Liver function: what to watch, what to test, and how meds fit in
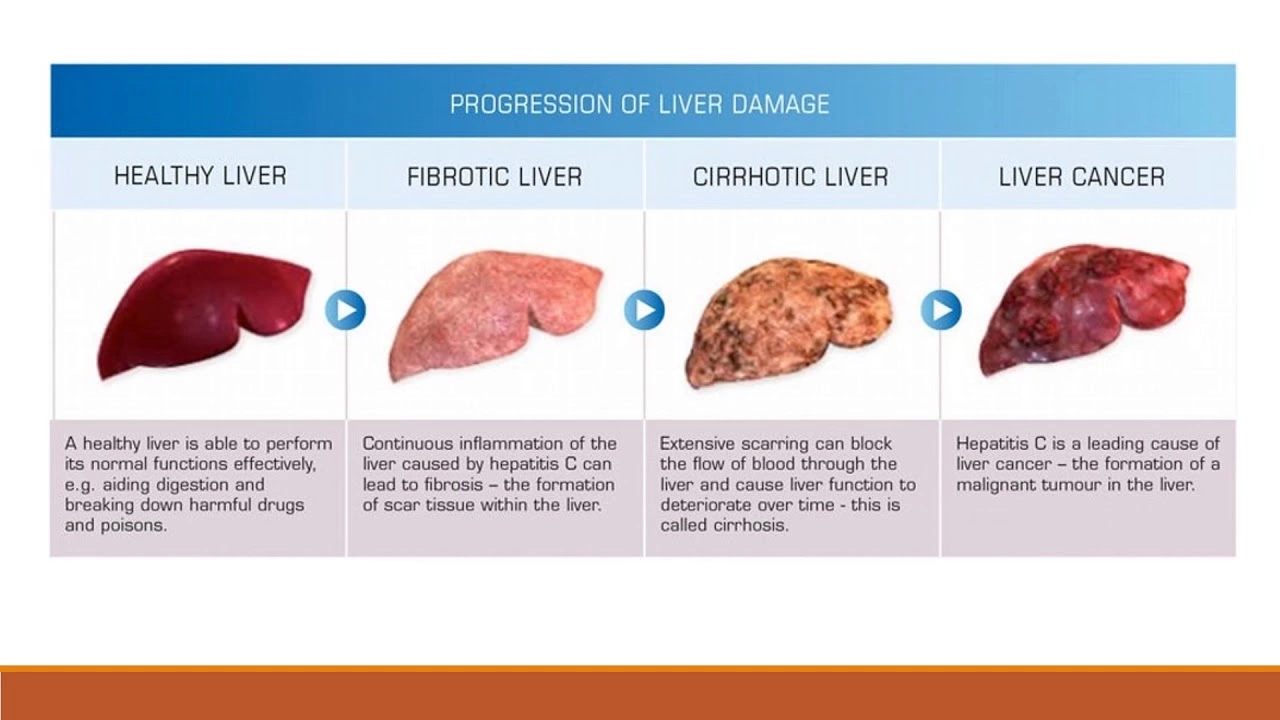
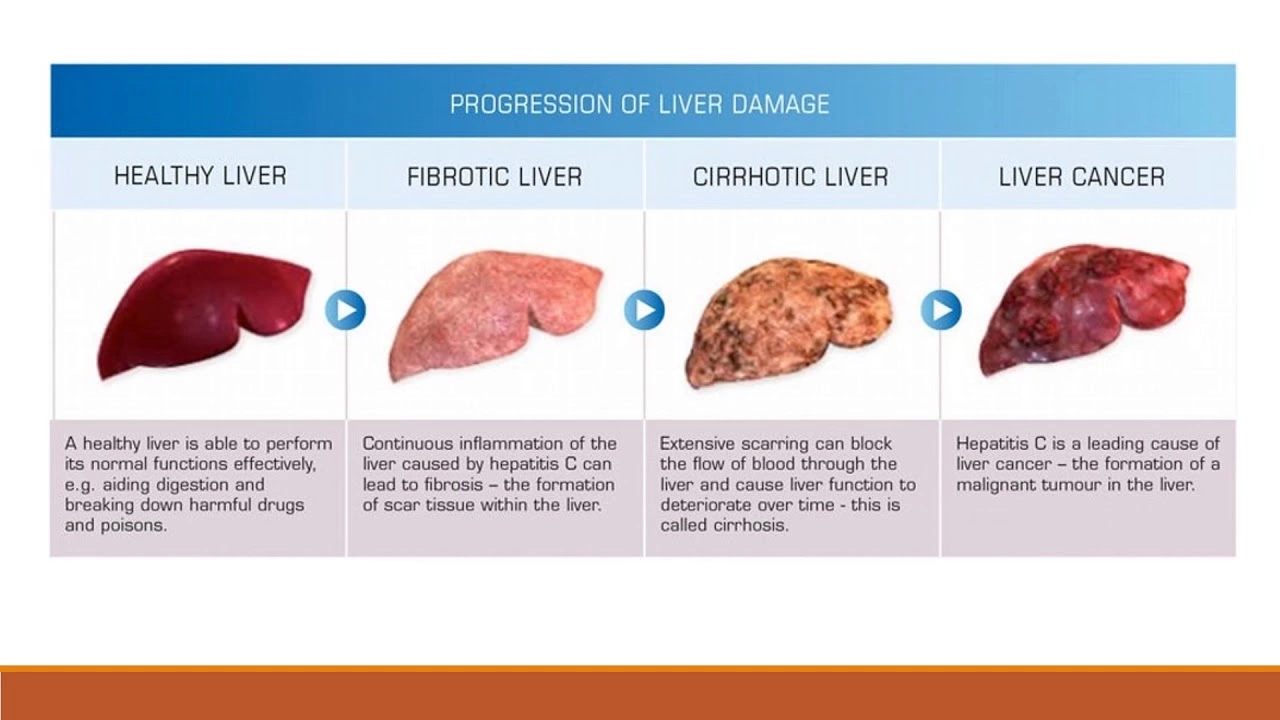
Your liver handles a lot: it filters blood, breaks down drugs, stores nutrients, and helps make bile for digestion. When it’s stressed, you might feel tired, notice jaundice, or have belly pain — but sometimes liver problems show up only in blood tests. If you take regular medicine, or if a doctor mentioned “watch your liver,” this short guide tells you what the common tests mean and what you can do right now.
Key tests and what they mean
Doctors usually check a panel of liver markers. Here’s a quick, practical look at the usual ones:
ALT and AST: These enzymes leak out of liver cells when they’re irritated or damaged. Mild rises can come from fatty liver, some medicines, or alcohol. Bigger jumps need follow-up.
ALP and GGT: These point to bile flow problems or blockage. GGT can help confirm if ALP rises are from the liver versus bone issues.
Bilirubin: Raised bilirubin shows up as yellow skin or eyes (jaundice) and can mean the liver isn’t processing waste normally.
When results are abnormal, doctors often repeat tests, check medications, screen for viral hepatitis, or order an ultrasound. Mild, stable enzyme changes sometimes just need lifestyle fixes and a recheck in a few months.
How medicines and daily choices affect your liver
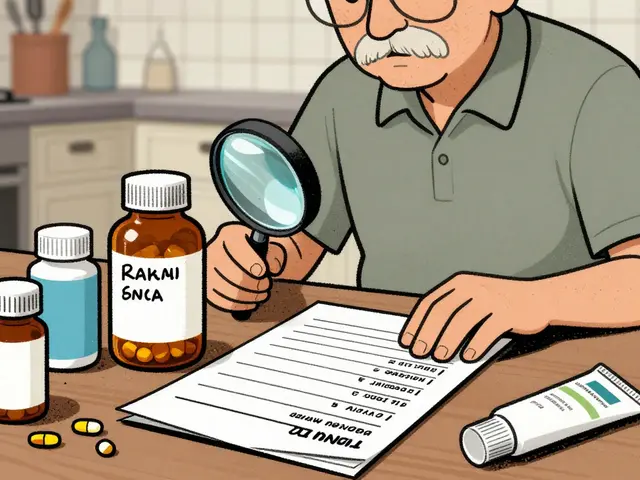
Some drugs can stress the liver. Acetaminophen (paracetamol) is a common cause of liver injury when taken above recommended doses or mixed with alcohol. Other meds — certain antibiotics, antifungals, statins, methotrexate, and some herbal supplements — can also raise liver enzymes in some people. That doesn’t mean you must stop important treatment, but you should:
- Tell your doctor about every pill and supplement you take. Small things like herbal products or extra pain pills matter.
- Avoid alcohol while on high-risk medicines.
- Stick to the recommended dose, especially for acetaminophen. Don’t combine multiple products that contain it.
Simple lifestyle steps go a long way: maintain a healthy weight, eat mostly whole foods, cut sugary drinks, and move regularly. Vaccines for hepatitis A and B are smart if you’re at risk. If you have fatty liver (common with obesity or diabetes), losing even 5–10% of body weight often lowers enzyme levels and improves liver health.
If you have symptoms like persistent belly pain, dark urine, pale stools, or yellowing of skin/eyes, see a doctor right away. Also ask for a liver check before starting long-term medicines that can hurt the liver. Keeping a clear list of your meds, drinking less alcohol, and getting routine blood tests when advised are practical steps that protect your liver without much fuss.
As a blogger, I've recently delved into the topic of Ofloxacin and its impact on liver function. Through my research, I've found that Ofloxacin, a commonly prescribed antibiotic, can sometimes cause liver damage, especially in patients with pre-existing liver conditions. It's essential for individuals to consult their healthcare providers before taking this medication to ensure their safety. Regular monitoring of liver function tests is also crucial to detect any potential issues early on. Overall, it's vital for everyone to be aware of this potential side effect and take necessary precautions when using Ofloxacin.
Continue Reading