Why Doctors Recommend Generic Medications - And Why Patients Still Hesitate
Every year, over 90% of prescriptions filled in the U.S. are for generic drugs. Yet, if you walk into a doctor’s office and ask for the cheapest option, you’ll still hear, "I’m prescribing the brand-name version." Why? It’s not about science. It’s about psychology.
The Truth About Generic Drugs
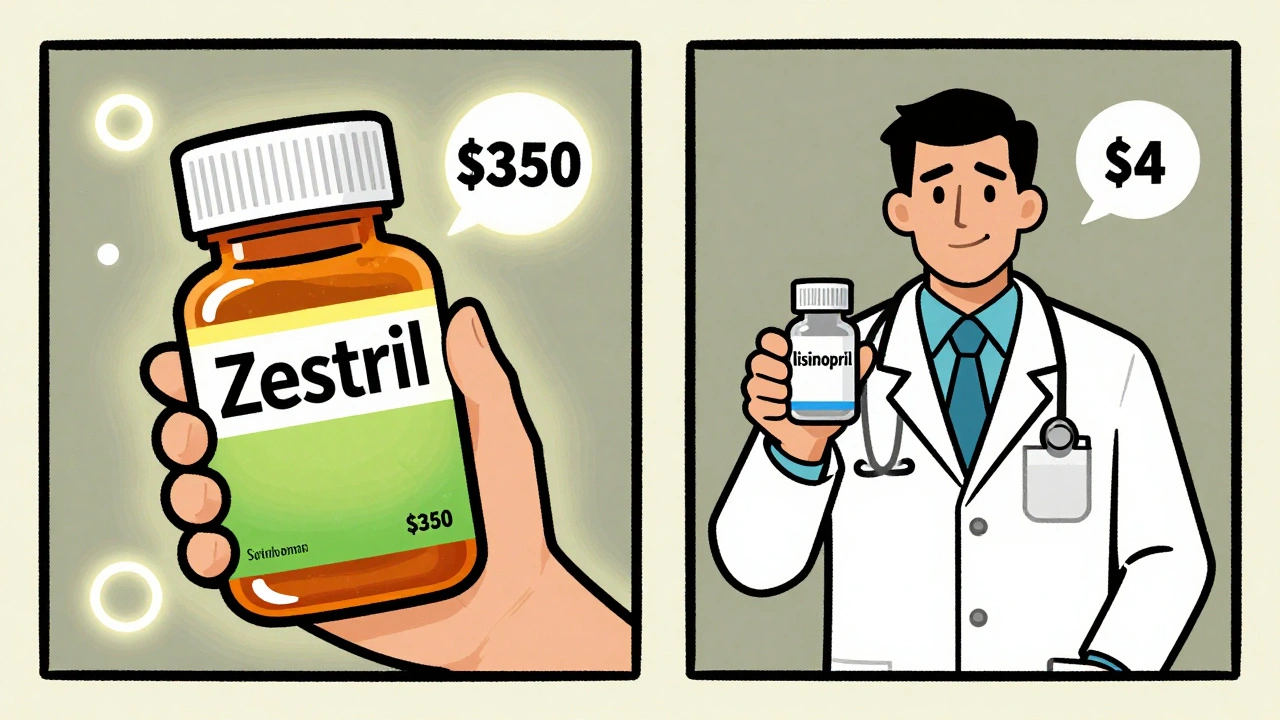
Generic drugs aren’t cheaper because they’re weaker. They’re cheaper because they don’t need to spend millions on advertising, fancy packaging, or patent lawsuits. By law, a generic must contain the same active ingredient, in the same strength, and deliver it the same way as the brand-name version. The FDA requires bioequivalence testing - meaning the generic must release the drug into your bloodstream at the same rate and amount as the brand. The acceptable range? 80% to 125% of the brand’s performance. That’s not a guess. That’s science.Take lisinopril, a common blood pressure pill. The brand-name version, Zestril, costs around $350 a month without insurance. The generic? $4 at Walmart. Same molecule. Same effect. Same side effects. The only difference? The color of the pill and the name on the bottle.
The American College of Physicians has been clear since 2016: prescribe generics when possible. Their review of dozens of studies found that patients on generics are 6% more likely to keep taking their medication. That’s not a small boost. It means fewer hospital visits, fewer complications, and lower overall costs. For someone managing diabetes or high blood pressure, that 6% can mean the difference between staying healthy and ending up in the ER.
Why Do Doctors Still Prescribe Brands?
You’d think doctors, trained in evidence-based medicine, would always choose the cheaper, equally effective option. But they don’t. And it’s not because they’re being paid by drug companies - at least not directly.Here’s what actually happens: doctors are human. They’ve been trained for years to recognize brand names. Zoloft. Lipitor. Advil. These aren’t just drugs - they’re familiar landmarks in their minds. When a patient walks in with anxiety, the doctor doesn’t think, "I need to prescribe sertraline." They think, "I need to prescribe Zoloft." It’s automatic.
Then there’s the fear of blame. If a patient’s blood pressure doesn’t drop after switching to a generic, who gets called? The doctor. Even if the generic is identical, the patient blames the switch. "I switched to the cheap one and now I feel worse." That’s not always true - but it’s how it feels. And in medicine, perception often outweighs data.
Studies show that primary care doctors prescribe generics more often than specialists. Why? Because they see the long-term results. They’re the ones managing hypertension, diabetes, cholesterol - conditions where sticking to the medication matters more than the brand. Hospital doctors? They’re focused on acute care. If a patient’s heart attack came after a drug interaction, they’re more likely to stick with what they know.
Patients Don’t Trust Generics - Even When They Should
You’ve probably heard it: "The generic doesn’t work like the real thing." Or, "I tried it and my headaches got worse."The FDA’s own research found that patients believe generics are less effective, even when they’re not. Why? Because they look different. A blue pill becomes white. A capsule becomes a tablet. A pill with "Pfizer" on it becomes one with "Watson." Your brain doesn’t process that as "same medicine." It processes it as "different. Something changed. Something’s wrong."
One internist in Birmingham told me about a patient who refused generic metformin after switching from Glucophage. "I’ve been on this for 12 years," the patient said. "I know how this one makes me feel. This one? It’s not the same." The patient wasn’t wrong - they just didn’t know the active ingredient hadn’t changed. The side effects? Identical. The effectiveness? Identical. But the pill looked different. And that was enough.
Even worse, some patients assume generics are "old" or "low quality." But here’s the truth: the same factories that make brand-name drugs often make the generics. The FDA inspects them all the same way. In 2022, they inspected nearly 1,500 generic drug facilities - domestic and foreign - with the same standards as brand-name plants.

The Real Problem: Inertia, Not Evidence
The data is clear. Generics work. They’re safe. They save money. So why isn’t everyone using them?Because change is hard - even when it’s obvious.
Doctors don’t get enough training on generics. A 2016 study found that 96% of Saudi doctors said they knew generics were effective - but only 16% said they’d use them in every case. Why? Because they never learned how to explain the switch to patients. They never learned how to handle the resistance.
And patients? They’re bombarded with ads. "Brand-name. Trusted. Proven." The message is everywhere. Meanwhile, generics have no marketing. No commercials. No billboards. Just a price tag.
The FDA tried to fix this with their "Look Alike Sound Alike" program - reducing confusion between similarly named drugs. It cut patient errors by 37%. But it didn’t fix the deeper issue: the emotional connection people have to brand names.
When Generics *Shouldn’t* Be Used
There are exceptions. Not because generics are bad - but because the margin for error is razor-thin.The FDA keeps a list of 15 drugs where even tiny differences in blood levels can cause serious problems. Think seizure meds like phenytoin, thyroid meds like levothyroxine, and blood thinners like warfarin. For these, doctors often stick with brand-name versions - not because generics are unsafe, but because the body is less forgiving. Small changes in absorption can mean the difference between control and crisis.
Even then, many of these generics are perfectly fine. The issue isn’t the drug. It’s the patient’s history. If someone’s been stable on a brand for years, switching might not be worth the risk - even if the science says it’s safe.
And then there are complex drugs - inhalers, topical creams, injectables. These aren’t just pills. Their delivery matters. A generic inhaler might have the same active ingredient, but if the nozzle feels different or the puff is weaker, patients might not inhale properly. That’s not the drug’s fault. It’s the design.

What You Can Do
If you’re on a brand-name drug and you’re paying hundreds a month, ask your doctor: "Is there a generic?" Don’t be afraid. You’re not being cheap. You’re being smart.If your pharmacist switches your medication to a generic without asking - and you feel different - speak up. Tell your doctor. It’s not about distrust. It’s about awareness.
And if you’re a doctor? Don’t assume your patient knows the difference. Say it clearly: "This generic has the same active ingredient as the brand. It’s just cheaper. I’ve prescribed it to hundreds of patients. It works the same way."
That simple sentence - "It works the same way" - changes everything.
The Bigger Picture
The global generic drug market is worth over $400 billion and growing. By 2030, generics will still make up over 85% of all prescriptions. The future isn’t about brand names. It’s about access. About affordability. About making sure people don’t skip their meds because they can’t afford them.But until we fix the psychology - until we break the myth that "brand = better" - we’ll keep wasting billions. Patients will keep refusing generics. Doctors will keep prescribing brands. And the system will keep paying the price.
The science is settled. The cost savings are real. The only thing left to change? Our minds.



9 Comments
Dematteo Lasonya
December 4 2025My grandma switched from Lipitor to generic atorvastatin last year and her cholesterol dropped even more. She didn’t even notice the pill looked different. Sometimes the real magic is just sticking with the treatment, not the label.
Jessica Baydowicz
December 5 2025OMG YES. I used to pay $200 a month for my diabetes meds. Switched to generic metformin? $5. I started actually taking it regularly. Life changed. No joke. 💪
Gillian Watson
December 6 2025In the UK we’ve been on generics for ages and it’s just normal. I think the US obsession with branding spills over into medicine. It’s weird when you think about it. Same chemical, different color. Who cares?
Jordan Wall
December 7 2025Let’s be real - generics are just pharma’s way of monetizing bioequivalence loopholes. The FDA’s 80–125% range is a joke. You’re essentially gambling with your pharmacokinetics. And don’t get me started on the CROs in Hyderabad.
Gareth Storer
December 7 2025So what you’re saying is… doctors are lazy and patients are gullible? Wow. Groundbreaking. 🤡
Pavan Kankala
December 7 2025Generics are a government plot to control the population. They’re cheaper because they’re laced with microchips. You think your blood pressure is stable? Nah. You’re being tracked. Big Pharma + Big Brother = same thing.
Libby Rees
December 8 2025It’s fascinating how deeply we associate identity with objects-even pills. We don’t just take medication; we ritualize it. The color, the shape, the brand name-it becomes part of our healing narrative. When that changes, even if the science says it’s identical, the psyche rebels. It’s not irrational. It’s human.
My father refused generic thyroid medication for years because he believed the ‘blue pill’ was ‘more powerful.’ He didn’t understand that the FDA’s bioequivalence standards were stricter than most consumer product safety rules. He just knew his body felt different. And in medicine, feeling is often the only truth that matters.
Doctors aren’t just prescribing drugs-they’re prescribing familiarity. And for many patients, that’s more valuable than cost savings. It’s not about ignorance. It’s about trust.
When I switched my own blood pressure meds, I noticed a slight change in how I felt. Not because the drug was different-but because I was anxious it might be. I called my doctor. We talked. She explained the equivalence data. I still took the generic. But I didn’t feel better until I stopped thinking about it.
That’s the real barrier: perception, not pharmacology. We need to reframe generics not as ‘cheap alternatives’ but as ‘equivalent choices.’ Language matters. Framing matters.
And yes, the same factories make both. I’ve toured a facility in New Jersey that churns out both brand-name and generic versions on the same line. The only difference? The sticker on the box.
It’s not about quality. It’s about marketing. And we’ve been trained to believe that more expensive means better-even when the numbers say otherwise.
Maybe the solution isn’t more education. Maybe it’s more empathy. Instead of saying ‘it’s the same,’ say ‘I’ve seen this work for hundreds of people like you.’
And if you’re a doctor? Don’t assume your patient knows what ‘bioequivalence’ means. Say it plainly. Say it kindly. Say it like you mean it.
Martyn Stuart
December 9 2025Important note: for drugs like levothyroxine, warfarin, and phenytoin, the FDA does recommend caution-because the therapeutic window is narrow. But even here, many generics are perfectly safe-especially if the patient has been stable on one formulation for months or years. The key is consistency, not brand.
Also: many generic manufacturers are now producing high-quality, AB-rated products that meet or exceed brand standards. The FDA’s 2022 inspection report showed that 98% of generic facilities passed with zero critical violations.
And yes, patients do report feeling ‘different’ after switching-but often, that’s due to the nocebo effect. The mind expects to feel worse, so it does. That’s why doctors need to proactively normalize the switch: ‘This is the same drug, just without the ad budget.’
Finally: if you’re on a brand and your insurance won’t cover it, ask for a prior authorization. Many insurers will cover brand-name drugs if you can prove you’ve tried and failed with generics. Don’t give up!
Shofner Lehto
December 10 2025My sister’s cardiologist switched her from Plavix to generic clopidogrel after she lost her job. She was terrified. He spent 20 minutes explaining it. He showed her the FDA data. He told her he’d prescribed it to 300 patients. She cried. Then she took it. Two years later, she’s fine. No event. No issue. Just a cheaper pill and a smarter system.
It’s not about the drug. It’s about the conversation.