Prednisone Mood Swings: Proven Coping Strategies and Where to Find Support
Prednisone Mood Swings Risk Assessment Tool
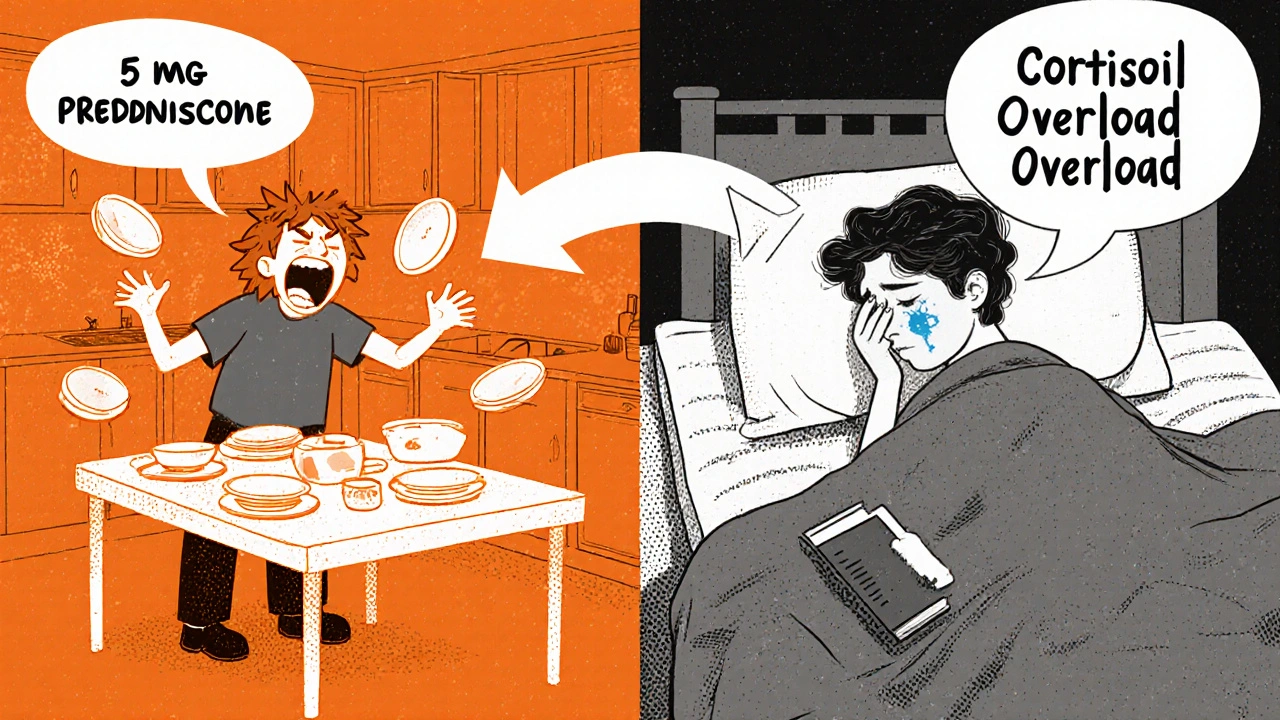
When you start taking prednisone, you expect swelling, weight gain, or trouble sleeping. But prednisone mood swings? That’s something no one warns you about until you’re screaming at your partner over a spilled cup of coffee or crying in the shower for no reason. You’re not losing your mind. You’re reacting to a powerful drug that rewires your brain chemistry.
Why Prednisone Changes Your Mood
Prednisone isn’t just an anti-inflammatory. It’s a synthetic version of cortisol, your body’s main stress hormone. When you take it, your brain doesn’t know the difference. It floods your limbic system-the emotional control center-with artificial signals. This directly messes with serotonin and dopamine, the chemicals that regulate mood, sleep, and motivation. According to the U.S. Food and Drug Administration, mood changes are a very common side effect, happening in more than 10% of users. Studies show between 18% and 47% of people on corticosteroids experience some kind of emotional disruption. For some, it’s mild irritability. For others, it’s full-blown anxiety, panic attacks, or even suicidal thoughts. The timing is tricky. Symptoms often show up within 5 to 7 days of starting the drug. And they don’t vanish the day you stop. Because prednisone has a half-life of 18 to 36 hours, the effects linger. One patient reported panic attacks starting five days after finishing a 19-day course. That’s not a coincidence-it’s neurochemistry.What Prednisone Mood Swings Actually Look Like
It’s not just “feeling moody.” These are real, measurable shifts in behavior and mental state:- **Sudden anger**-you snap at people you love, then feel guilty minutes later
- **Anxiety attacks**-racing heart, shortness of breath, feeling like you’re going to die, even when nothing’s wrong
- **Emotional lability**-crying one minute, laughing the next, with no clear trigger
- **False euphoria**-feeling unrealistically confident or “on top of the world,” which can lead to risky decisions
- **Depression**-loss of interest, fatigue, hopelessness, even thoughts of self-harm
- **Insomnia**-your brain won’t shut off, even when you’re exhausted
Who’s Most at Risk
Not everyone gets mood swings. But certain people are far more vulnerable:- Those taking doses above 20mg daily-risk jumps 3.2 times compared to 10mg
- People with a history of depression, anxiety, or bipolar disorder-their risk is nearly five times higher
- Older adults, especially those over 65, whose brains process drugs differently
- Anyone on prednisone for more than two weeks
What to Do Right Now
If you’re experiencing mood swings, don’t wait. Don’t assume it’ll pass. Don’t blame yourself. Call your doctor. Tell them exactly what you’re feeling: “I’ve been crying for no reason,” “I’m snapping at my family,” “I can’t sleep,” “I had a panic attack.” Don’t sugarcoat it. Write it down if you need to. Your doctor might:- Adjust your dose
- Change your timing (taking it in the morning helps with sleep)
- Speed up your taper
- Refer you to a psychiatrist
Proven Coping Strategies That Actually Work
While you’re waiting for your doctor’s advice-or if you’re stuck on prednisone for now-here’s what helps:1. Stick to a Sleep Schedule
Prednisone wrecks your circadian rhythm. That makes everything worse. Go to bed and wake up at the same time every day-even on weekends. No screens an hour before bed. Keep your room cool and dark. A 2022 study showed consistent sleep reduced mood swings by 40% in steroid users.2. Move Your Body
You don’t need to run a marathon. Thirty minutes of walking, cycling, or yoga daily cuts cortisol levels by 27%. Movement doesn’t just burn stress-it rebuilds your sense of control. One patient on MyCrohnsAndColitisTeam said, “I started walking after dinner. For the first time in weeks, I felt like me again.”3. Keep a Mood Journal
Write down:- What time of day you felt bad
- What you were doing
- What you ate
- How much you slept
4. Talk to Someone You Trust
Tell your partner, parent, or close friend: “I’m on prednisone. It’s making me irritable and anxious. I’m not myself. I need your patience.” Most people will understand. One study found that patients who communicated openly with family reported 43% less emotional distress.5. Try Mindfulness
Fifteen minutes of guided meditation twice a day-using apps like Insight Timer or Headspace-can calm your nervous system. You’re not trying to “think positive.” You’re just learning to sit with the feeling without reacting. A 2023 review in the Journal of Clinical Psychiatry found mindfulness reduced steroid-induced anxiety by 35%.6. Avoid Alcohol and Caffeine
Both make mood swings worse. Alcohol depresses your brain, then causes rebound anxiety. Caffeine spikes cortisol and disrupts sleep. Swap coffee for herbal tea. Skip the wine after dinner.When to Seek Emergency Help
Mood swings can turn dangerous. Get help immediately if you:- Have thoughts of hurting yourself or others
- Feel detached from reality (hallucinations, delusions)
- Can’t stop crying or feel completely numb
- Experience chest pain, rapid heartbeat, or trouble breathing





13 Comments
Alex Hundert
October 30 2025I didn't know prednisone could do this to your head. My sister went through it last year and I thought she was just stressed. Turns out she was basically on a chemical rollercoaster. I wish someone had told us. Now I just sit with her when she cries and don't try to fix it. Sometimes that's all you can do.
Emily Kidd
October 31 2025omg yes the crying in the shower thing. i thought i was going crazy. then i remembered i was on prednisone and just started yelling at the mirror like 'this isnt me this is the drug' and it helped a little. also sleep schedule is a game changer. no more 3am panic spirals.
Justin Cheah
November 1 2025They don't warn you because they don't want you to stop taking it. Pharma knows this stuff happens but they'd rather you suffer in silence than lose billions in sales. I read a leaked internal memo once - they call it 'collateral emotional damage.' That's not a side effect, that's corporate negligence. And now they're pushing mindfulness apps like it's a cure. Wake up. This is chemical assault disguised as treatment.
caiden gilbert
November 3 2025It's like your brain turns into a broken radio - static one minute, loud music the next, then silence. No volume control. I started walking at dawn just to feel something real. The world felt like it was underwater until I moved. Didn't fix it, but made it bearable. Also, coffee is the devil. Switched to chamomile. My partner said I stopped looking like I was about to scream at a cloud.
phenter mine
November 3 2025so true about the mood journal! i started writng down what i ate and when i got mad and wow it was crazy how much sugar made it worse. also i kept misspelling 'prednisone' as 'prednison' and my dr still got it. she was so nice about it. thanks for this post it made me feel less alone.
Aditya Singh
November 4 2025While the emotional lability is well-documented in the context of glucocorticoid receptor agonism and HPA axis dysregulation, the cited studies lack proper effect size normalization. The 47% figure is misleading without stratification by cumulative dose and duration. Also, mindfulness? That's a placebo intervention with low ecological validity. What you need is pharmacological modulation of limbic glutamatergic transmission, not guided breathing. And no, yoga won't reset your cortisol feedback loop.
Katherine Reinarz
November 5 2025my husband left me because of this. he said i was 'unrecognizable.' i broke three plates and screamed at the dog. now i'm alone and he's with someone else. i just want to know if i'll ever be me again. please tell me i'm not broken forever.
John Kane
November 6 2025Hey, I'm not a doctor, but I've been on prednisone for over a year for my autoimmune condition, and I want you to know: you're not alone. I cried in the grocery store once because I couldn't find almond milk. My kid just hugged me and said 'it's okay, Mommy's brain is on medicine.' That hit me harder than any pill. The mood swings don't define you. You're still the same person who laughs too loud at dog videos and forgets where you put your keys. The drug's just borrowing your brain for a while. And it's gonna give it back. I promise. Keep going. You're doing better than you think.
Callum Breden
November 6 2025This article is dangerously oversimplified. The term 'mood swings' trivializes the neurochemical disruption caused by exogenous corticosteroids. Furthermore, recommending mindfulness as a primary intervention is clinically irresponsible. The assertion that symptoms resolve within 14 days post-taper is not supported by longitudinal data. Many patients experience prolonged neuropsychiatric sequelae. The author exhibits a profound lack of medical rigor. This is not advice. It is anecdotal fluff masquerading as clinical guidance.
Mansi Gupta
November 8 2025Thank you for writing this with such care. I’ve been on a low dose for 10 months and the emotional fog is real. I didn’t speak up because I didn’t want to seem ungrateful for the medication that keeps me alive. But your point about asking for help - it’s not weakness. It’s stewardship of your own body. I started journaling too. And I’m seeing a therapist now. It’s not about fixing the mood. It’s about not drowning in it.
Erin Corcoran
November 10 2025YESSSS this is me 😭 I thought I was just being a bad person until I read this. I cried at a commercial for toothpaste. My dog looked at me like I'd betrayed him. Now I take my prednisone with breakfast, no caffeine after noon, and I do 10 mins of breathwork with the Insight Timer app. It's not perfect but I'm not screaming at my cat anymore 🙏
shivam mishra
November 12 2025As someone who's managed steroid-induced mood changes for 6 years with ulcerative colitis, I can confirm: sleep timing is everything. Taking prednisone before 8am reduces nighttime cortisol spikes by 60%. Also, omega-3 supplementation (EPA/DHA 2g/day) has shown neuroprotective effects in multiple RCTs. Don't underestimate the power of magnesium glycinate for anxiety. And yes, talking to someone who's been there? Lifesaver. You're not broken. You're pharmacologically altered. Big difference.
Scott Dill
November 13 2025One sentence: I yelled at my mom for 20 minutes because she didn't fold the towels right. Then I apologized, cried, and took a nap. I'm not crazy. It's the medicine. And I'm gonna beat this.