Gout and the Immune System: Essential Facts & Management
Gout Risk Assessment Tool
Assess Your Gout Risk Factors
Answer the following questions to determine your risk level for developing gout.
Your Gout Risk Assessment
Quick Takeaways
- gout is triggered by uric‑acid crystals that set off a powerful immune response.
- The NLRP3 inflammasome and cytokines such as IL‑1β drive the painful swelling.
- Diet, alcohol, obesity and genetics all influence uric‑acid levels.
- Long‑term control relies on lowering uric acid (allopurinol, febuxostat) and managing flare‑ups (colchicine, NSAIDs).
- Addressing underlying inflammation reduces the risk of kidney and heart complications.
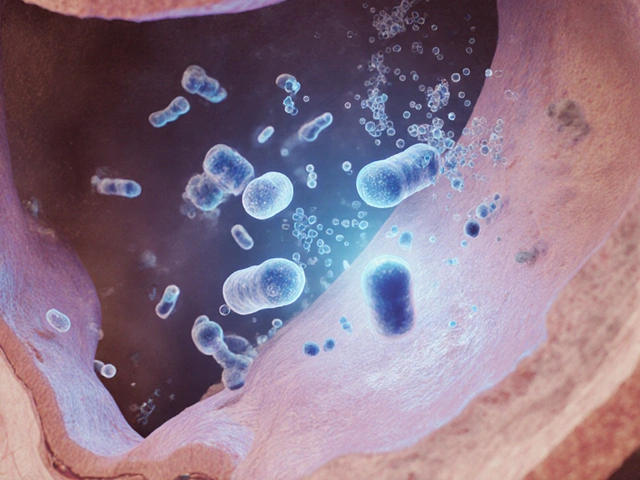
Understanding how gout is a form of inflammatory arthritis that erupts when uric acid builds up in the blood, forms monosodium urate crystals, and lodges in joints. Those tiny crystals aren’t just annoying; they act like an alarm bell for your body’s defense system. When the immune system the network of cells and proteins that protects you from infection and injury spots the crystals, it launches a cascade of inflammation that makes the toe-or any affected joint-red, hot, and excruciatingly painful.
Why the Immune System Gets It Wrong
The key player is the NLRP3 inflammasome a protein complex inside immune cells that detects danger signals and activates inflammatory pathways. When monosodium urate (MSU) crystals settle in a joint, they trigger NLRP3, which then releases the cytokine IL‑1β a potent messenger that amplifies pain and swelling. IL‑1β recruits more white blood cells, especially neutrophils, which try to engulf the crystals but end up causing tissue damage.
Other cytokines-TNF‑α, IL‑6, and interferon‑γ-join the party, creating a feedback loop that sustains the attack. This explains why a single crystal deposit can produce days of agony, and why repeated attacks can lead to chronic joint damage.
How Uric Acid Levels Rise
Uric acid is the end product of purine metabolism. Purines are found in high‑protein foods (red meat, organ meats), certain seafood (anchovies, sardines), and alcoholic beverages (beer, spirits). Your liver turns purines into uric acid, which then travels through the bloodstream to the kidneys for excretion.
When production outpaces elimination, hyperuricemia blood uric‑acid concentration above 6.8mg/dL, the solubility limit for uric acid occurs. The excess crystallizes, especially in cooler areas like the big toe, and the immune system reacts.
Common contributors:
- Genetics: about 30% of uric‑acid handling is inherited.
- Kidney impairment: reduced filtration keeps uric acid in the bloodstream.
- Obesity: excess visceral fat raises insulin resistance, which hampers uric‑acid excretion.
- Medications: diuretics, low‑dose aspirin, and some chemotherapy agents increase levels.

From Acute Flare to Chronic Gout
An acute flare is the body’s rapid response to new crystal formation. If the underlying hyperuricemia isn’t addressed, crystals accumulate, leading to tophi-chalky deposits under the skin-and chronic joint inflammation.
Chronic gout isn’t just a joint problem. Long‑term inflammation raises the risk of cardiovascular disease, chronic kidney disease, and metabolic syndrome. Studies from the British Society for Rheumatology (2023) show that patients with untreated gout have a 25% higher chance of developing hypertension.
Managing the Immune Response
Effective gout care has two tracks: short‑term flare control and long‑term uric‑acid lowering. Both rely on taming the immune system.
Fast‑Acting Options
- Colchicine: interferes with neutrophil migration, dampening the inflammatory surge. Typical dose is 1.2mg then 0.6mg an hour later.
- NSAIDs (e.g., ibuprofen, naproxen): inhibit COX enzymes, reducing prostaglandin‑mediated pain.
- Corticosteroids (oral or intra‑articular): blunt the entire cytokine cascade, useful when NSAIDs or colchicine are contraindicated.
Uric‑Acid‑Lowering Therapies
These drugs act upstream, preventing crystal formation and thus the immune trigger.
| Medication | Mechanism | Typical Dose | Key Benefits | Common Side Effects |
|---|---|---|---|---|
| Allopurinol | Xanthine oxidase inhibition (reduces uric‑acid production) | 100mg daily, titrated up to 300mg | Proven long‑term control, inexpensive | Rash, rare Stevens‑Johnson syndrome |
| Febuxostat | Selective xanthine oxidase inhibition | 40‑80mg daily | Effective in allopurinol‑intolerant patients | Liver enzyme elevation, cardiovascular caution |
| Colchicine | Disrupts microtubule formation, blocks neutrophil activity | 1.2mg then 0.6mg, may continue low‑dose | Rapid flare relief, low cost | GI upset, rare muscle toxicity |
| NSAIDs (e.g., Ibuprofen) | COX‑1/COX‑2 inhibition (reduces prostaglandins) | 400‑800mg every 6‑8h | Fast pain relief | Stomach ulcer, kidney strain |
Choosing the right regimen depends on kidney function, heart health, and other medications. A common strategy is to start colchicine or an NSAID for the flare, then begin allopurinol or febuxostat to keep uric acid below 6mg/dL.
Lifestyle Tweaks That Calm the Immune Reaction
Even with medication, diet and habits influence the immune system’s baseline tone.
- Hydration: Aim for 2‑3L of water daily; urine dilution helps excrete uric acid.
- Limit purine‑rich foods: Reduce red meat, organ meats, and certain seafood.
- Alcohol moderation: Beer and spirits raise uric acid; wine is less risky but still should be limited.
- Weight management: Losing 5‑10% of body weight can drop uric‑acid levels by up to 1mg/dL.
- Vitamin C: 500mg daily may modestly boost uric‑acid clearance.
Regular low‑impact exercise improves insulin sensitivity, which indirectly helps the kidneys clear uric acid.

When to Seek Medical Help
If you notice any of the following, contact a healthcare professional promptly:
- Sudden, severe joint pain lasting >24hours.
- Swelling that doesn’t improve with OTC NSAIDs.
- Fever, chills, or red streaks spreading from the joint.
- Kidney‑related symptoms (blood in urine, flank pain).
Early intervention can prevent tophi formation and reduce long‑term organ damage.
Putting It All Together: A Simple Plan
- Confirm diagnosis: Blood test for uric acid, joint aspiration if needed.
- Start flare control: Colchicine 1.2mg → 0.6mg, or NSAID.
- Begin uric‑acid‑lowering drug: Allopurinol 100mg daily, titrate.
- Track levels: Re‑check serum uric acid every 2‑4weeks until <6mg/dL.
- Adopt lifestyle habits: Hydrate, trim purines, exercise.
- Review annually: Adjust meds based on kidney function and cardiovascular risk.
Following these steps keeps the immune system from over‑reacting to crystal deposits, cuts pain, and lowers the chance of heart or kidney complications.
Frequently Asked Questions
Can gout be cured completely?
Gout can be fully controlled, but the underlying tendency to produce uric acid often remains. Ongoing medication and lifestyle changes keep crystal formation at bay, making flare‑ups rare.
Why does gout often affect the big toe?
The big toe is cooler than the core body temperature, so uric‑acid crystals are more likely to precipitate there. The joint’s limited blood flow also makes it a prime spot for crystal buildup.
Is it safe to take allopurinol if I have kidney disease?
Allopurinol doses are usually reduced for moderate kidney impairment, and kidney function is monitored closely. In severe cases, febuxostat may be a better option.
Can I use natural remedies instead of prescription meds?
Herbal or supplement approaches (cherries, vitamin C) may lower uric acid modestly, but they rarely replace prescription therapy for people with frequent flares or high uric‑acid levels.
How long does a gout flare usually last?
Without treatment, a flare can persist 5‑10days. With colchicine or NSAIDs, most people feel major relief within 24‑48hours.





14 Comments
Hardy D6000
October 8 2025The narrative that gout is merely a harmless inconvenience is a thin veneer; it's really an engineered excuse for the pharma industry to push aggressive uric‑acid‑lowering drugs onto unsuspecting Americans, and we should be skeptical of that agenda.
Amelia Liani
October 18 2025Reading this, I can almost feel the collective sigh of relief from those who've wrestled with that searing, burning pain-gout is no joke, and the way you broke down the immune connection really shines a light on how much our bodies are trying to tell us when we ignore the warning signs.
shikha chandel
October 29 2025Only a privileged few recognize that elevated uric acid is a deliberate biomarker of hidden metabolic manipulation.
Zach Westfall
November 8 2025I swear gout feels like a thousand tiny volcanoes erupting inside your toe-pain so intense it makes you question reality!
Pranesh Kuppusamy
November 18 2025In the grand tapestry of human physiology, gout emerges as a paradoxical sentinel, warning us of deeper metabolic discord.
It is not merely a disease of excess purines; it is a manifestation of the body's struggle to maintain homeostasis in the face of evolutionary pressure.
When uric acid crystals deposit within joints, they act as microscopic flags, signalling that the kidneys are failing to excrete waste efficiently.
This crystalline intrusion sets off a cascade of innate immune activation, recruiting neutrophils that unleash a barrage of inflammatory mediators.
The resulting edema and excruciating pain serve as a visceral reminder that the internal milieu is out of balance.
Philosophically, one might view gout as the body's own courtroom, where the jury of cytokines delivers verdicts on lifestyle choices and genetic predisposition.
Yet, the modern medical establishment often reduces this complex dialogue to a simple prescription for allopurinol, ignoring the nuanced interplay of diet, comorbidities, and environmental toxins.
Such reductionism reflects a deeper societal tendency to favor quick fixes over holistic understanding.
Furthermore, the immune response in gout is a double‑edged sword; while it strives to clear crystal deposits, it also inflicts collateral damage upon the surrounding tissue.
This paradox underscores the delicate equilibrium that must be maintained between defense mechanisms and self‑preservation.
Consequently, management strategies should extend beyond pharmacology to encompass dietary modification, weight control, and renal health monitoring.
Only by addressing the root causes can we hope to restore the fragile equilibrium and prevent recurrent attacks.
In this light, the immune system is not an adversary but a partner that, when properly guided, can facilitate healing.
Thus, the essential facts about gout and immunity are not isolated bullet points, but interconnected threads weaving a larger narrative about human health.
Recognizing this interdependence empowers patients and clinicians alike to adopt a more comprehensive, preventive approach.
Ultimately, the battle against gout is a collaborative venture between mind, body, and the microscopic guardians of our immune system.
Crystal McLellan
November 29 2025They dont tell u that the labs are rigged to make uric acid look high so they can sell more meds.
Kelly Thomas
December 9 2025If you’re looking for practical steps, start by cutting back on red meat, organ meats, and sugary drinks-those are the biggest culprits for raising uric acid.
Swap them for low‑purine proteins like chicken breast or tofu, and hydrate with plenty of water throughout the day.
Adding a handful of cherries or a splash of vitamin C can also help your body flush out excess uric acid.
When a flare does strike, a short course of colchicine or an NSAID can tame the inflammation, but always check with your doctor before starting any medication.
Consistency is key: keep a food diary, monitor your weight, and get your kidney function checked annually.
These colorful tweaks can turn the tide and keep gout from hijacking your life.
Mary Ellen Grace
December 19 2025Whoa, that’s a lot of info!
Carl Watts
December 30 2025Think of gout as a microcosm of existential tension: the body posits a problem, the immune system answers, and the individual is left to interpret the pain.
In this dance, each flare is a stanza in a poem written by our metabolism.
Brandon Leach
January 9 2026Sure, because we all love a good poetic explanation when our toe hurts like hell.
Alison Poteracke
January 19 2026Managing gout doesn’t have to be a solo mission.
Talk to your primary care doctor about a uric‑acid test and ask about lifestyle changes that fit your routine.
Simple steps-like reducing alcohol, staying active, and eating more vegetables-can make a big difference.
Marianne Wilson
January 29 2026I must point out the glaring inconsistency in presenting gout as merely a “lifestyle issue” while ignoring the socioeconomic factors that limit access to healthy foods; it’s a disservice to readers and borders on moral negligence.
Patricia Bokern
February 9 2026OMG, this whole gout thing is like a secret government plot – they want us all terrified of our own bodies while they laugh and sell us endless meds!!!
It’s straight out of a dystopian novel and we’re the unsuspecting extras.
Garrett Gonzales
February 19 2026From a pharmacodynamic perspective, xanthine oxidase inhibitors such as allopurinol function by reducing the conversion of hypoxanthine to uric acid, thereby lowering serum uricemia.
Therapeutic drug monitoring is essential to avoid subtherapeutic dosing that could precipitate breakthrough flares.
Consideration of renal clearance is paramount; dose adjustments based on creatinine clearance mitigate the risk of accumulation and toxicity.
Adjunctive therapy with lesinurad can augment uricosuric pathways, but beware of potential drug–drug interactions with azathioprine.
Patient adherence improves when clinicians employ a treat‑to‑target strategy, aiming for serum uric acid <6 mg/dL.
Integration of dietary counseling with pharmacotherapy yields synergistic reductions in gout incidence.