NOACs (Direct Oral Anticoagulants): What you need to know
NOACs — also called DOACs — are the newer blood thinners many doctors pick instead of warfarin. You’ve probably heard the names: apixaban, rivaroxaban, dabigatran, and edoxaban. They stop clots without the need for routine INR checks, which is one big convenience. But they still carry risks and require a bit of attention.
When are NOACs used?
Most often NOACs are prescribed to prevent stroke in non-valvular atrial fibrillation and to treat or prevent deep vein thrombosis (DVT) and pulmonary embolism (PE). They’re also used after some surgeries to cut the risk of clotting. If you have a mechanical heart valve or certain valve problems, NOACs may not be suitable — that’s a case where warfarin is still the go-to.
Here are typical dosing examples (talk to your prescriber for your exact dose):
- Apixaban (Eliquis): often 5 mg twice daily for atrial fibrillation.
- Rivaroxaban (Xarelto): often 20 mg once daily (usually with food).
- Dabigatran (Pradaxa): often 150 mg twice daily.
- Edoxaban: often 60 mg once daily.
Doctors adjust doses for kidney function, age, weight, or interacting drugs. Never change dose on your own.
Safety, interactions, and common questions
NOACs don’t need daily blood tests, but they’re still full-strength medicines. Key points to watch:
- Bleeding risk: any unusual bruising, nosebleeds that won’t stop, black stools, coughing up blood, or heavy bleeding — call your doctor or go to ER.
- Kidney function matters: kidneys clear these drugs. If your kidney function is low, dose or drug choice may change.
- Drug interactions: some heart and antifungal meds, and strong P-gp or CYP3A4 inhibitors, can raise NOAC levels. Herbal products like St. John’s wort can lower them. Tell your prescriber about all medicines and supplements.
- Reversal options: there are specific reversal agents (for example, idarucizumab reverses dabigatran; andexanet alfa can reverse some factor Xa inhibitors). Hospitals use these when major bleeding happens.
- Before procedures: you’ll usually stop the NOAC for a short time before surgery. How long depends on the drug, your kidney function, and the bleeding risk of the procedure. Ask the surgeon and the prescriber for a clear plan.
- Missed doses: rules vary. A common approach is to take a missed dose as soon as you remember the same day, but don’t double up. Confirm the rule for your specific medicine with your provider.
If you’re starting a NOAC, bring a list of all your drugs to the appointment, ask how kidney function will be checked, and get clear instructions for missed doses and when to stop before procedures. Simple steps like these lower surprises and keep you safer while on these powerful medicines.
Need more details or plain answers about a specific NOAC? Check with your doctor or pharmacist — and if you want, use our site search to find related articles and drug guides for deeper reading.

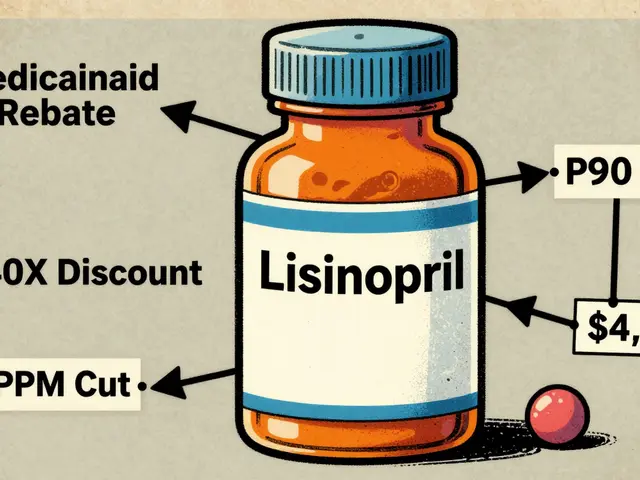
Curious about the future of anticoagulation therapy and whether rivaroxaban will keep its spot among top blood thinners? This article dives deep into how rivaroxaban stacks up against newer treatments, what science is saying about its future, and what patients and doctors need to know. You'll get real-world tips, stats, and honest talk about risks and rewards—no sugarcoating, just clear facts.
Continue Reading