Menstrual Cycle Phases Explained: How They Influence Ovulation & Period Regulation
Menstrual Cycle Phase Tracker
Enter your cycle details to see how your menstrual cycle phases align with hormone changes and fertility windows.
Quick Takeaways
- The menstrual cycle is split into four main phases, each driven by distinct hormone spikes.
- Follicular phase builds the egg; ovulatory phase releases it; luteal phase prepares the lining; menstruation sheds the lining if pregnancy doesn’t occur.
- Estrogen peaks early, progesterone dominates later - tracking these hormones helps predict fertile windows.
- Lifestyle factors like stress, sleep, and nutrition can shift phase lengths and affect regularity.
- Understanding the cycle empowers you to manage symptoms, plan conception, or simply know what’s normal.
What the Menstrual cycle is the monthly series of hormonal and physiological changes that prepare a woman's body for pregnancy actually looks like
Most people hear about periods and ovulation, but the menstrual cycle phases are a coordinated dance of hormones, eggs, and uterine tissue. A typical cycle lasts about 28 days, but anywhere from 21 to 35 days is normal. The key is that the cycle repeats in a predictable pattern, allowing the body to fine‑tune its readiness for conception.
The Follicular phase the first half of the cycle, starting on day1 of menstruation and ending just before ovulation
Day1 marks the first day of bleeding. During the follicular phase, the pituitary gland releases Follicle‑Stimulating Hormone (FSH) a hormone that stimulates the growth of ovarian follicles. A handful of follicles awaken, but usually only one becomes dominant.
As the dominant follicle grows, it produces increasing amounts of Estrogen the primary female sex hormone that thickens the uterine lining and regulates other hormones. Rising estrogen levels do two things: they rebuild the endometrium after the previous period and they signal the brain to reduce FSH output, narrowing the competition to a single follicle.
Typical duration: 10‑14days, but it can be shorter if hormonal imbalances speed up follicle maturation.
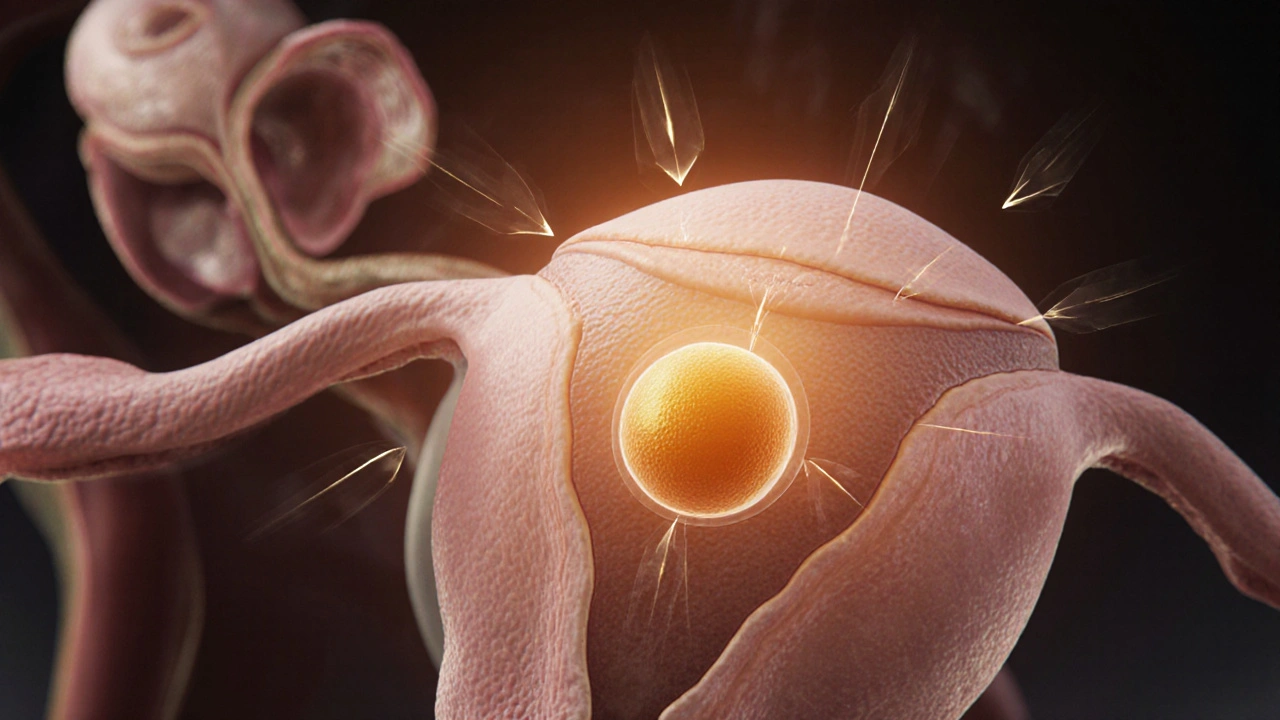
The Ovulatory phase the brief window, usually around day14, when the mature egg is released
When estrogen peaks, the pituitary switches gears and releases a surge of Luteinizing Hormone (LH) the hormone that triggers ovulation and the formation of the corpus luteum. This LH spike lasts only 24‑36hours and is the catalyst that ruptures the follicle, letting the egg travel down the fallopian tube.
The egg is viable for about 12‑24hours. If sperm meet the egg in that window, fertilization can occur; otherwise the egg disintegrates.
Tracking the LH surge with ovulation kits or monitoring basal body temperature can pinpoint this fertile window with impressive accuracy.
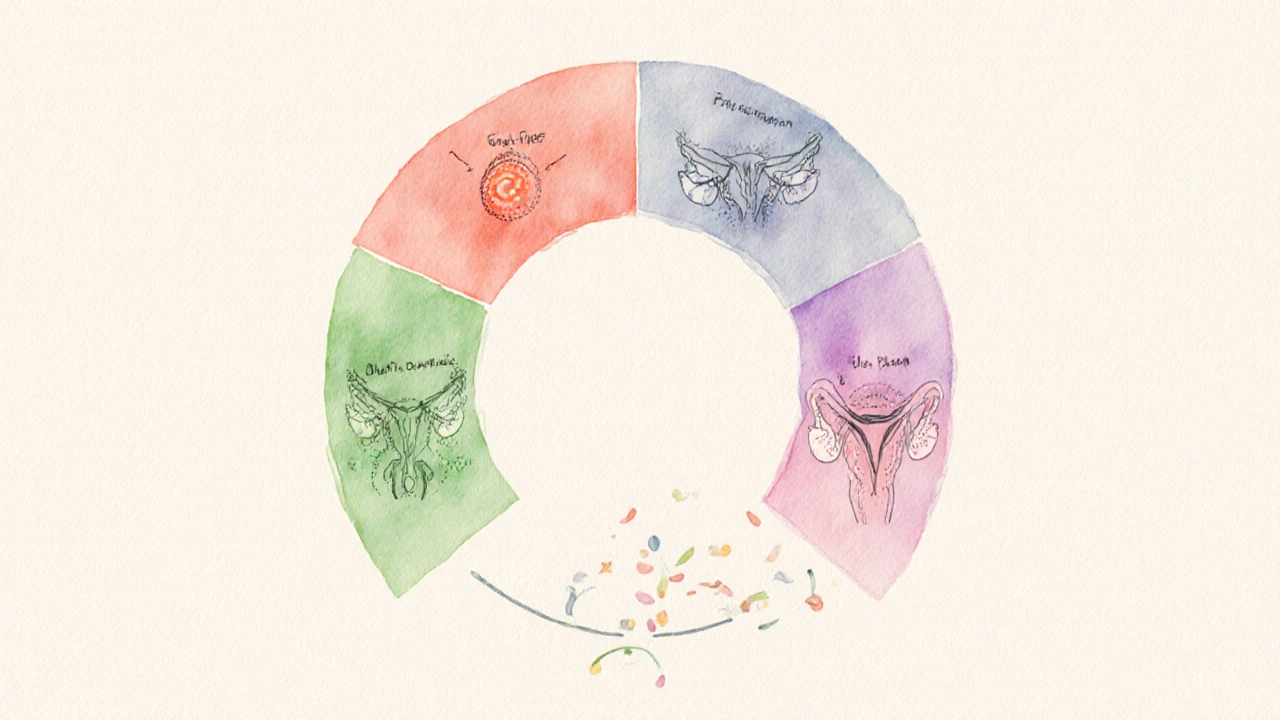
The Luteal phase the post‑ovulation period when the ruptured follicle transforms into the corpus luteum
After the egg departs, the empty follicle becomes the Corpus luteum a temporary endocrine structure that secretes progesterone and moderate estrogen. Progesterone rises sharply, stabilizing the thickened uterine lining and creating a hospitable environment for a potential embryo.
If pregnancy doesn’t happen, the corpus luteum degenerates around day22‑24, causing progesterone to drop. This hormonal decline triggers the next menstrual bleed.
Typical luteal length is remarkably consistent-about 14days-making it a reliable marker for cycle regularity.
The Menstruation the shedding of the uterine lining that marks the start of a new cycle
When progesterone falls, blood vessels in the endometrium constrict, and the lining sloughs off. This results in the familiar period, lasting anywhere from 3 to 7days. Iron loss during menstruation can affect energy levels, which is why many people feel a dip in stamina.
While the amount of blood varies, the average is about 30‑40ml per month-roughly two to three teaspoons. Keeping a simple log of flow, pain, and mood can reveal patterns that signal underlying issues like hormonal imbalance or polycystic ovary syndrome (PCOS).
Hormonal Interplay: How Estrogen, Progesterone, FSH, and LH Shape the Cycle
The four hormones mentioned above form a feedback loop. Early in the follicular phase, low estrogen tells the brain to release more FSH. As estrogen climbs, the brain switches to releasing LH, which then causes ovulation. After ovulation, rising progesterone tells the brain to stop both FSH and LH, completing the loop.
Disruptions-whether from stress, illness, or endocrine disorders-can blunt these signals, leading to irregular periods, missed ovulation, or heavy bleeding. Understanding where a symptom fits in the hormonal cascade helps pinpoint the right intervention.
Practical Tips to Keep Your Cycle on Track
- Track daily: Use a simple notebook or an app to record bleeding, basal temperature, and any noticeable cervical mucus changes.
- Balance nutrition: Adequate iron (spinach, lentils), B‑vitamins, and omega‑3 fatty acids support hormone synthesis.
- Prioritize sleep: 7‑9hours a night keeps the hypothalamic‑pituitary axis stable.
- Manage stress: Mind‑body practices (yoga, meditation) lower cortisol, which otherwise interferes with LH surges.
- Exercise smart: Moderate activity promotes circulation, but extreme training can suppress FSH and LH, causing missed periods.
If you notice persistent irregularities-cycles shorter than 21days or longer than 35days, very heavy bleeding, or painful cramps beyond the first few days-consult a healthcare professional. Tests for hormone levels, ultrasound imaging of the ovaries, or screening for thyroid function can uncover hidden causes.
Phase‑by‑Phase Summary Table
| Phase | Days (typical) | Dominant Hormone(s) | Main Physiological Events |
|---|---|---|---|
| Follicular | 1‑13 | Estrogen ↑, FSH | Follicle growth, endometrial rebuilding |
| Ovulatory | 14‑15 | LH surge, brief estrogen peak | Egg release, peak fertility |
| Luteal | 16‑28 | Progesterone ↑, moderate estrogen | Corpus luteum formation, lining maintenance |
| Menstruation | 1‑7 (overlaps start of next follicular) | Progesterone ↓, estrogen low | Shedding of uterine lining |

Frequently Asked Questions
Why does my cycle sometimes feel longer or shorter than 28 days?
Cycle length can shift due to stress, changes in weight, travel across time zones, or underlying conditions like thyroid disorders. The follicular phase is the most flexible part; a shorter follicular phase shortens the whole cycle, while the luteal phase stays around 14days.
Can I predict ovulation without kits?
Yes. Track basal body temperature (it rises ~0.5°C after ovulation) and monitor cervical mucus (clear, stretchy “egg‑white” mucus peaks with estrogen). Combining both signs gives a reliable natural forecast.
What does a "short luteal phase" mean for fertility?
A luteal phase shorter than 10days may not allow enough progesterone to fully support implantation, lowering the chance of pregnancy. Lifestyle adjustments and, in some cases, progesterone supplementation can help extend it.
Why is my period heavier some months?
Hormonal spikes, especially a sudden estrogen drop, can cause the endometrium to build thicker than usual, leading to heavier bleeding. Consistent heavy flow (>80ml) warrants a check for fibroids, polyps, or coagulation issues.
How does birth control alter these phases?
Combined hormonal contraceptives supply steady estrogen and progestin, suppressing the natural FSH/LH surge. This prevents follicle development and ovulation, turning the cycle into a withdrawal bleed rather than a true menstrual phase.




18 Comments
Hannah M
September 30 2025Wow, this breakdown really helped me see how everything fits together! 😊 The way you explained the hormone spikes makes the whole cycle feel less mysterious. I especially love the tip about tracking basal temperature and mucus – it’s something I’ll start doing tonight. Thanks for making such a dense topic approachable. Keep the great posts coming! 🌸
Yareli Gonzalez
October 1 2025I appreciate the clear overview of each phase.
Carl Mitchel
October 1 2025While the article is thorough, it overlooks a key point about luteal phase variability. Most textbooks claim a fixed 14‑day luteal phase, yet real‑world data shows a noticeable spread of 10‑16 days depending on individual progesterone metabolism. Ignoring this nuance can mislead those trying to pinpoint their fertile window. Moreover, the piece could have mentioned that stress‑induced cortisol can suppress the LH surge, extending the follicular phase. It also fails to address how thyroid disorders subtly shift cycle length by altering basal metabolic rate. A brief note on the impact of insulin resistance would have rounded out the hormonal interplay section. Lastly, the advice to “use an app” assumes universal access to smartphones, which isn’t always the case.
Josh SEBRING
October 1 2025Interesting take, but it feels like you’re just regurgitating textbook facts without any real-world context. People dealing with PCOS or endometriosis won’t find this "one‑size‑fits‑all" guide helpful.
Lily Tung
October 1 2025This article attempts to be comprehensive yet it repeatedly falls into the trap of oversimplification. It states that the follicular phase lasts ten to fourteen days but then contradicts itself by assigning a fixed day count for ovulation regardless of individual variation. The language used is peppered with vague phrases such as "typically" and "often" which do little to clarify the uncertainty inherent in menstrual physiology. Additionally the piece fails to acknowledge that hormone levels are not static spikes but rather dynamic gradients that fluctuate even within a single day. While the table provides a quick reference, it omits essential information about the role of inhibin in feedback regulation. The mention of iron loss is accurate but lacks depth regarding the impact on hemoglobin synthesis and overall energy metabolism. The advice to track basal body temperature is sound, however the article neglects to discuss the influence of sleep disturbances on temperature readings. The recommendation for omega‑3 fatty acids is relevant, yet it does not differentiate between plant‑based ALA and marine EPA/DHA, which have distinct effects on prostaglandin synthesis. The section on birth control simplistically reduces hormonal contraceptives to "steady estrogen and progestin" without addressing the diversity of formulations and their varying impacts on cycle suppression. Finally the article could benefit from citing recent meta‑analyses that examine the relationship between stress biomarkers and cycle irregularity. Overall the content is useful as a primer but would be greatly enhanced by incorporating these nuances.
Taryn Bader
October 1 2025I love the vibe of this guide, it feels like a friend walking you through a confusing topic. The simple language makes it easy to follow.
Myra Aguirre
October 2 2025Good summary, especially the quick takeaways. I’ll try the tracking suggestions. Thanks for the info.
Shawn Towner
October 2 2025While the summary is handy, it glosses over the fact that not everyone experiences a clean 5‑day bleed. Some have spotting that can confuse tracking efforts.
Ujjwal prakash
October 2 2025Wow, what a detailed piece! I love how you broke down each hormone, the way estrogen rises, peaks, and then dips – it’s fascinating, really. The table is a great visual aid, and the tips on lifestyle factors are spot‑on – especially the stress‑sleep‑nutrition triad, which many overlook. Also, your note on using basal temperature alongside cervical mucus is solid; those two together give a much clearer picture of ovulation than any single method alone. Keep up the excellent, thorough work!
Diane Helene Lalande
October 2 2025Great job on summarizing the phases. One extra tip: logging mood changes alongside your physical symptoms can help spot patterns linked to estrogen or progesterone shifts. This can be especially useful for identifying pre‑menstrual syndrome trends.
Edwin Levita
October 3 2025Honestly, reading this felt like watching a drama unfold – the rise and fall of hormones is like a theatrical performance! The ovulation climax is the dramatic high point, and the luteal phase is the brooding act before the tragic end of menstruation. I wish there were more emphasis on the emotional roller‑coaster that accompanies these hormonal shifts.
Xander Laframboise
October 3 2025Your dramatic analogy is nice but let’s get real – hormone levels are measurable data, not just emotions. The luteal phase’s progesterone isn’t “brooding,” it’s physiologically essential for endometrial preparation. Over‑romanticizing can mislead readers about the clinical importance of tracking.
Jason Petersen
October 3 2025The data seems solid however i think more references would help
Melissa Gerard
October 3 2025Nice effort, but could use more depth 🤷♀️
Cindy Knox
October 4 2025I really appreciate the friendly tone of this guide – it feels welcoming and supportive. The way you broke down each phase into bite‑size pieces makes it less intimidating. I especially love the practical tips about nutrition and stress management; they’re exactly what many of us need. Keep sharing these helpful resources, they truly make a difference!
beverly judge
October 4 2025Thanks for the comprehensive overview. For those wanting a deeper dive, consider reading recent reviews on the impact of environmental endocrine disruptors on cycle regularity. They add an important layer to the discussion.
Capt Jack Sparrow
October 4 2025Fact check: the luteal phase is consistently about 14 days, give or take a day or two – that’s why it’s such a reliable marker for cycle tracking.
Manju priya
October 4 2025Excellent synthesis of complex information; I encourage readers to implement the tracking suggestions for better health outcomes. 😊