Psoriasis and Psoriatic Arthritis: Understanding the Autoimmune Link Between Skin and Joints
When your skin breaks out in red, scaly patches, it’s easy to think it’s just a cosmetic issue. But if those patches come with stiff, swollen fingers, achy heels, or lower back pain, you’re not just dealing with a skin condition-you’re facing something deeper. Psoriasis and psoriatic arthritis (PsA) are two sides of the same autoimmune coin. One affects your skin, the other your joints, but both stem from the same broken immune response. And if you’ve got one, you’re far more likely to get the other.
What Exactly Is Psoriatic Arthritis?
Psoriatic arthritis isn’t just arthritis that happens to appear in someone with psoriasis. It’s a distinct disease where the immune system attacks healthy tissue-not just in the joints, but in the tendons, nails, and even the spine. About 30% of people with psoriasis will develop PsA, according to the American College of Rheumatology. In most cases, the skin comes first-about 85% of the time. But in 5 to 10% of cases, joint pain starts before any rash shows up. That’s why doctors now look for joint symptoms even if the skin looks fine.
The hallmark signs? Swollen fingers and toes that look like sausages-that’s called dactylitis. It happens in nearly 40% of PsA patients. Then there’s enthesitis, where tendons pull away from the bone, causing pain at the back of the heel or under the foot. Many people mistake this for plantar fasciitis, but if you’ve got psoriasis and this pain, it’s likely PsA.
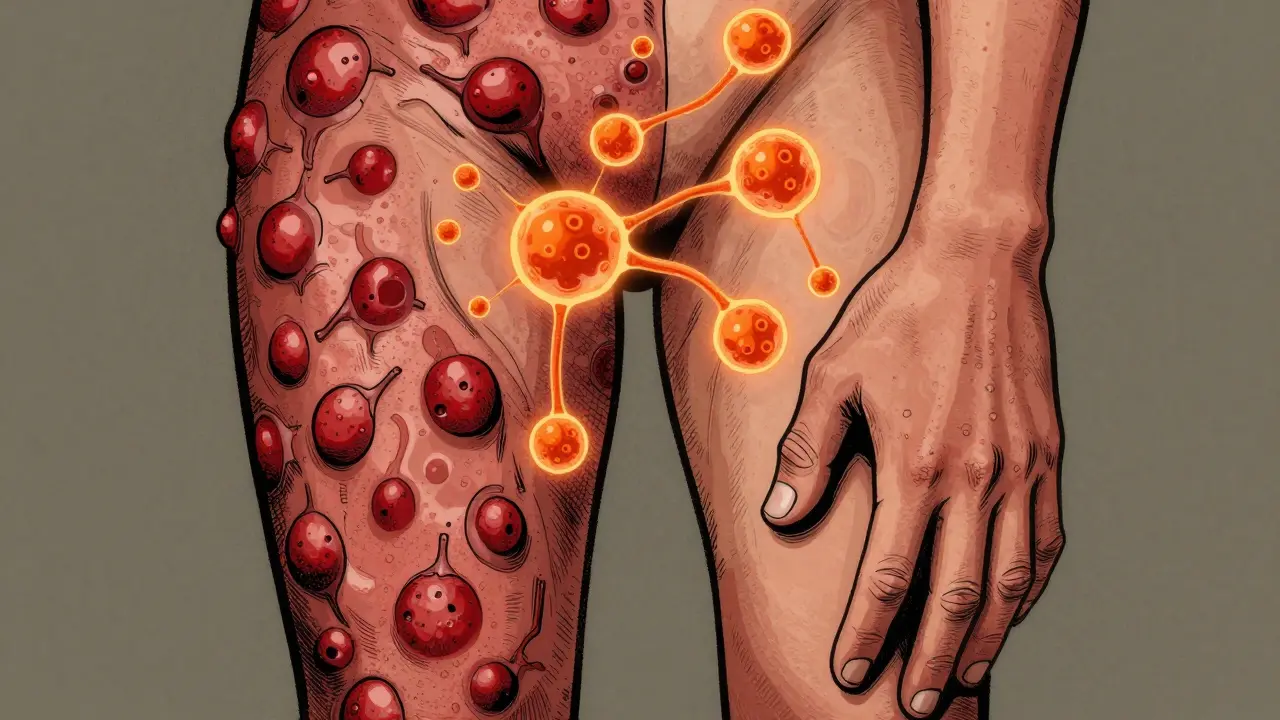
How Your Skin and Joints Are Connected
The link between psoriasis and PsA isn’t random. It’s biological. In both conditions, immune cells-especially T-cells-go rogue. They trigger inflammation in the skin, producing those thick, silvery plaques. The same cells then migrate to the joints, where they attack the lining, causing swelling, pain, and eventually, bone damage.
Genetics play a big role. If you carry certain HLA genes-like HLA-B27, HLA-B38, or HLA-B39-you’re at higher risk. But genes alone don’t cause it. Triggers like stress, infections, injury, or even smoking can turn on the disease in someone genetically predisposed. That’s why two people with psoriasis might never develop joint problems, while another person develops PsA within a year of their first flare.
And here’s something most people don’t realize: your nails tell the story too. Around 80% of PsA patients have nail changes-pitting, ridges, or the nail lifting off the nail bed. If you’ve got psoriasis and suddenly notice your nails looking weird, don’t ignore it. It’s a red flag.
How Doctors Diagnose Psoriatic Arthritis
There’s no single blood test for PsA. Diagnosis relies on a mix of clinical signs, imaging, and a tool called the CASPAR criteria. To meet the threshold, you need at least three points from this checklist:
- Current psoriasis (3 points)
- History of psoriasis (2 points)
- Nail changes (1 point)
- Negative rheumatoid factor (1 point)
- Characteristic bone changes on X-ray (1 point)
So if you have psoriasis, nail pitting, and no rheumatoid factor-that’s already five points. You’ve got PsA.
Doctors also use imaging. X-rays can show bone erosion or that classic “pencil-in-cup” deformity, where bone wears down on one side and grows abnormally on the other. Ultrasound and MRI are even better-they catch inflammation before it turns into permanent damage. Blood tests for CRP and ESR measure general inflammation, but they’re not specific. That’s why a good physical exam matters more than any lab result.
Treatment Isn’t One-Size-Fits-All
For mild joint pain, over-the-counter NSAIDs like ibuprofen can help. But they don’t stop the disease. If your joints are swelling or your skin is worsening, you need stronger tools.
First-line disease-modifying drugs include methotrexate. It’s been around for decades and still works for many. But for moderate to severe cases, biologics are the game-changers. These are targeted drugs that block specific parts of the immune system:
- TNF inhibitors (like adalimumab, etanercept): Best for spine and tendon pain
- IL-17 inhibitors (secukinumab, ixekizumab): Best for skin and nail symptoms
- IL-23 inhibitors (guselkumab, risankizumab): Newer, highly effective for both skin and joints
- JAK inhibitors (tofacitinib, deucravacitinib): Oral pills that work fast
Studies show TNF blockers help 50-60% of patients achieve at least a 20% improvement in symptoms. IL-17 inhibitors often do even better for skin clearance-up to 80% of patients see 75% or more improvement in their plaques.
The goal isn’t just to feel better. It’s to reach minimal disease activity-a real standard doctors now use. That means: no more than one tender or swollen joint, less than 1% of skin affected, pain under 15 out of 100, and no fatigue. If you’re hitting that, your treatment’s working.
The Hidden Dangers: Comorbidities You Can’t Ignore
PsA isn’t just a joint and skin disease. It’s a systemic condition with serious side effects. About half of people with PsA also have metabolic syndrome-high blood pressure, belly fat, insulin resistance, and bad cholesterol. That doubles your risk of heart disease. In fact, your chance of having a heart attack is 43% higher than someone without PsA.
Depression and anxiety are common too. One in three patients struggle with mood disorders. It’s not just because living with chronic pain is hard. Inflammation itself affects brain chemistry. That’s why mental health screening is now part of standard PsA care.
And here’s the scariest stat: people with PsA have a 30-50% higher risk of early death-mostly from heart problems. That’s why managing your blood pressure, cholesterol, and weight isn’t optional. It’s part of your treatment plan.
What’s Next? The Future of PsA Care
Research is moving fast. Scientists are now looking at your gut microbiome. People with PsA have different gut bacteria than those without it. Could probiotics or diet changes help? Early trials are promising.
Biomarkers are also emerging. Blood tests for calprotectin or MMP-3 might soon tell doctors which drug will work best for you-before you even start. That’s precision medicine in action.
By 2027, experts predict 70% of PsA patients will be on biologics or targeted drugs within two years of diagnosis. That’s up from 40% today. Why? Because we now know that early, aggressive treatment stops joint damage before it’s permanent. Waiting until your fingers are deformed is no longer acceptable.
What You Should Do Now
If you have psoriasis and any joint pain, stiffness, or swelling-don’t wait. See a rheumatologist. Don’t let your doctor dismiss it as “just aging” or “overuse.”
If you’ve been diagnosed with PsA:
- Stick to your treatment plan-even when you feel fine
- Get regular heart and metabolic screenings
- Quit smoking if you do
- Maintain a healthy weight
- Track your symptoms: pain levels, skin coverage, fatigue
PsA is not a death sentence. But it demands attention. The sooner you treat it, the less damage it does. And with today’s treatments, many people go on to live full, active lives-without pain, without limits.
Can psoriasis turn into psoriatic arthritis?
Psoriasis doesn’t "turn into" psoriatic arthritis. Both are caused by the same autoimmune process. Having psoriasis increases your risk of developing PsA, but not everyone with psoriasis gets it. About 30% do. The key is watching for joint symptoms-like swelling, stiffness, or pain-and getting checked early.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) typically affects small joints symmetrically-both hands, both knees. PsA is more unpredictable. It can affect just one finger, the spine, or the heels. RA is linked to rheumatoid factor in the blood; PsA is not. Nail changes and enthesitis are common in PsA but rare in RA. Diagnosis relies on different criteria.
Can diet cure psoriatic arthritis?
No diet can cure PsA. But some people find that reducing sugar, processed foods, and alcohol helps lower inflammation. Weight loss, especially if you’re overweight, can significantly improve symptoms. Some studies suggest omega-3s from fish oil and vitamin D may help, but they’re supplements-not replacements-for prescribed treatment.
Do I need to see a dermatologist or a rheumatologist?
You need both. A dermatologist manages your skin and nails. A rheumatologist manages your joints, spine, and overall disease activity. Since PsA affects multiple systems, coordinated care is essential. Many clinics now have combined dermatology-rheumatology teams for this reason.
Can I stop taking my medication if my symptoms improve?
Don’t stop without talking to your doctor. Even if you feel fine, inflammation may still be quietly damaging your joints. Stopping treatment often leads to flare-ups-and sometimes, the drugs stop working as well when restarted. The goal is long-term control, not temporary relief.
Is psoriatic arthritis hereditary?
Yes, genetics play a role. If a close family member has psoriasis or PsA, your risk is higher. But having the genes doesn’t mean you’ll get it. Environmental triggers like stress, infections, or injury are usually needed to start the disease. Family history is a warning sign-not a guarantee.




15 Comments
Kent Peterson
December 15 2025This is just another corporate-sponsored medical propaganda piece. You know what really cures psoriasis? Cutting out gluten, dairy, and sugar. No drug company wants you to know that. I've been symptom-free for 7 years. No biologics. Just discipline.
Evelyn Vélez Mejía
December 16 2025The ontological rupture between skin and joint in this discourse is profoundly revealing. One does not merely 'have' psoriasis; one is constituted by it-a living paradox of autoimmunity wherein the body becomes both perpetrator and victim. The epistemic violence of reductionist medical taxonomy obscures the existential weight borne by those who inhabit this liminal state.
Nishant Desae
December 16 2025I have psoriasis and my knee has been aching for months but my doctor said it's just arthritis from walking too much. I didn't know it could be psoriatic arthritis. This post made me realize I need to see a rheumatologist. Thank you for sharing this. I'm not alone in this. I'm going to book an appointment this week. You're all so brave for sharing your stories.
Pawan Chaudhary
December 18 2025Hey everyone, just wanted to say you're all doing amazing. I was diagnosed with PsA last year and thought my life was over. But with methotrexate and walking every day, I'm back to playing with my kids. It's not easy, but it's worth it. You got this 💪❤️
Linda Caldwell
December 19 2025Stop taking biologics and start lifting weights. That's the real treatment. I lost 40 lbs and my skin cleared. No pills needed.
Anna Giakoumakatou
December 21 2025Ah yes, the sacred text of modern rheumatology: a 3000-word essay on how to monetize chronic illness. How many pharmaceutical reps did this post pay off? The real breakthrough? Not needing to see a doctor at all. Just stop caring. Your immune system will thank you.
Erik J
December 21 2025Interesting. I wonder if the T-cell migration pattern differs between nail-pitting dominant vs. dactylitis-dominant presentations. Has any imaging study tracked that?
BETH VON KAUFFMANN
December 22 2025The CASPAR criteria are outdated. The 2023 EULAR guidelines now emphasize enthesitis scoring and IL-23 pathway biomarkers. Also, calling it 'minimal disease activity' is a PR stunt. It's just 'not actively destroying your joints yet.' And you missed mentioning the gut-joint axis entirely. Pathetic.
Donna Packard
December 24 2025I was diagnosed last year. I didn't know nail changes meant anything. Now I check them every morning. It's scary, but knowing what to look for makes me feel like I have some control.
Jessica Salgado
December 25 2025I cried reading this. Not because I'm sad-but because for the first time, someone described exactly how I feel. The fatigue. The shame when my nails look like that. The fear that my husband will leave me. This isn't just a skin thing. It's my whole life. Thank you for saying it out loud.
Chris Van Horn
December 25 2025You people are all delusional. PsA is a myth invented by Big Pharma to sell $100,000/year drugs. I've had 'psoriasis' since I was 12. No joint pain. No biologics. Just raw apple cider vinegar and willpower. Anyone who takes these drugs is a sheep. You're being manipulated.
Peter Ronai
December 27 2025Let me guess-you got this from a medical blog written by a pharma rep with a PhD in marketing. Real patients don't care about CASPAR criteria. They care about whether they can hold their grandkid. And if you're still on methotrexate in 2025, you're doing it wrong. Biologics are the baseline now. You're 10 years behind.
Michael Whitaker
December 28 2025I appreciate the thoroughness of this piece, truly. However, I must gently point out that the conflation of correlation with causation in the gut microbiome section is statistically tenuous. Moreover, the omission of epigenetic modifiers-particularly DNA methylation patterns in CD4+ T-cells-is a glaring oversight. Perhaps a peer-reviewed citation would have elevated the discourse.
Brooks Beveridge
December 30 2025You're not broken. You're not a burden. You're a warrior. Every time you get out of bed with stiff joints, you're winning. I'm proud of you. Keep going. We're all right here with you. 💙
Anu radha
January 1 2026I have psoriasis on my elbow. My husband says it's just dry skin. I didn't know it could hurt my joints. I will tell him now. Thank you for writing this.