Antidepressants: Types and Safety Profiles for Patients
When you're struggling with depression or anxiety, the idea of taking an antidepressant can feel like a lifeline-or a leap into the unknown. You’ve heard they help, but what do they actually do? And more importantly, what might they do to you? Not all antidepressants are the same. Some work faster. Some cause fewer side effects. Some can be dangerous if you’re not careful. This isn’t about marketing. It’s about real people, real risks, and real choices.
How Antidepressants Work (And Why They Don’t Work the Same for Everyone)
Antidepressants don’t fix your mood like a light switch. They don’t make you happy. They help your brain regain the ability to regulate emotions, sleep, and energy. Most target neurotransmitters-chemical messengers like serotonin, norepinephrine, and dopamine-that get out of balance in depression.
The most common type today is the SSRI-selective serotonin reuptake inhibitor. These include sertraline (Zoloft), escitalopram (Lexapro), and fluoxetine (Prozac). They block serotonin from being reabsorbed too quickly, leaving more of it available in the brain. SSRIs are usually the first choice because they’re safer than older drugs. They don’t cause dangerous heart rhythms or require strict diets like the older options.
Then there are SNRIs-serotonin-norepinephrine reuptake inhibitors. Venlafaxine (Effexor) and duloxetine (Cymbalta) affect both serotonin and norepinephrine. These are often used when SSRIs don’t help enough, or if fatigue and low energy are major symptoms. They can be more energizing but also carry a slightly higher risk of raising blood pressure.
Then there’s bupropion (Wellbutrin), an atypical antidepressant. It doesn’t touch serotonin much. Instead, it boosts dopamine and norepinephrine. That’s why it’s often chosen for people who struggle with low motivation or who’ve had sexual side effects from other meds. It’s also less likely to cause weight gain.
The older drugs-tricyclics (like amitriptyline) and MAOIs (like phenelzine)-are still used, but rarely as a first step. Tricyclics can cause dry mouth, dizziness, and heart issues. MAOIs require you to avoid aged cheeses, cured meats, and certain wines. One wrong food can spike your blood pressure dangerously. These are usually only tried after other options fail.
What You’ll Likely Experience-Side Effects That Actually Happen
Most people expect antidepressants to cause nausea or drowsiness. But the reality is messier. About 1 in 5 people feel sick to their stomach in the first week. For many, it fades. For others, it sticks around. Weight gain is another big one. Half of long-term users gain weight-sometimes 10 pounds or more. It’s not just about appetite. The medication changes how your body stores fat.
Sexual side effects are the most underreported issue. Up to 56% of people on SSRIs and SNRIs report problems: low desire, trouble getting aroused, delayed or absent orgasm. Many never tell their doctor because they think it’s normal. It’s not. And it’s not always permanent. Switching to bupropion or adding a low dose of another drug like buspirone can help.
Then there’s emotional blunting. Some people say they feel ‘numb.’ They’re not crying, but they’re not laughing either. They feel like they’re watching life through glass. This isn’t just ‘being calm.’ It’s a loss of emotional range. Studies show 64.5% of long-term users report this. It’s not listed on most medication guides. But if you’re feeling this way, it’s real-and worth talking about.
And then there’s the worst-case scenario: increased suicidal thoughts. The FDA requires a black box warning for people under 25. About 1 in 6 young adults starting antidepressants report a spike in suicidal thinking in the first few weeks. That’s why the first month is critical. If you or someone you love starts feeling worse, not better, don’t wait. Call your doctor immediately.

The Long Game: What Happens After Months or Years?
Antidepressants aren’t meant to be a quick fix. They take 4 to 6 weeks to show real effects. Full benefit can take 12 weeks. That’s why people give up too soon. But if you stick with it, the payoff can be huge. For people with moderate to severe depression, antidepressants reduce symptoms by about 50% more than placebo, according to a major 2018 study in The Lancet.
But what happens after you’ve been on them for a year? Two years? A 2016 study in the PMC found that 73.5% of long-term users experienced withdrawal symptoms when they tried to quit. That’s not addiction. It’s your brain adapting. Stopping suddenly can cause dizziness, electric-shock feelings in your head, anxiety, and flu-like symptoms. This is called discontinuation syndrome. Some drugs, like paroxetine, are notorious for this. Others, like fluoxetine, have a longer half-life and are easier to taper off.
Long-term use also increases risks of bone thinning, low sodium levels (hyponatremia), and even type 2 diabetes. These aren’t common, but they’re real. If you’ve been on antidepressants for more than two years, ask your doctor about bone density scans and regular blood tests.
And yet-stopping isn’t always the answer. Studies show that if you stop too soon, your chance of relapse jumps from 20-30% to 50-60%. The National Institute for Health and Care Excellence recommends staying on treatment for at least 6 to 9 months after you feel better. For people with recurring depression, long-term use may be necessary.
Who Should Be Careful? Pregnancy, Age, and Drug Interactions
If you’re pregnant or planning to be, antidepressants need careful thought. Using them in the third trimester can lead to jitteriness, low blood sugar, or breathing trouble in newborns. But not taking them can also be risky. Severe depression during pregnancy increases the chance of preterm birth and low birth weight. The American College of Obstetricians and Gynecologists now says the decision should be individualized. Sertraline and citalopram are often preferred because they have the most safety data.
Older adults are more sensitive to side effects. Low sodium levels are a big risk. Dizziness can lead to falls. Some antidepressants interact dangerously with common heart or blood pressure meds. Always tell your doctor what else you’re taking-even over-the-counter painkillers or herbal supplements like St. John’s Wort.
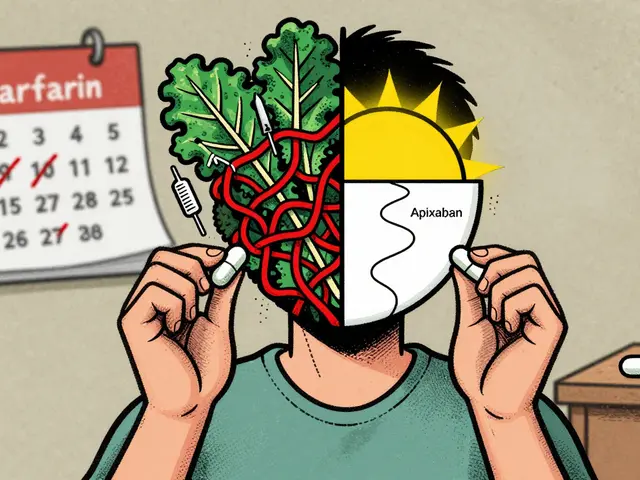
And here’s something rarely discussed: drug interactions. Most antidepressants are broken down by the liver using the same enzyme system-CYP450. That means if you’re on a statin, a blood thinner, or even some antibiotics, your antidepressant levels can spike or drop. This isn’t theoretical. It’s why pharmacists now check for these interactions before filling prescriptions.
Finding the Right Fit-Trial, Error, and Patience
There’s no magic pill. No single antidepressant works best for everyone. A 2022 survey on PatientsLikeMe showed 68% of users felt better, but 79% had at least one side effect. Most people try two or three different meds before finding one that works without crushing them.
Don’t get discouraged if the first one doesn’t fit. It’s not you. It’s the medication. The process is frustrating, but it’s normal. Some people find relief with sertraline. Others need venlafaxine. A few do best with bupropion. One Reddit user wrote: ‘It took me four antidepressants over 18 months. The fifth one? Finally, I felt like myself again.’
And here’s the key: combine meds with therapy. The American Psychiatric Association says neither antidepressants nor talk therapy alone work as well as both together. CBT-cognitive behavioral therapy-helps you change negative thought patterns. That’s what keeps depression from coming back.
What to Do Next
If you’re considering antidepressants:
- Ask your doctor: ‘What’s the evidence this drug works for my symptoms?’
- Request a full side effect list-not just the pamphlet. Know what’s likely and what’s rare.
- Start low. Many side effects fade if you begin with a low dose and increase slowly.
- Track your mood and side effects weekly. Use a free app or a notebook.
- Don’t stop suddenly. If you want to quit, plan it with your doctor over weeks or months.
- Ask about alternatives. For mild depression, exercise, CBT, or light therapy can be just as effective-with fewer risks.
If you’re already on one:
- Are you feeling better-or just less bad?
- Are the side effects worth it?
- Have you talked to your doctor about emotional blunting or sexual problems?
- Have you had a blood test or bone density scan in the last two years?
Antidepressants aren’t perfect. But for many, they’re the only thing that brings back the ability to get out of bed, to care again, to live. The goal isn’t to be ‘fixed.’ It’s to be functional. To feel human again. That’s worth the effort.
How long do antidepressants take to start working?
Most people start noticing small improvements after 2 to 4 weeks, but full benefits usually take 6 to 12 weeks. If you don’t feel any change after 8 weeks, talk to your doctor. It doesn’t mean the drug won’t work-it just might not be the right one for you.
Can antidepressants make anxiety worse at first?
Yes. Especially in the first 1 to 2 weeks, some people feel more anxious, jittery, or even panicky. This is common with SSRIs and SNRIs. It usually passes. But if it’s severe or you have thoughts of self-harm, call your doctor right away. Don’t wait.
Is weight gain from antidepressants permanent?
Not always. Many people gain 5 to 10 pounds in the first few months, then stabilize. Some lose it after switching medications. Bupropion and vortioxetine are less likely to cause weight gain. If weight becomes a concern, ask about adding a low dose of topiramate or switching to a different class. Lifestyle changes help too-regular movement and mindful eating make a big difference.
Do antidepressants cause addiction?
No. Antidepressants don’t cause addiction like opioids or benzodiazepines. You won’t crave them or need higher doses to get the same effect. But your body adapts to them. Stopping suddenly can cause withdrawal symptoms-dizziness, brain zaps, nausea-which is why you must taper off slowly under medical supervision.
Are generic antidepressants as good as brand names?
Yes. Generic versions of sertraline, citalopram, and fluoxetine are just as effective as their brand-name versions. The FDA requires them to have the same active ingredient, strength, and absorption rate. The only differences are in inactive ingredients like fillers, which rarely affect how the drug works. Save money-ask your pharmacist for the generic.
What should I do if I miss a dose?
If you miss one dose, take it as soon as you remember-if it’s within a few hours of your usual time. If it’s close to your next dose, skip it. Don’t double up. Missing one dose won’t ruin your progress, but frequent missed doses can cause withdrawal symptoms or reduce effectiveness. Set phone reminders or use a pill organizer.
Can I drink alcohol while taking antidepressants?
It’s not recommended. Alcohol can worsen depression and anxiety. It can also increase drowsiness, dizziness, and impair your judgment. With some antidepressants, like MAOIs, alcohol can cause dangerous spikes in blood pressure. Even with SSRIs, mixing alcohol and meds reduces your ability to cope with stress. If you choose to drink, keep it minimal-and talk to your doctor first.
Are there natural alternatives to antidepressants?
For mild depression, yes. Regular exercise, sunlight exposure, cognitive behavioral therapy, and omega-3 supplements have been shown to help. But for moderate to severe depression, these alone aren’t enough. Don’t replace prescribed meds with supplements without medical advice. St. John’s Wort, for example, can interfere with birth control and other medications. It’s not safer-it’s just unregulated.




11 Comments
Mark Kahn
November 20 2025Been on sertraline for 3 years now. First 6 weeks were rough - nausea, jittery as a caffeine addict, but then… boom. Like someone turned the volume down on the static in my head. Not ‘happy’ - just able to breathe again. Don’t let the side effects scare you off. Talk to your doc, start low, and give it time.
Daisy L
November 21 2025EMOTIONAL BLUNTING?! Oh my GOD YES. I thought I was just ‘getting older’ - turns out I was just numb. No tears at funerals. No laughter at dumb memes. Just… flat. Switched to bupropion and it’s like my soul got Wi-Fi again. Why isn’t this on the FDA pamphlet???
Anne Nylander
November 23 2025you guys are so overthinking this. just take the pill. walk outside. drink water. talk to someone. it’s not magic but it helps. i cried the first week, then i laughed again. that’s all that matters.
Leo Tamisch
November 24 2025How quaint. You all treat SSRIs like a spiritual awakening. Let’s be clear: these are neurochemical band-aids for a society that’s too lazy to fix systemic trauma. You’re not ‘finding yourself’ - you’re chemically suppressing existential dread because capitalism doesn’t pay you to feel. 🤷♂️
Franck Emma
November 26 2025I almost died the first time I tried to quit. Brain zaps. Like my skull was being rewired with a Tesla coil. Never again. I’m on Lexapro for life. I’d rather be numb than feel that again.
Noah Fitzsimmons
November 27 2025Wow. So you’re telling me people are actually surprised antidepressants have side effects? Did you think you were injecting fairy dust? Also, who let you post a 10,000-word essay without a single citation? 🙄
Eliza Oakes
November 27 2025Ugh. Another ‘antidepressants are life-changing’ post. What about the people who tried 7 meds and still can’t get out of bed? Or the ones who gained 50 lbs and lost their marriage? This isn’t a TED Talk. It’s a pharmaceutical sales pitch dressed in clinical language.
Corra Hathaway
November 29 2025Y’all are so brave for sharing. 💪 I started on citalopram after my mom passed and thought I’d never smile again. Now I dance in the kitchen while making oatmeal. It’s not perfect - I still have bad days - but I’m here. And that’s enough. 🌞
Pravin Manani
November 29 2025Let’s unpack the pharmacodynamics: SSRIs inhibit SERT with >90% binding affinity, but downstream neuroplasticity changes - BDNF upregulation, hippocampal neurogenesis - take weeks to manifest. That’s why efficacy lags. Meanwhile, SNRIs’ dual reuptake blockade increases noradrenergic tone, which explains their efficacy in fatigue-dominant phenotypes. But here’s the kicker: CYP2D6 polymorphisms cause 15-30% of patients to be poor metabolizers, leading to toxic accumulation. Always check pharmacogenomic panels before initiating therapy. Also - emotional blunting? That’s not a side effect. That’s the dopamine system being chronically downregulated. We need longitudinal fMRI studies. This isn’t medicine. It’s trial-and-error alchemy.
Clifford Temple
December 1 2025Why are we letting Big Pharma tell us how to feel? In my country, we don’t take pills for sadness - we work harder. Build something. Get outside. Stop being weak. This whole post is a soft, American luxury. You don’t need serotonin - you need discipline.
Leo Tamisch
December 2 2025Oh, so now we’re talking about CYP2D6? 🧠👏 How poetic. The man who called SSRIs ‘band-aids’ just turned into a pharmacology professor. You’re not a researcher, Leo - you’re just trying to sound smart. Also, ‘neuroplasticity’? Cute. Next you’ll be quoting Heidegger on SSRI-induced anhedonia.