Targeted Therapy: How Tumor Genetics Are Changing Cancer Treatment
For decades, cancer treatment meant one thing: chemotherapy. Harsh, broad-spectrum, and damaging to healthy cells, it was the only tool doctors had. But today, something different is happening. Doctors are no longer treating cancer based on where it lives in the body - lung, breast, colon - but on what’s driving it at the genetic level. This is targeted therapy. It’s not science fiction. It’s happening right now, in hospitals across the U.S. and Europe, and it’s changing survival rates for people with certain cancers.
What Exactly Is Targeted Therapy?
Targeted therapy is a type of cancer treatment that uses drugs to find and attack specific molecules - usually proteins or genes - that are helping cancer cells grow and spread. Unlike chemotherapy, which hits all fast-dividing cells (cancerous or not), targeted drugs are like precision missiles. They go straight for the faulty switches inside cancer cells and flip them off.
The breakthrough came from large-scale research like The Cancer Genome Atlas, which mapped genetic changes in over 20,000 tumor samples. That project revealed that two cancers that look identical under a microscope - say, lung and colon - can have completely different genetic drivers. And that means they need different treatments.
The first big win was imatinib (Gleevec), approved in 2001 for chronic myeloid leukemia. Before imatinib, about 20-30% of patients survived one year. After? Nearly 90%. That wasn’t just an improvement - it was a revolution.
How Do These Drugs Work?
There are two main types of targeted therapies: small molecule inhibitors and monoclonal antibodies.
Small molecule drugs, like osimertinib for EGFR-mutant lung cancer, are designed to slip inside cancer cells and block signals that tell them to grow. They’re taken as pills. Monoclonal antibodies, like trastuzumab for HER2-positive breast cancer, are injected and latch onto proteins on the outside of cancer cells. Once attached, they either mark the cell for destruction by the immune system or block growth signals.
These drugs target specific genetic changes:
- EGFR mutations - common in non-small cell lung cancer
- ALK and ROS1 fusions - found in a small but significant group of lung cancer patients
- BRAF V600E mutations - seen in melanoma and some colorectal cancers
- HER2 amplifications - drive about 20% of breast cancers
- NTRK fusions - rare, but found across many cancer types
What’s remarkable is that drugs like larotrectinib work the same way whether the tumor is in the lung, thyroid, or colon - as long as it has the NTRK fusion. That’s called a tissue-agnostic approach, and it’s changing how we classify cancer.
Why Genomic Testing Is Non-Negotiable
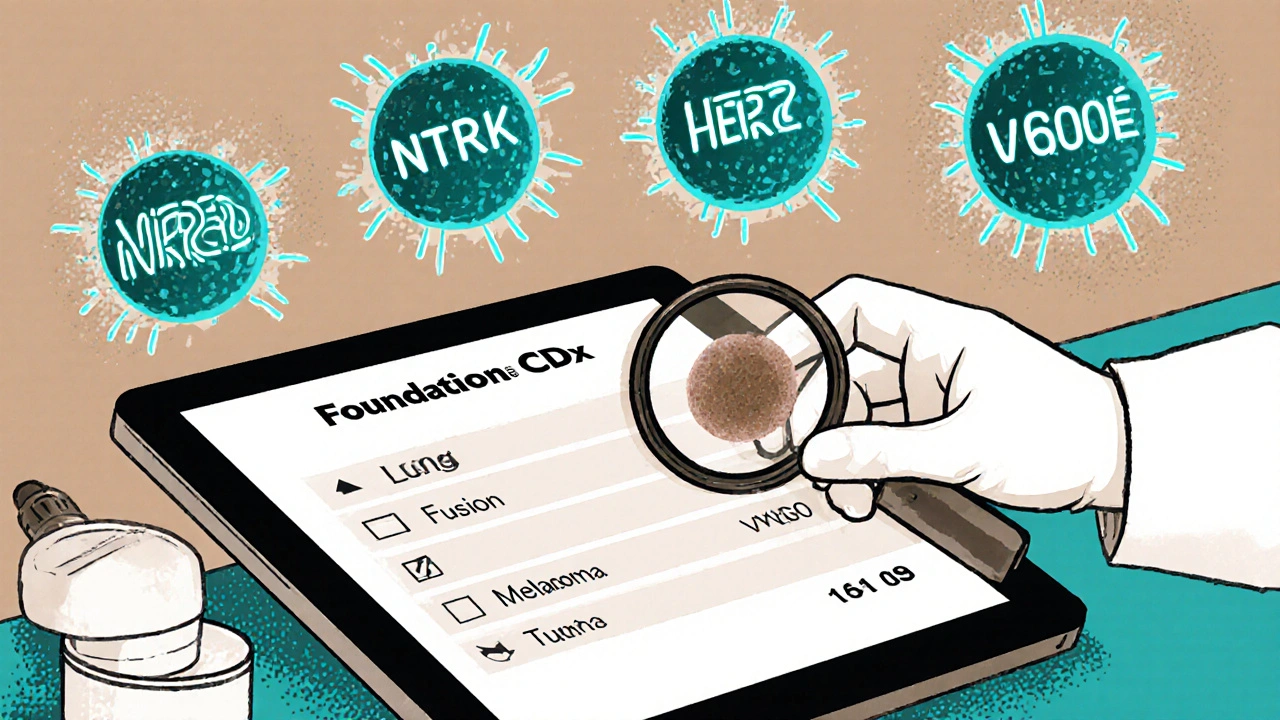
You can’t use targeted therapy unless you know what you’re targeting. That’s why genomic testing - usually through next-generation sequencing (NGS) - is now standard for advanced cancers.
Tests like FoundationOne CDx or MSK-IMPACT scan 300 to 500 cancer-related genes in a single sample. They look for mutations, fusions, and other alterations that might make a tumor vulnerable to a specific drug. The test needs as little as 20 nanograms of DNA from a tumor biopsy, and results typically take two to three weeks.
But here’s the catch: not every tumor has a targetable mutation. Only about 13.8% of cancer patients have a match for an approved targeted therapy, according to AACR Project GENIE. And even when a match is found, the mutation might be too rare or too complex to treat.
And then there’s the problem of variants of unknown significance - changes in the DNA that we see often but don’t yet understand. These make up 20-30% of test results and can leave doctors and patients stuck in uncertainty.
Real Results: Survival and Quality of Life
The numbers speak for themselves. In EGFR-mutant lung cancer, osimertinib extends progression-free survival to nearly 19 months - almost double what chemotherapy achieves. For melanoma with BRAF mutations, combination targeted therapies can shrink tumors in over 70% of patients.
But beyond survival, patients report better quality of life. One patient with stage IV lung cancer wrote on a cancer forum: “After starting osimertinib, my tumor shrank 80% in eight weeks. No vomiting, no hair loss, no constant fatigue. I was able to go back to work.”
A 2023 survey of 1,200 patients found that 68% of those on targeted therapies felt they could manage daily life better than those on chemotherapy. Side effects are different - often skin rashes, diarrhea, or high blood pressure - but they’re usually less severe than the nausea, low blood counts, and exhaustion caused by chemo.
Grade 3-4 side effects (the serious ones) occur in 15-30% of targeted therapy patients - compared to 50-70% with traditional chemotherapy.
The Hard Truth: Limitations and Challenges
Targeted therapy isn’t a magic bullet. It has serious limitations.
First, resistance almost always develops. In 70-90% of cases, the cancer finds a way around the drug - a new mutation, a backup pathway, or even a change in the tumor’s environment. That’s why many patients eventually need a new drug or combination.
Second, cost is a huge barrier. A single month of targeted therapy can cost $15,000 to $30,000. Insurance often denies coverage, especially for drugs used off-label. One Reddit user shared: “My NTRK fusion makes me eligible for larotrectinib - 75% response rate - but my insurance said it’s ‘not standard for my cancer type.’”
Third, access is uneven. In the U.S., 65% of advanced cancer patients get genomic testing. In Europe, it’s 22%. In parts of Asia, it’s below 8%. Even in the U.S., only 42% of community oncology practices can offer comprehensive testing. Many patients never get tested at all.
And then there’s the issue of who benefits. Most clinical trials have historically included mostly white patients. As a result, some mutations are better understood in certain populations than others. The NCI’s RESPOND initiative is trying to fix that, but progress is slow.
What’s Next? The Future of Precision Oncology
The field is moving fast. Liquid biopsies - blood tests that detect tumor DNA floating in the bloodstream - are now FDA-approved. These can track how a tumor is changing in real time, often spotting resistance months before a scan shows it.
Researchers are also exploring combination therapies: targeting both the cancer cell and its environment. For example, pairing a drug that blocks a mutation with one that boosts the immune system. Early trials are promising.
Artificial intelligence is helping too. IBM Watson for Oncology matched molecular tumor board recommendations with 93% accuracy in a 2024 study. That could help smaller hospitals without specialists make better decisions.
By 2030, experts predict that 40% of cancer patients will receive some form of biomarker-directed therapy. But that future only works if we fix access, reduce costs, and make sure no one is left behind because of where they live or how much money they have.
What Patients Should Ask Their Doctors
If you or someone you know has advanced cancer, here are five questions to ask:
- Has my tumor been tested for genomic alterations? If not, can we do it?
- Are there any approved targeted therapies for my specific mutation?
- Is there a clinical trial I might qualify for based on my tumor’s genetics?
- What are the costs, and will my insurance cover the test and treatment?
- Can you refer me to a molecular tumor board or genetic counselor?
Don’t assume your oncologist knows everything. Many community doctors are still catching up. Advocate for testing. Ask for a second opinion if needed. Your tumor’s DNA holds the key - and you have the right to see it.
Final Thoughts
Targeted therapy is not the end of cancer treatment. But it’s the most significant shift since chemotherapy. It turns cancer from a one-size-fits-all disease into something that can be understood, mapped, and matched with the right drug. For some, it’s turned a death sentence into a chronic condition. For others, it’s buying time - and quality time - when none was expected.
The challenge now isn’t just science. It’s fairness. It’s access. It’s making sure that the next breakthrough doesn’t just help those who can afford it, but everyone who needs it.
How is targeted therapy different from chemotherapy?
Chemotherapy attacks all rapidly dividing cells - cancerous and healthy - causing widespread side effects like hair loss, nausea, and low blood counts. Targeted therapy, by contrast, focuses only on specific genetic changes in cancer cells. It’s more precise, often has fewer severe side effects, and works only if the tumor has the right mutation.
Do all cancer patients qualify for targeted therapy?
No. Only about 10-15% of solid tumors have currently actionable genetic targets. For some cancers, like melanoma or lung cancer, the rate is higher - up to 30% in certain subtypes. But for others, like pancreatic or ovarian cancer, options are still very limited. Genomic testing is required to find out if a patient qualifies.
How long does genomic testing take?
Most comprehensive tests, like FoundationOne CDx or MSK-IMPACT, take 14 to 21 days from the time the biopsy is received by the lab. Some faster tests can deliver results in 7-10 days, but they often analyze fewer genes. Time matters - delays can impact treatment decisions.
What if my test shows a mutation but no approved drug exists?
That’s common. About 30% of mutations found are not yet matched to a drug. In those cases, doctors may consider off-label use of a drug approved for another cancer type, or recommend a clinical trial. Some patients with rare mutations, like NTRK fusions, can access drugs like larotrectinib even if their cancer type isn’t listed on the label - because the drug works based on the mutation, not the tumor location.
Why are targeted therapies so expensive?
Developing a targeted drug requires deep genetic research, complex clinical trials focused on small patient groups, and specialized manufacturing. Because these drugs are designed for smaller populations, companies recover costs from fewer patients. A single month can cost $15,000-$30,000. Insurance often requires prior authorization, and denials are common - especially for off-label use.



19 Comments
Jenny Lee
November 16 2025This is life-changing stuff. I watched my mom go through chemo - the vomiting, the hair loss, the exhaustion - and now seeing targeted therapy work? It’s like comparing a sledgehammer to a scalpel.
Evan Brady
November 18 2025Let’s be real - targeted therapy isn’t magic, but it’s the closest thing we’ve had since penicillin. The fact that a drug can work across tissue types - lung, colon, thyroid - if it hits NTRK? That’s not just science. That’s a paradigm shift. And yes, the cost is insane, but imagine if we treated cancer like we treat heart disease: early detection, personalized meds, and insurance that actually covers it. We’re not far off.
The real win? Quality of life. My cousin on osimertinib went from bedridden to hiking weekends. No wig. No IV bags. Just pills and progress.
And yeah, resistance happens - tumors are sneaky bastards - but liquid biopsies are catching mutations before they even show up on scans. We’re moving from reactive to predictive medicine. That’s huge.
Shravan Jain
November 18 202513.8% match rate? That’s a scam. They’re selling hope to the desperate while charging $25k/month. This isn’t medicine - it’s a pharmaceutical Ponzi scheme. And don’t get me started on how they cherry-pick trial participants. If you’re not a wealthy white male, good luck getting tested.
Alex Boozan
November 20 2025Targeted therapy relies on NGS - next-generation sequencing - which requires high-fidelity DNA extraction, variant calling via GATK pipelines, and annotation against ClinVar/OMIM databases. Most community hospitals lack the bioinformatics infrastructure. This isn’t a treatment gap - it’s a systemic failure in translational infrastructure.
mithun mohanta
November 21 2025Oh wow, so now we’re treating cancer based on DNA? Like, literally… genes? I mean, I knew cancer was bad, but I didn’t realize we were playing God with CRISPR now… wait, is this what they mean by ‘precision oncology’? I feel like I’m in a sci-fi movie. Also, $30k/month?! My rent is $1200. I think I’ll just pray.
Premanka Goswami
November 22 2025Who really benefits from this? Big Pharma. The government. The oncologists who get kickbacks from drug reps. The patients? They’re guinea pigs in a $$$ experiment. And don’t tell me about ‘clinical trials’ - they’re just marketing tools to get FDA approval before the side effects kill half the subjects. Remember Vioxx? This is the same playbook.
Kevin Jones
November 23 2025It’s not about the drug. It’s about the epistemology. We’ve moved from organ-based taxonomy to molecular ontology. Cancer is no longer a location - it’s a signature. That’s a Copernican revolution in medicine. But we’re still stuck in the Ptolemaic model of healthcare: profit-driven, fragmented, and unjust.
Brandon Lowi
November 24 2025They say ‘targeted therapy’ - but who’s doing the targeting? The same people who told us cigarettes were safe. The same people who patented the polio vaccine and then sold it to the highest bidder. This isn’t progress - it’s corporate control dressed up in lab coats. And don’t think for a second they’re not tracking your DNA for insurance redlining.
Alexis Paredes Gallego
November 24 2025So let me get this straight - we’re spending billions on pills that only work for 14% of people, while the VA can’t even get veterans their pain meds? And you call this progress? This is the American healthcare system in a nutshell: brilliant science, broken ethics, and a billion-dollar circus for the rich. I’m not mad - I’m just disappointed.
Ram tech
November 25 2025Genomic testing takes 3 weeks? That’s ridiculous. My cousin had lung cancer and waited 5 weeks. By then, it was stage 4. They should just give the drugs to everyone - if it doesn’t work, they’ll know. Why make people wait to die?
Richard Couron
November 25 2025They’re lying. Targeted therapy? Nah. It’s all part of the globalist agenda to control the population. Chemotherapy kills you fast - targeted therapy kills you slow while they harvest your DNA for the biometric database. You think they care about your survival? They care about your genome. You’re not a patient - you’re a data point.
steffi walsh
November 27 2025My sister’s on a targeted drug for HER2+ breast cancer. She’s back to painting. She’s laughing again. I don’t care how much it costs - this is worth every penny. If we can make this accessible, we owe it to every person who’s ever lost someone to chemo.
Erica Lundy
November 28 2025The moral imperative here is not merely technological, but ontological: if we possess the capacity to map and intervene upon the molecular architecture of disease, then to withhold such knowledge - or to ration it by wealth - constitutes a profound ethical failure. The body, once a vessel of fate, is now a text to be interpreted; to deny its decipherment is to deny dignity.
Holly Powell
November 28 2025Let’s not romanticize this. Most of these drugs extend life by weeks, not years. The data is cherry-picked. The ‘quality of life’ surveys? Funded by pharma. And the ‘rare mutations’? They’re marketing hooks to justify billion-dollar price tags. This isn’t medicine - it’s monetized hope.
Joshua Casella
November 29 2025Hey, I’m a community oncology nurse - we don’t have NGS here. But I’ve seen patients get tested at academic centers and come back with answers. It’s not perfect, but it’s better than guessing. If you’re reading this and your doc hasn’t mentioned genomic testing - ask. Don’t wait. Your DNA doesn’t care about your zip code.
Saket Sharma
November 30 2025They say ‘tissue-agnostic’ - but that’s just corporate speak for ‘we found one mutation and we’re going to sell it to every cancer type we can.’ It’s not innovation - it’s repackaging. And the real winners? The lawyers who drafted the off-label prescribing loopholes.
Emanuel Jalba
December 2 2025God bless science 🙏 But who’s paying for it? The middle class? The poor? The uninsured? This isn’t healing - it’s exploitation. I saw a kid with NTRK fusion cry because his insurance denied it. He’s 12. His mom works two jobs. This isn’t medicine. This is a crime.
Leilani O'Neill
December 3 2025Targeted therapy? More like targeted profit. If you’re not white, wealthy, and well-connected, you’re just a statistic in their quarterly report. They don’t want to cure cancer - they want to make it a lifetime subscription.
Riohlo (Or Rio) Marie
December 3 2025It’s beautiful, isn’t it? The way our cells whisper their secrets in nucleotides - and now we’re learning to listen. But the tragedy isn’t the cost - it’s that we’re still treating this like a luxury. The future isn’t just personalized medicine. It’s human justice. And right now? We’re failing.