VA Generic Medication Coverage: Understanding Veterans Affairs Formulary Benefits
Every day, 9 million veterans depend on the Veterans Affairs (VA) system to get prescription medications at affordable prices. Understanding your VA formulary is key to saving money on prescriptions. The VA National Formulary is the official list of medications available at all VA healthcare facilities nationwide, established in 1998 and updated monthly. This system ensures veterans get the right drugs at the right price-without hidden fees or surprise costs.
How the VA Formulary Works: Tiered Copay System
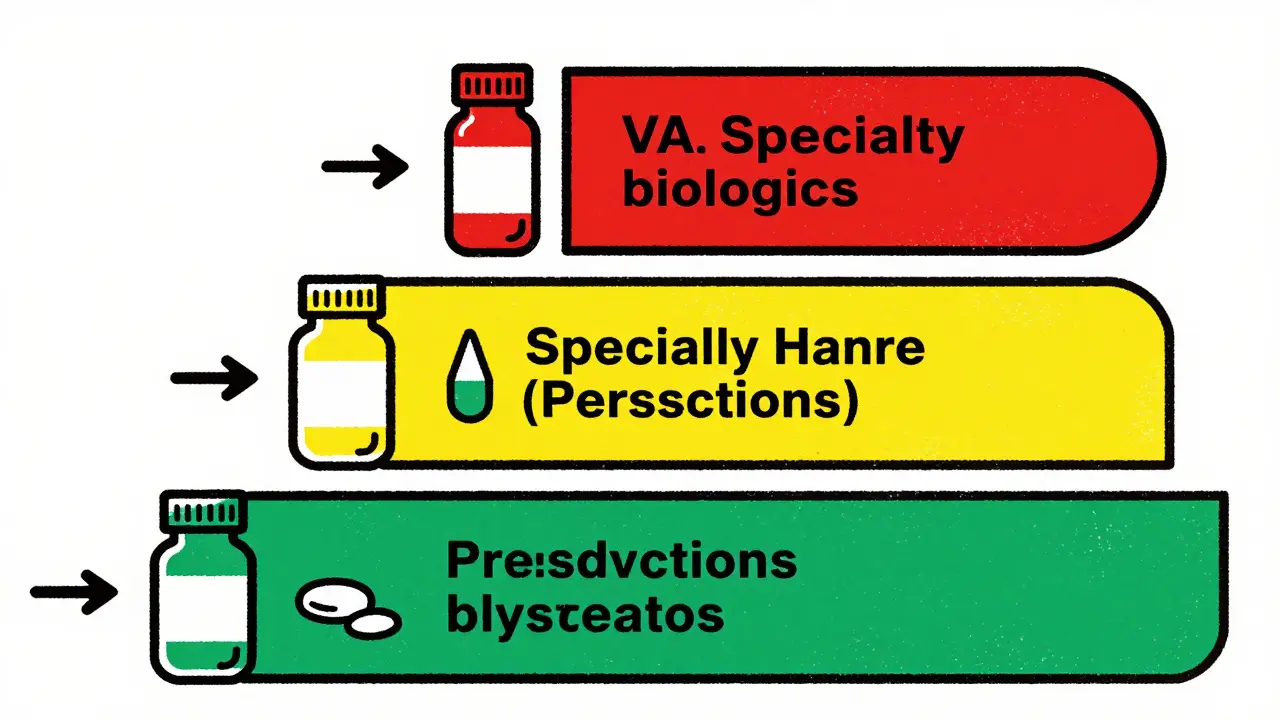
The VA uses a simple three-tier system to manage prescription costs. Tier 1 medications are preferred generic drugs with the lowest copay, typically $5-$10 for a 30-day supply. This includes common medications like alendronate (for osteoporosis), aspirin (for heart health), and sertraline (for depression). Tier 2 covers some brand-name drugs and higher-cost generics, with copays around $10-$20. Tier 3 includes specialty medications like cancer treatments or biologics, costing $20-$50 per fill.
| Tier | VA Copay | Medicare Part D Copay | Common Medications |
|---|---|---|---|
| Tier 1 | $5-$10 | $15-$40 | Alendronate, Atorvastatin, Sertraline |
| Tier 2 | $10-$20 | $40-$60 | Some brand-name generics |
| Tier 3 | $20-$50 | $60-$100+ | Specialty medications (e.g., biologics) |
For example, when Meds by Mail the VA's prescription delivery service sends your monthly sertraline (generic Zoloft), you pay $0 copay-versus $15 at most local pharmacies. This difference adds up fast: veterans using Meds by Mail save over $180 per year on average.
How to Check if Your Medication is Covered
Before filling a prescription, always verify coverage using the VA Formulary Advisor a free online tool for checking medication coverage. Simply enter your drug name or National Drug Code (NDC) number at VA.gov. The tool shows exactly which tier it's on and your copay amount. You can also download the latest formulary data in Excel or CSV format from the VA National Drug File.
Pro tip: If your medication isn't listed, don't panic. Your VA provider can request a prior authorization. This process usually takes 24-48 hours and requires a short clinical justification. For urgent needs, the VA Urgent/Emergent Formulary allows immediate access to non-formulary drugs in emergencies through community pharmacies.

Meds by Mail: Free Delivery for Maintenance Medications
Most veterans don't realize they can get up to a 90-day supply of maintenance medications delivered free to their door. Meds by Mail the VA's prescription delivery service eliminates pharmacy trips and copays for Tier 1 drugs. Over 1.2 million veterans use this service monthly, with 87% reporting high satisfaction in VA's 2024 survey.
Here's what you need to know:
- No cost share for Tier 1 medications (like blood pressure pills or antidepressants)
- Delivered in 7-10 business days
- Refills automatically processed when eligible
- Special handling for refrigerated drugs like insulin
Many veterans prefer Meds by Mail because it avoids the "pharmacy wait time" problem. As one Reddit user shared: "I switched to Meds by Mail for my diabetes meds. No more driving 30 miles to the pharmacy-just waiting for the box to arrive." This service is especially helpful for rural veterans or those with mobility issues.
CHAMPVA Coverage for Specific Medications
For veterans using the Civilian Health and Medical Program (CHAMPVA), coverage rules differ slightly. CHAMPVA the VA's health program for dependents and survivors follows the same formulary but has specific restrictions. As of January 2025, GLP-1 medications like Ozempic and Wegovy are covered only for FDA-approved uses: type 2 diabetes, sleep apnea, or cardiovascular prevention. Weight loss uses outside these indications require prior authorization.
For example, if you're prescribed Wegovy for weight loss, your provider must submit clinical documentation showing you have obesity-related complications. The VA's National Drug Formulary Committee reviews these requests within 72 hours. This targeted approach ensures veterans get the right drugs for their specific health needs without unnecessary costs.

Common Challenges and How to Solve Them
Even with a robust system, veterans sometimes face hurdles. Here's what to expect and how to handle it:
- Tier confusion: New enrollees often mix up Tier 1 and Tier 2 copays. Always check your formulary status before filling prescriptions. VA pharmacy staff help explain tiers during your first visit.
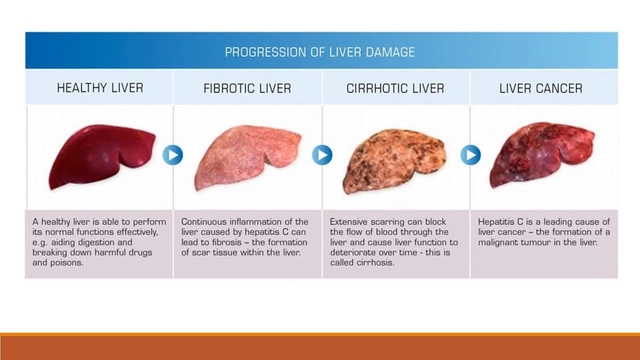
- Prior authorization delays: Specialty drugs like cancer treatments may require paperwork. Call the VA Pharmacy Benefits call center at 1-800-877-8339 for real-time help-they handle 18,000 calls daily.
- Generic substitution concerns: Some veterans worry generics aren't as effective. But 94% of those who tried generics after initial concerns reported no issues. Your VA provider can address these worries during your appointment.
Remember: The VA's generic substitution policy saves you money without compromising care. In 2024, this approach generated $2.8 billion in annual savings while maintaining identical clinical outcomes compared to brand-name drugs.
What's Next for VA Formulary? (2026 Updates)
The VA is constantly improving its system. By Q3 2026, artificial intelligence will help suggest therapeutic alternatives directly in your electronic health record. This means your provider gets real-time guidance on cost-effective drug swaps during appointments.
Other upcoming changes include:
- Expanded coverage for rare disease treatments in oncology
- Real-time formulary status indicators in e-prescribing systems
- Enhanced telehealth support for medication management
These updates build on the VA's proven track record: 92% generic utilization rate (higher than commercial insurers' 89%) and $1,850 average annual prescription cost per veteran versus $2,700 for commercial insurance.
How do I check if my medication is covered by the VA?
Use the VA Formulary Advisor tool on VA.gov. Enter your drug name or NDC number to see coverage details, including tier and copay. You can also call the VA Pharmacy Benefits call center at 1-800-877-8339 for immediate assistance. Most queries are resolved within minutes.
What's the difference between VA and Medicare formularies?
The VA uses a simpler three-tier system with lower copays, while Medicare Part D typically has five tiers with higher costs. For example, Tier 1 VA copays are $5-$10 versus $15-$40 for Medicare. The VA also enforces stricter generic substitution rules-92% of VA prescriptions are generics compared to 85% in Medicare Part D. This results in significant savings: veterans pay $1,850 annually for prescriptions versus $2,300 for Medicare beneficiaries.
Can I get my medications through mail order?
Yes! The VA's Meds by Mail program delivers up to a 90-day supply of maintenance medications directly to your home at no cost for Tier 1 drugs. Over 1.2 million veterans use this service monthly. Refills are automatic, and delivery takes 7-10 business days. You can sign up through your VA healthcare provider or online at VA.gov.
What if my medication isn't on the VA formulary?
Your VA provider can request prior authorization for non-formulary drugs. For urgent needs, the VA Urgent/Emergent Formulary allows immediate access through community pharmacies. Most prior authorization requests are approved within 24-48 hours. If denied, you can appeal through the VA's formal review process.
How does the VA handle generic substitutions?
The VA defaults to generic medications when available-this is standard practice unless your provider specifies a brand-name drug is medically necessary. Studies show 94% of veterans who tried generics report no difference in effectiveness compared to brand-name drugs. This policy saves veterans an average of $180 per year on common prescriptions like blood pressure medications.



9 Comments
Savannah Edwards
February 6 2026As someone who's seen veterans from all walks of life, I really appreciate how the VA's formulary system makes meds affordable. It's not just about the copays either - it's about dignity. When my buddy from the Marines needed insulin, he didn't have to choose between rent and meds. The Meds by Mail service is a game-changer for rural vets like him. I remember hearing a story about a vet in Montana who'd drive 4 hours for a prescription before they had mail order. Now he gets it delivered. And the tier system is so straightforward compared to Medicare. Like, Tier 1 generics at $5 vs Medicare's $15? That's huge savings. Also, the fact that they cover biologics for cancer treatments at Tier 3 with $20-$50 copay is life-saving. I know some people worry about generics, but studies show they're just as effective. The VA's 92% generic use rate is impressive. It's not just about saving money either - it's about getting the right meds without hassle. The formulary advisor tool is super easy to use. Just type in your drug and it tells you everything. No more guessing. And for those with CHAMPVA, the coverage rules are clear. Like, Ozempic for diabetes is covered but not for weight loss. Makes sense. Overall, the VA system is way better than private insurance. I've seen too many vets struggle with high drug costs elsewhere. This is why I'm proud to support our veterans' healthcare. Seriously, if you're a vet, take advantage of these benefits. You deserve it.
Mayank Dobhal
February 6 2026Prior auth delays are killing us.
Marcus Jackson
February 7 2026Actually, the VA's generic substitution is backed by studies showing 94% effectiveness. You don't need to worry about generics. They're just as good.
Natasha Bhala
February 7 2026i switched to med by mail for my blood pressure meds no more driving 30 miles just wait for the box lifesaver thanks va
Gouris Patnaik
February 8 2026In India, healthcare is universal and free. VA's system is outdated. Why charge anything? It's a disgrace.
Jesse Lord
February 9 2026hey if youre struggling with va meds reach out were here to help the formulary advisor is easy just check it out youll find what you need
AMIT JINDAL
February 10 2026OMG this is so great 😍 The VA system is way better than Medicare. I know because I've used both. Tier 1 is $5 vs $15 on Medicare. That's a no-brainer! 😂 But seriously, the prior auth process needs to be faster. My friend's insulin was delayed. 😠 But overall, VA is awesome! 🌟
Catherine Wybourne
February 12 2026Oh, the VA formulary? It's lovely. Except for when it's not. Like, 'Tier 3 $50 copay' - that's nothing compared to private insurance. Oh wait, it is. Haha. But seriously, Meds by Mail is a lifesaver for us Brits living in the US. No more pharmacy queues. Cheers!
Ashley Hutchins
February 14 2026you all need to stop complaining va does great work my cousin is a vet and he says its perfect if you dont like it dont use it simple also why are you all so negative its not that hard