How to Read Storage Instructions on Medication Labels
Have you ever opened a medicine bottle and wondered, Should this be in the fridge or on the shelf? You’re not alone. A 2023 survey found that nearly 7 out of 10 people store their medications in places that could make them less effective-or even dangerous. The answer isn’t guesswork. It’s written right on the label. But if you don’t know what to look for, those tiny words might as well be in another language.
Where to Find Storage Instructions on the Label
Look past the big font that says "Take one tablet daily." The storage info isn’t always in the spotlight. For over-the-counter meds like painkillers or antihistamines, check the "Other Information" section on the Drug Facts panel. That’s the part that comes after the active ingredients, uses, warnings, and directions. It’s usually near the bottom, often printed in smaller type. For prescription drugs, the instructions appear in the "Storage and Handling" section-sometimes labeled just "Storage." This is typically found in the prescribing information packet or on the pharmacy label attached to your bottle. The FDA requires this section to include any special conditions needed to keep the medicine safe and strong. Don’t assume all meds are stored the same way. A pill you take for high blood pressure might need to stay dry, while your child’s antibiotic syrup must stay cold. Always read the label for each medication separately-even if you’ve taken it before. Formulations change, and so can storage rules.Decoding the Common Terms
Storage instructions use specific language. Here’s what they really mean:- Store at controlled room temperature - This means between 68°F and 77°F (20°C to 25°C). It’s not "anywhere in your house." Avoid places that get too hot or too cold. Your kitchen counter near the oven? Too hot. Your windowsill? Too cold in winter.
- Refrigerate - Keep it between 36°F and 46°F (2°C to 8°C). That’s the main fridge compartment, not the door. The door swings open every time someone grabs a soda, and the temperature there can spike above 50°F. Insulin, some liquid antibiotics, and certain biologics fall into this category.
- Protect from light - Sunlight and even bright indoor lights can break down some drugs. Keep them in their original opaque bottle. Don’t transfer them to clear pill organizers unless the label says it’s safe.
- Store in a dry place - Humidity kills. Bathrooms are the worst place for meds. Showers create steam. That moisture can make tablets crumble, capsules stick together, or liquids grow mold. A bedroom drawer or a cabinet in a cool hallway is better.
- Avoid freezing - Just because something says "refrigerate" doesn’t mean it can handle ice. Freezing can destroy the structure of liquids and injectables. Insulin, for example, becomes useless if frozen-even once.
Why It Matters: What Happens When You Ignore the Rules
Storing medicine wrong isn’t just about wasting money. It can hurt you. Take acetaminophen-the active ingredient in Tylenol. If it’s exposed to heat and moisture over time, it can break down into a toxic compound called NAPQI. That’s the same chemical that causes liver damage in overdose cases. You won’t feel any difference in taste or color, but your body will. Liquid antibiotics like amoxicillin lose potency fast if left unrefrigerated. A 2022 study showed that some brands dropped below 90% effectiveness within 48 hours at room temperature. That means your child’s infection might not clear up-and could get worse. Nitroglycerin tablets, used for chest pain, are extremely sensitive. If they’re exposed to heat or air, they can become useless in under a month. In an emergency, that could be life-threatening. The FDA tracked over 1.2% of all medication errors between 2020 and 2022 as being linked to improper storage. That’s tens of thousands of cases. Most go unreported because people don’t realize their medicine failed due to storage, not because the drug didn’t work.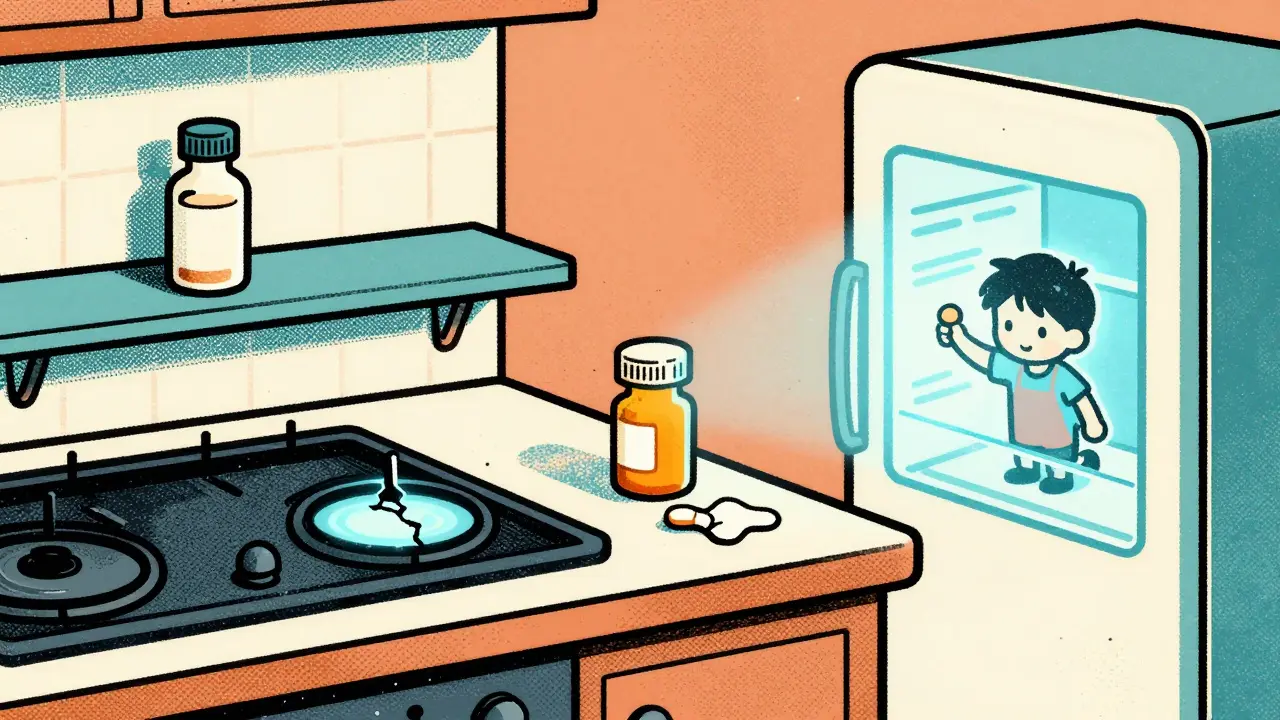
Where NOT to Store Your Medications
Here are the top three worst spots for storing meds-and why:- The bathroom cabinet - Steam, humidity, and temperature swings from showers make this the #1 mistake. Even if it looks clean and convenient, it’s the worst place for pills.
- The car - On a 90°F day, the inside of a parked car can hit 140°F in under 30 minutes. That’s hotter than an oven. Pills, patches, and liquids left in glove boxes or cup holders can melt, separate, or degrade.
- The kitchen near the stove or microwave - Heat rises. If your meds sit above the stove or next to the microwave, they’re getting baked daily. Even a few weeks of this can reduce potency.
Best Practices for Safe Storage at Home
Follow these simple rules to keep your meds working as they should:- Use a cool, dry drawer or cabinet away from windows and appliances.
- Keep meds in their original containers with the label attached. That way, you always have the expiration date and storage info handy.
- If you need to use a pill organizer, only fill it for a few days at a time, especially for temperature-sensitive drugs.
- For refrigerated meds, store them on a middle shelf-not the door. Use a small, dedicated container so they don’t get mixed with food.
- Consider a small digital thermometer and hygrometer in your storage area. You don’t need fancy gear. A $10 device from a hardware store can tell you if your cabinet stays between 60°F and 70°F with humidity below 60%.
- Keep all medications out of reach of children and pets-even if they’re "just in the drawer."
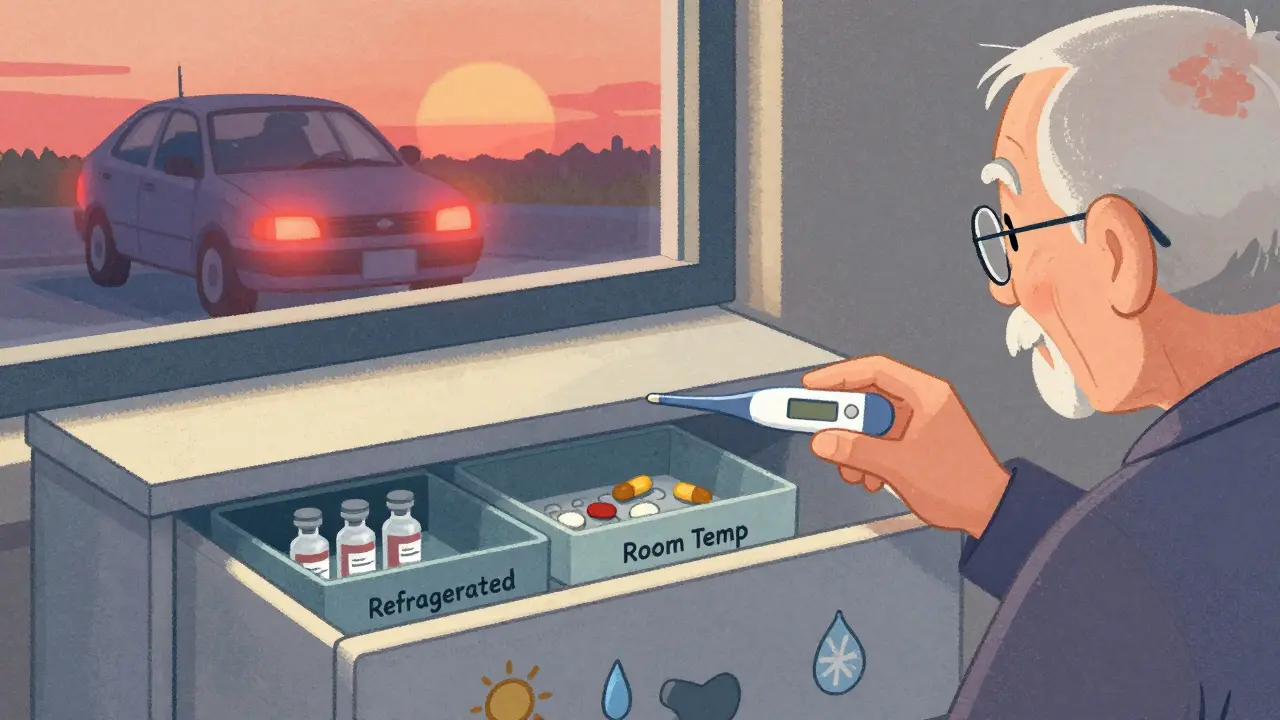
Special Cases: Kids, Travel, and Seniors
Children’s medicines often have different storage needs than adult versions. A children’s liquid ibuprofen might need refrigeration after opening, while the adult tablet version doesn’t. Always check the label-or ask your pharmacist. Traveling? Pack temperature-sensitive meds in a small insulated bag with a cold pack. Don’t check them in luggage. Airplane cargo holds can freeze or overheat. Keep them in your carry-on. If you’re flying across time zones, bring extra doses in case of delays. Seniors living in homes without air conditioning face real challenges. If your house hits 90°F in summer, your pills might be at risk. Talk to your pharmacist. They can sometimes switch you to a tablet form instead of a liquid, or suggest a different brand with more stable storage requirements.When in Doubt, Ask Your Pharmacist
You don’t have to be an expert to read the label. But if you’re confused-whether it’s because the wording is unclear, or your home doesn’t have a cool, dry spot-ask your pharmacist. They see this every day. A 2023 survey by Express Scripts showed that 68% of people admit to storing meds in less-than-ideal conditions. Most don’t realize it’s a problem. But pharmacists can help you adapt. They’ve seen homes with no AC, garages turned into storage rooms, and people keeping meds in drawers next to hair dryers. They’ve got practical solutions. And if you’re ever unsure whether your medicine has gone bad-whether it changed color, smell, or texture-don’t guess. Take it to the pharmacy. They’ll dispose of it safely and give you a new one if needed.What’s Coming Next
The future of medication storage is getting smarter. Major pharmacies like CVS and Walgreens are testing QR codes on labels that link to real-time storage advice based on your location and the current weather. Imagine scanning your insulin pen and seeing: "Today’s temperature in Birmingham is 82°F. Store in fridge. Do not leave in car." In the next five years, some high-risk medications will come with built-in temperature sensors. If the pill bottle gets too hot, it’ll glow red or send a notification to your phone. This isn’t sci-fi-it’s already in pilot testing. But for now, the simplest tool is still the one on the label. Take a second. Read it. Your health depends on it.Can I store all my medications in the same place?
No-not all medications need the same conditions. Some must be refrigerated, others need to stay dry and cool. Mixing them can lead to contamination or degradation. Use separate containers if needed. A small labeled box for refrigerated meds and another for room-temperature ones helps keep things organized and safe.
What if my medicine looks different? Should I still use it?
If a pill has changed color, cracked, become sticky, or smells odd, don’t take it. Liquid medicines that look cloudy, separated, or have particles floating in them should be discarded. These are signs the medication has broken down. Take it to your pharmacy for safe disposal and ask for a replacement.
Is it okay to keep medications in a pill organizer?
Yes-but only for short-term use. Pill organizers expose meds to air and light, which can reduce potency over time. Use them for a week or less, especially for drugs that are sensitive to humidity or heat. Always keep the original bottle as your main storage, and use the organizer just to help you remember doses.
How long can I keep a medicine after opening it?
It depends on the drug. Some pills last until the printed expiration date. Liquids, eye drops, and insulin often expire soon after opening-sometimes within 14 days. Always check the label for "discard after" dates. If it doesn’t say, ask your pharmacist. Never use medicine past its expiration date, even if it looks fine.
Can I store medications in the freezer to make them last longer?
Only if the label specifically says "freeze." For almost all medications, freezing will damage the active ingredients. Insulin, antibiotics, and vaccines can become useless or even harmful if frozen. Stick to the exact instructions: "refrigerate" means fridge, not freezer. If you’re unsure, call your pharmacy.





15 Comments
Glenda Marínez Granados
January 22 2026So let me get this straight... we’re trusting our lives to tiny pills that turn into poison if left near a toaster? 🤡 I’ve been keeping my insulin in the glovebox ‘cause it’s ‘convenient.’ Guess I’m just one bad road trip away from becoming a cautionary tale. 😅
shubham rathee
January 23 2026this is all government propaganda to sell more meds and make pharmacists rich i mean why would they put storage info on the bottle if they didnt want us to ignore it the real story is big pharma wants you to buy new bottles every month because your old ones are magically broken by humidity lol
Sangeeta Isaac
January 25 2026i used to keep my blood pressure pills in the bathroom like a total chad. then one day i found a moldy capsule that looked like it had its own little ecosystem. now i store em in a Tupperware in my sock drawer. no one’s ever accused me of being a health guru but hey, i’m alive. 🧦💊
Alex Carletti Gouvea
January 27 2026This is why America is falling apart. We can’t even read a label without needing a PhD in pharmaceutical science. Back in my day, you took your medicine like a man-no thermometer, no QR codes, no ‘discard after 14 days.’ Just swallow it and shut up.
Roisin Kelly
January 28 2026They didn’t mention the REAL danger: the government’s using your meds to track your health data. That QR code? It’s not for storage advice-it’s for your insurance company to see you’re still alive. They’ll raise your rates if you take too many pills. I’m throwing mine in the river.
lokesh prasanth
January 29 2026Storage instructions are just corporate legalese. The real question is why do we need so many pills in the first place? Maybe the problem isn’t how we store them but why we take them at all
Yuri Hyuga
January 31 2026This is such an important post! 🙌 Seriously, so many people overlook this-and it’s not just about efficacy, it’s about dignity. Your body trusts the medicine. Don’t betray that trust by storing it like a forgotten snack in a hot car. 🚗💨 A little care goes a long way. You’ve got this!
MARILYN ONEILL
January 31 2026I mean, if you’re the kind of person who needs a 2000-word guide to store pills, maybe you shouldn’t be taking them at all. I just keep mine in my purse. They work. End of story.
Coral Bosley
February 2 2026I used to keep my antidepressants in the kitchen because it was ‘easy to remember.’ Then I realized I’d been eating them with my cereal for three months. I don’t even remember taking them. I just… ate them. Like snacks. I’m not okay.
Uju Megafu
February 2 2026You think this is bad? In Nigeria, people store meds in plastic bags tied to ceiling beams because they don’t have cabinets. And still, they live longer than Americans who have smart fridges but can’t read the word ‘refrigerate.’ This isn’t about storage-it’s about privilege.
Barbara Mahone
February 4 2026I’ve started labeling my pill containers with sticky notes: 'DO NOT PUT IN CAR.' It’s not elegant, but it works. My cat hasn’t eaten any pills yet. Progress.
Kelly McRainey Moore
February 5 2026I just realized I’ve been keeping my thyroid meds next to my coffee maker. Oops. 🤦♀️ I’m moving them to the hall closet tonight. Thanks for the nudge.
Stephen Rock
February 6 2026Why does this even matter? The system’s rigged. Your meds are designed to expire. You’re just a customer. Read the label? Nah. I just take it till it stops working then buy more.
Amber Lane
February 7 2026My grandma used to say, 'If it looks weird, don’t chew it.' She never read a label. Lived to 98. Maybe the real answer is trust your gut.
Ashok Sakra
February 8 2026I store all my meds in my sock drawer with my dirty socks. It’s dark. It’s dry. And no one touches them. Plus my cat hates the smell. Win win.