Autism and Diet: How Nutrition Impacts Autism Spectrum Disorder
Autism Diet Impact Calculator
Estimated Impact Summary
Diet Recommendations
Diet Comparison Guide
Gluten-Free
Low-Moderate EvidenceReduces GI distress and may improve mood.
Casein-Free
Low EvidenceMay decrease mucus production and improve sleep.
Mediterranean
High EvidenceRich in omega-3s and antioxidants; supports overall health.
Ever wondered if changing what's on the plate could change life for someone on the autism spectrum? The idea that food matters isn’t new, but the science behind it is still catching up. Below you’ll find a plain‑spoken guide that cuts through the hype, outlines what the research really says, and gives you a toolbox of practical steps you can start using today.
Key Takeaways
- Nutrition can affect behaviour and gut health in autistic children, but no single diet works for everyone.
- Evidence supports modest benefits from gluten‑free, casein‑free, and omega‑3‑rich diets, especially when tailored to individual sensitivities.
- Before starting any plan, screen for nutrient deficiencies, consult a qualified dietitian, and monitor progress with a simple checklist.
- Safety matters: extreme restrictions can lead to low iron, calcium, or vitamin D, which may worsen behavioural challenges.
- Combine diet tweaks with behavioural therapies for the most reliable improvements.
Understanding Autism Spectrum Disorder
Autism Spectrum Disorder is a neurodevelopmental condition characterized by differences in social communication, repetitive behaviours, and sensory processing. It appears early in childhood and persists throughout life, with wide variability in abilities and challenges. The brain differences associated with ASD can also influence appetite, texture preferences, and how the body processes nutrients. This link is why many families explore dietary strategies as part of a broader support plan.
Why Nutrition Matters
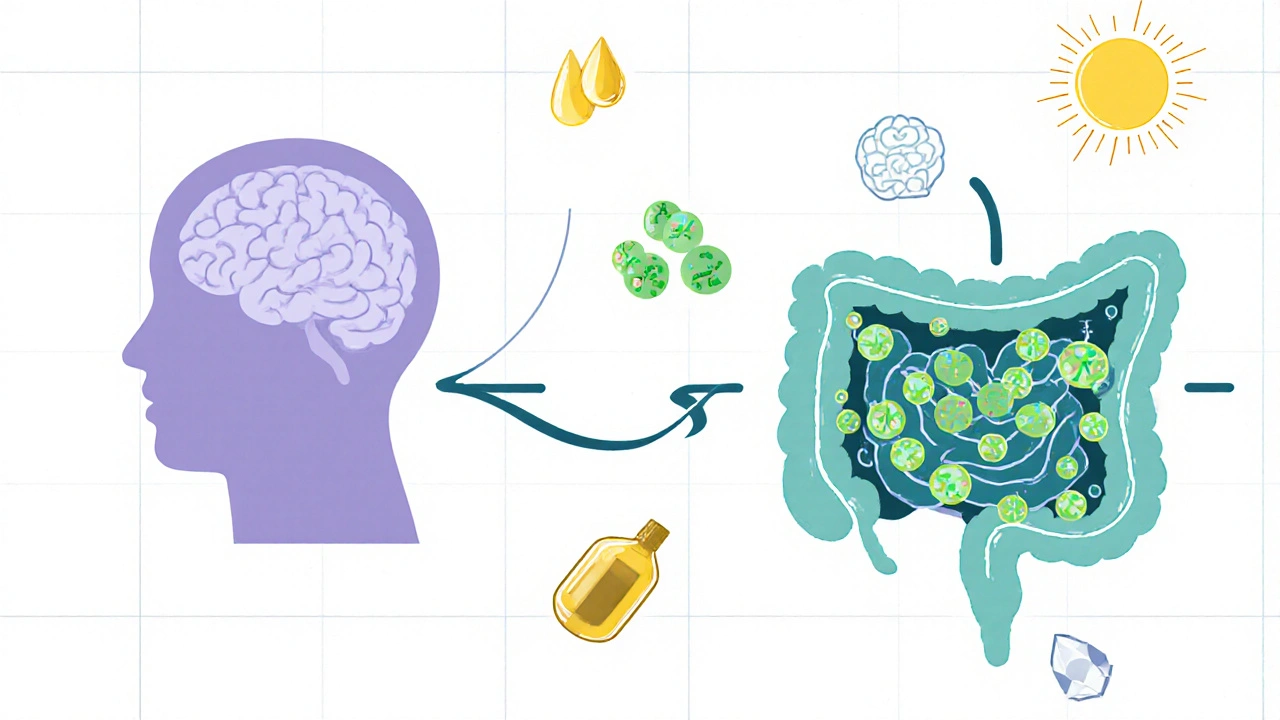
Nutrition does more than fuel the body. It shapes the gut microbiome, modulates inflammation, and supplies the building blocks for neurotransmitters that affect mood and cognition. For autistic individuals, who often experience gut‑brain communication differences, the impact can be noticeable.
Core Nutritional Concepts
Nutrition is the intake of food substances that support growth, repair, and daily function. It includes macronutrients (carbs, protein, fat) and micronutrients (vitamins, minerals) that each play a role in brain health. Below are the nutrients most frequently discussed in autism research.
- Omega‑3 Fatty Acids are polyunsaturated fats found in fish oil, flaxseed, and walnuts. They help build cell membranes in the brain and reduce inflammation.
- Vitamin D supports immune regulation and neuronal development. Low levels are common in children who spend a lot of time indoors.
- Probiotics are live bacteria that help balance the gut microbiome, which can influence anxiety, irritability, and sleep.
- Gut Microbiome refers to the trillions of microbes living in the digestive tract. Research shows a distinct composition in many autistic children, linked to gastrointestinal symptoms and behaviour.
Popular Dietary Approaches
Several structured diets have gained traction among parents and clinicians. Below is a quick snapshot of each, followed by a deeper dive.
Gluten‑Free Diet eliminates wheat, barley, and rye. Some families report reduced bloating and calmer behaviour after removal. Casein‑Free Diet cuts out dairy proteins, which can be difficult for children with oral sensory sensitivities. Gluten‑Free, Casein‑Free (GFCF) Combination combines the two restrictions. It’s the most studied protocol, though results vary. Specific Carbohydrate Diet (SCD) limits complex carbs, aiming to reduce gut inflammation by starving harmful bacteria. Ketogenic Diet is a high‑fat, low‑carb plan that forces the body into ketosis, potentially stabilizing neural firing patterns. Mediterranean‑Style Diet emphasizes whole grains, fruits, vegetables, fish, and olive oil-rich in omega‑3s and antioxidants.Evidence Snapshot
Research on diet and autism is a patchwork of small trials, observational studies, and parent surveys. Here’s what the most credible data show.
- GFCF: A 2022 meta‑analysis of 13 randomized controlled trials (RCTs) found modest improvements in social interaction for children with confirmed gluten or casein sensitivities, but no benefit for the broader ASD population.
- Omega‑3 Supplementation: A 2021 double‑blind RCT with 120 participants reported a 15% reduction in hyperactivity scores after 12 weeks of high‑quality fish‑oil capsules (1000mg EPA/DHA). \n
- Probiotics: A 2023 multicenter trial showed that a 4‑week course of Lactobacillus rhamnosus GG decreased GI complaints and improved sleep quality in 78% of participants.
- Vitamin D: Observational data from the UK National Health Service (NHS) indicate that children with serum 25‑(OH)D levels below 20ng/mL are 1.8× more likely to exhibit severe sensory aversions.
Practical Guide for Parents
Before you overhaul the pantry, follow this checklist to keep things safe and effective.
- Get a baseline assessment. Request a full blood panel (iron, ferritin, calcium, vitamin D, B12) from your GP or paediatrician.
- Identify food sensitivities. Work with an allergist or dietitian to run elimination trials-usually two weeks per food, noting behavioural and GI changes.
- Choose a diet that matches the findings. If gluten sensitivity shows up, start with a gluten‑free trial; otherwise, consider a balanced Mediterranean approach.
- Monitor progress. Use a simple daily log: sleep hours, GI symptoms, melatonin use, and any behaviour rating (e.g., ABC‑2 score).
- Adjust nutrients. If the diet cuts out dairy, add calcium‑rich alternatives (broccoli, fortified soy milk). If carbs are reduced, ensure enough fibre from fruits and legumes.
- Re‑evaluate every 3months. Blood work and behaviour logs will tell you whether the plan is helping or causing deficiencies.
Potential Pitfalls
Extreme restriction can backfire. Here are red flags to watch.
- Weight loss or growth faltering. Track height and weight at each clinic visit.
- Low iron or calcium. Symptoms include fatigue, pale skin, and brittle nails.
- Increased food anxiety. If a child becomes more resistant to eating, the diet may be causing stress.
- Social isolation. Strict diets can make school lunches and birthday parties tricky; plan inclusive meals ahead.

Combining Diet with Other Therapies
The strongest outcomes arise when nutrition is paired with evidence‑based behavioural interventions such as Applied Behaviour Analysis (ABA), Speech‑Language Therapy, or Occupational Therapy. Nutrition can smooth the physiological landscape, while therapies address skill building.
Comparison of Common Diets
| Diet | Evidence Level | Typical Restrictions | Potential Benefits | Common Risks |
|---|---|---|---|---|
| Gluten‑Free | Low‑to‑moderate (small RCTs) | Wheat, barley, rye | Reduced GI distress, possible calmer mood | Fiber loss, vitamin B deficiency |
| Casein‑Free | Low (limited trials) | Dairy proteins | Less mucus production, improved sleep | Calcium shortfall, higher cost |
| GFCF (Gluten+Casein‑Free) | Moderate (meta‑analysis 2022) | Wheat, barley, rye, dairy | Combined GI relief, occasional behaviour gains | Complex meal planning, risk of multiple deficiencies |
| Specific Carbohydrate Diet | Very low (case series) | All complex carbs (e.g., legumes, most grains) | Lower inflammation markers in some reports | Very restrictive, possible nutrient gaps |
| Ketogenic | Very low (small pilot studies) | High fat, low carbs | Potential seizure reduction, mood stabilization | Kidney stones, high saturated fat intake |
| Mediterranean‑Style | High (large cohort studies) | Few - focuses on quality foods | Rich in omega‑3, antioxidants; supports gut health | Generally safe, may need portion control for weight |
Frequently Asked Questions
Can a diet cure autism?
No. Autism is a lifelong neurodevelopmental condition. Diet can influence symptoms like GI issues, sleep, or attention, but it does not eliminate core autistic traits.
How long should an elimination trial last?
Typically 2-4weeks per food, followed by a re‑introduction phase to see if symptoms reappear. Keep a daily log to spot subtle changes.
Are supplements like omega‑3 safe for children?
Yes, when dosed appropriately (around 20mg per kg body weight of EPA+DHA). Choose products tested for purity, especially regarding heavy metals.
What signs indicate a nutrient deficiency?
Persistent fatigue, pale skin, frequent bruising, bone pain, or worsening behavioural spikes can hint at low iron, vitamin D, or calcium. Blood testing is the definitive check.
Should I try a diet before seeing a professional?
A brief trial under professional guidance is safest. Unsupervised restriction may lead to hidden deficiencies that can be hard to reverse later.
Next Steps
If you’re ready to explore nutrition for your autistic child, start with a conversation at the next GP or NHS clinic appointment. Bring a copy of this guide, ask for a referral to a paediatric dietitian, and request baseline blood work. From there, you can design a personalised plan that balances nutritional adequacy with any identified food sensitivities.
Remember, the goal isn’t a perfect diet; it’s a supportive routine that helps your child feel better physically, which often translates into smoother days socially and emotionally.






17 Comments
Kartikeya Prasad
October 10 2025Oh great, another miracle diet that promises to turn a toddler into a Zen monk – because that’s totally realistic 🙃. Let’s just hope the gluten‑free unicorns don’t eat all the calcium.
Tiffany Owen-Ray
October 17 2025Reading through the whole guide felt like embarking on an epic pilgrimage across the culinary map of autism research. One cannot ignore the sheer complexity of gut‑brain interactions; they are as tangled as a medieval tapestry. While the evidence for a strict GFCF regimen is modest at best, it does highlight a critical point: individual variability reigns supreme. A child who exhibits clear gluten sensitivity may indeed benefit, yet blanket prescriptions risk depriving them of essential nutrients. The Mediterranean‑style approach, on the other hand, stands out for its robust evidence base, offering omega‑3s, antioxidants, and a balanced macronutrient profile that supports neurodevelopment without the pitfalls of severe restriction. Moreover, the tables of micronutrient deficiencies serve as a stark reminder that any diet, no matter how well‑intended, must be paired with vigilant monitoring of iron, vitamin D, calcium, and B‑vitamins. It is encouraging to see the emphasis on baseline blood work, as this anchors the dietary experiment in objective data rather than anecdotal hope.
When families consider elimination trials, the recommended 2‑4 week windows are sensible; they provide enough time to observe subtle shifts in behavior or GI symptoms without dragging out uncertainty. The checklist framework for sleep, GI, and behavioral scoring is a practical tool that can translate subjective observations into actionable insights. Integrating diet with established therapies such as ABA or speech‑language therapy creates a synergistic effect: nutrition smooths the physiological terrain while behavioral interventions sculpt functional skills.
In the end, the mantra should be “personalized, monitored, balanced.” No single diet is a panacea, but a thoughtful, data‑driven approach can certainly tip the scales toward better quality of life for autistic children and their families.
Kate Taylor
October 24 2025The neurophysiological underpinnings you mentioned align with current literature on the gut‑microbiome‑brain axis, particularly the role of short‑chain fatty acids in modulating neuroinflammation. When constructing an elimination protocol, leveraging an evidence‑based biomarker panel (e.g., serum zonulin, fecal calprotectin) can strengthen the causal inference between dietary change and symptom modulation. Additionally, incorporating a standardized behavioural metric such as the Aberrant Behavior Checklist ensures reproducibility across clinical settings.
Yareli Gonzalez
October 31 2025Keeping the plan simple helps the child feel safe, and involving them in food choices can reduce anxiety. Documentation of any changes, even minor ones, is key for future adjustments.
Alisa Hayes
November 7 2025Before diving head‑first into any restrictive regimen, it’s wise to get a full blood panel – iron, ferritin, vitamin D, calcium, B12 – and to consult a paediatric dietitian. Those labs give you a concrete baseline and help avoid unintentionally creating new deficiencies while you’re trying to address existing ones.
Mariana L Figueroa
November 14 2025Start small, track daily, adjust as needed.
mausumi priyadarshini
November 21 2025Actually, the whole premise of "elimination trials" is fundamentally flawed; there is no scientific consensus-so why rely on such a shaky methodology?????
Carl Mitchel
November 28 2025It’s ethically irresponsible to suggest diet as a cure‑all without emphasizing that autism is a neurodevelopmental condition, not a disease to be eradicated. Parents need to understand that dietary tweaks may alleviate comorbid GI issues, but they will not change the core autistic traits.
Suzette Muller
December 5 2025I appreciate the reminder about the core condition. Balancing realistic expectations with hopeful optimism is the best way to support families navigating these decisions.
Josh SEBRING
December 12 2025Honestly, you’re overcomplicating it-just cut the dairy and wheat and see if anything changes. No need for endless labs if the kid looks fine.
Lily Tung
December 19 2025The discourse surrounding nutritional interventions often suffers from a paucity of rigorous methodology; consequently, many lay‑person recommendations lack statistical robustness. When evaluating the literature, one must prioritize double‑blind, placebo‑controlled trials over anecdotal case series to mitigate confirmation bias. Moreover, the heterogeneity of ASD phenotypes necessitates stratified analyses-aggregating data across disparate subpopulations obscures true effect sizes. It is also essential to differentiate between correlation and causation; merely observing symptom improvement concurrent with diet change does not establish a causal link. Researchers should therefore employ standardized outcome measures, such as the Social Responsiveness Scale, to facilitate cross‑study comparability. Finally, the ethical imperative to avoid nutrient deficiencies must remain paramount, particularly in pediatric cohorts with limited dietary diversity.
siddharth singh
December 26 2025While I respect the call for methodological rigor, we cannot ignore the lived experiences of families who report tangible benefits from targeted dietary changes. The challenge lies in bridging controlled‑trial evidence with real‑world applicability, ensuring that any recommended protocol is both scalable and safe.
Angela Green
January 1 2026Correcting a minor typo: it should be “gluten‑free” not “gluten free”.
April Malley
January 8 2026Thanks for the thorough breakdown! I’ll definitely pass this along to my sister, who’s looking into diet tweaks for her son – the tables make it so much easier to compare options, and the reminder about regular blood work is spot on.
scott bradshaw
January 15 2026Oh sure, because a Mediterranean diet will magically fix everything – data doesn’t lie, right?
Crystal Price
January 22 2026Listen, if you think a diet can rescue a child from the depths of autism, you’re living in a fantasy novel. Reality is far less theatrical.
Beth Lyon
January 29 2026Interesting read.