updates its label with a new warning, the generic maker MUST follow suit? That’s huge!!! But only if the brand updates it?! What if they don’t? What if they’re silent? What if they’re waiting for a lawsuit to trigger the change?!!! That’s not a fix-that’s a loophole with teeth!!! And what about the 80% of generics that never get updated because the brand never changed?!!! We’re still on the hook for that!!!
Andrew Eppich
November 23 2025Physicians must adhere to the standard of care. If they fail to document appropriately, they are negligent. The law is clear. The solution is simple: document thoroughly. Blaming the system does not absolve professional responsibility.
Jessica Chambers
November 24 2025So you’re telling me I have to spend 20 extra minutes per patient just to avoid getting sued… and my insurance is still going up? 😑 I’m starting to think medicine is just a job where you get paid in stress and paperwork.
Shyamal Spadoni
November 25 2025they say its a legal minefield but i think its all a big cover up… big pharma owns the courts… the supreme court… even the docs who write about this are paid… i saw a video once… the guy who wrote the article… he got sponsored by a brand name drug company… its all rigged… the generics are fine… its the docs who are the problem… they dont want to learn the new stuff… they just want to keep the old way… and now they wanna blame the law…