Pharmacokinetic vs Pharmacodynamic Drug Interactions: What You Need to Know
Drug Interaction Checker
Check Medication Interactions
Interaction Results
When you’re taking more than one medication, it’s not just about what each pill does on its own. It’s about how they interact-and those interactions can mean the difference between effective treatment and a trip to the hospital. Two main types of drug interactions drive most of these risks: pharmacokinetic and pharmacodynamic. They sound like jargon, but they’re not. They’re the reason why your doctor checks your meds every time you come in.
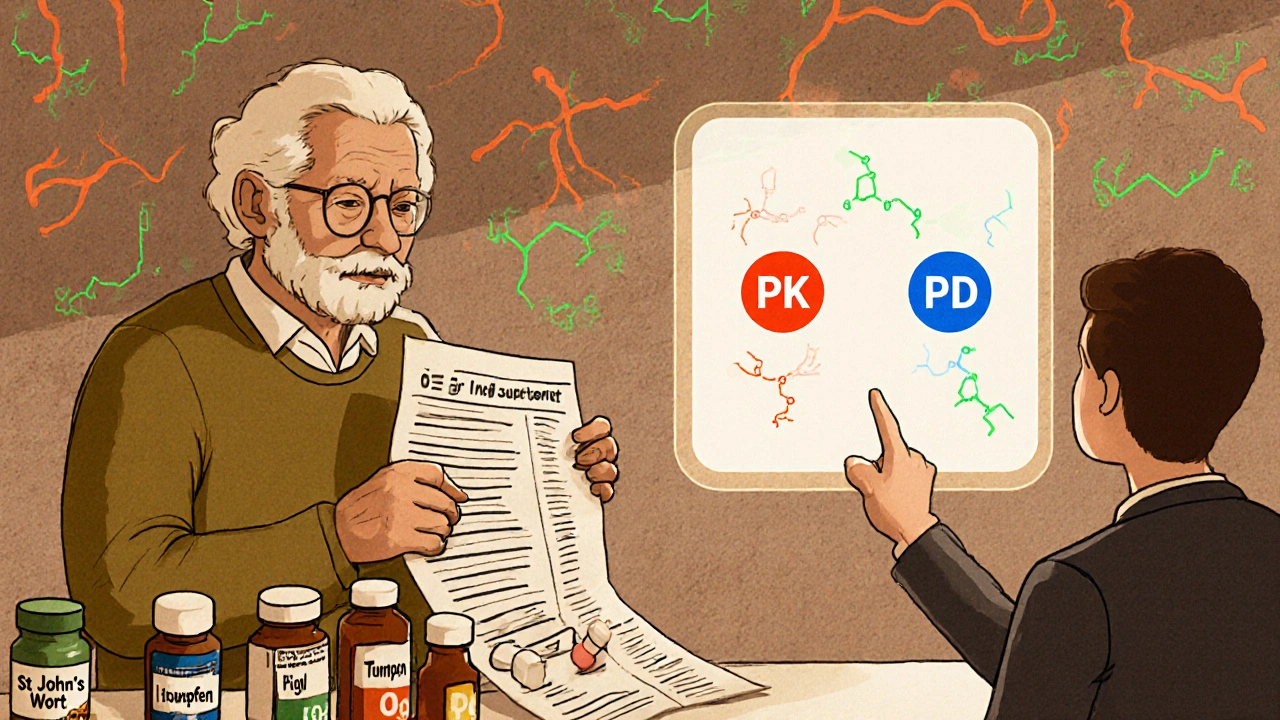
What Pharmacokinetic Interactions Really Mean
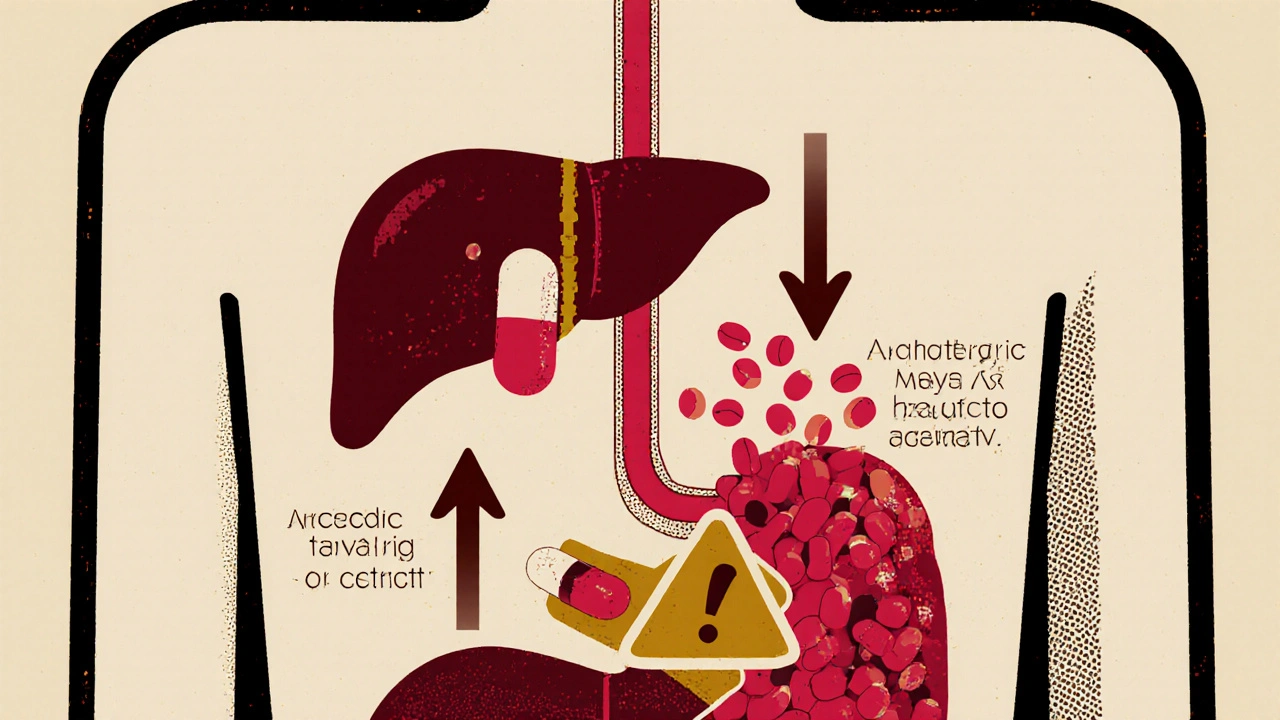
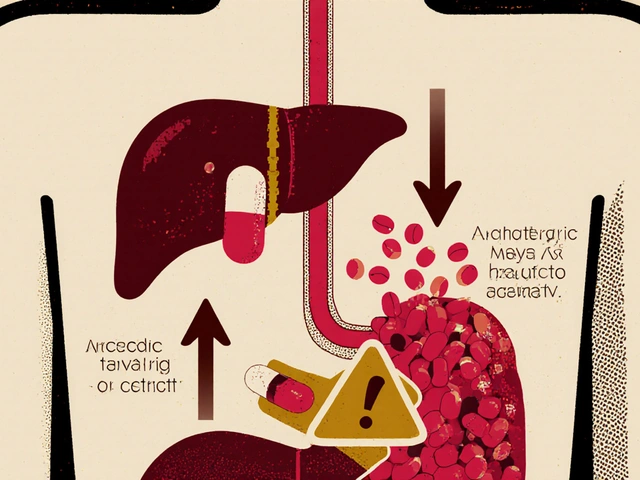
Pharmacokinetic interactions are all about what your body does to the drug. Think of it like a delivery system: how fast the drug gets into your bloodstream, where it goes, how long it stays, and how it leaves your body. These are the ADME steps-absorption, distribution, metabolism, excretion.One of the biggest players here is the liver, specifically the CYP3A4 enzyme. It’s responsible for breaking down about 50% of all prescription drugs. When another drug blocks or speeds up this enzyme, things go sideways. For example, if you take clarithromycin (an antibiotic) with simvastatin (a cholesterol drug), CYP3A4 gets shut down. Simvastatin builds up in your blood-up to 10 times higher than normal. That’s not just a tweak. That’s a high risk of muscle damage, even kidney failure.
It’s not just the liver. Antacids like Tums can stop antibiotics like ciprofloxacin from being absorbed. If you take them together, you might as well not take the antibiotic at all. Studies show absorption drops by 75-90%. That’s not a minor interaction-it’s a treatment failure.
Warfarin, the blood thinner, is another classic case. It sticks tightly to proteins in your blood. But if you add phenylbutazone (an old-school painkiller), it kicks warfarin off those proteins. Suddenly, you’ve got 300% more free warfarin floating around. That’s a recipe for dangerous bleeding. That’s why you can’t just add a new pill without checking.
What Pharmacodynamic Interactions Actually Do
Now, pharmacodynamic interactions are different. They don’t change drug levels. They change how your body responds to them. It’s like two people shouting at the same time-you can’t hear either one clearly.There are three kinds: additive, synergistic, and antagonistic.
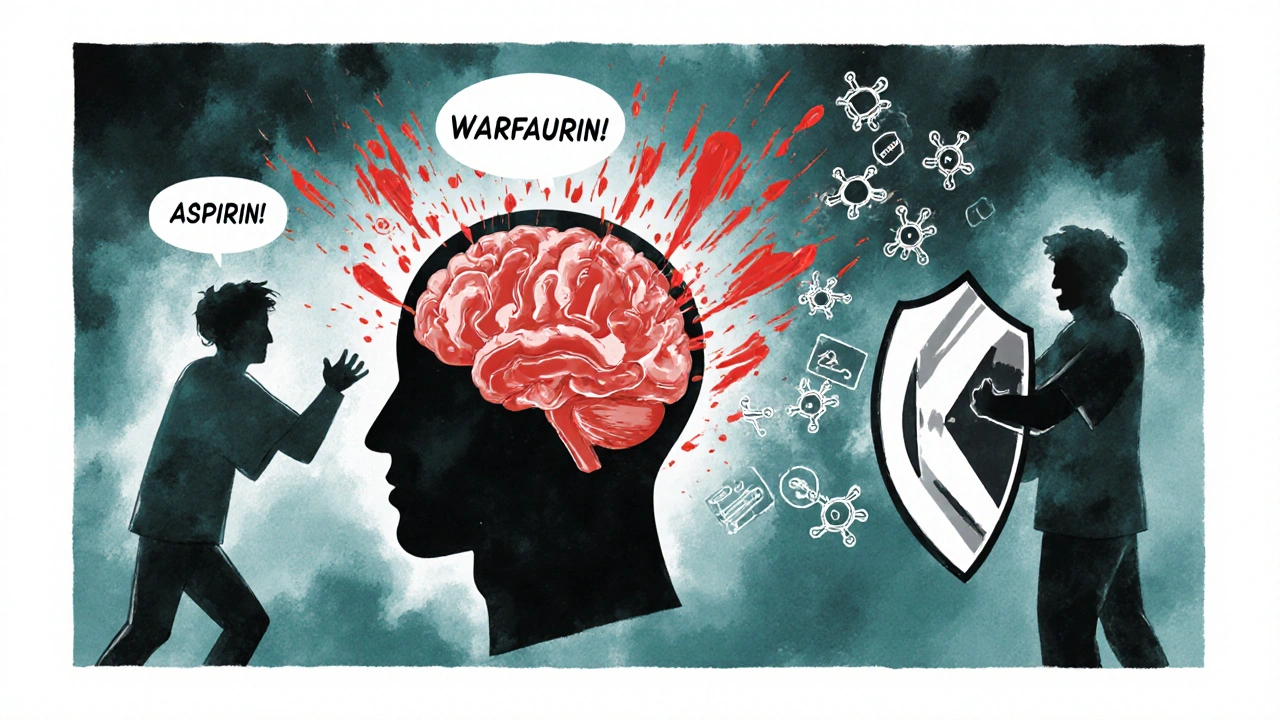
- Additive: Two drugs do the same thing, so their effects add up. Take warfarin and aspirin together? Both thin the blood. Your INR might climb to 4.0 or higher. That’s above the safe range. Bleeding risk goes up fast.
- Synergistic: Together, they do more than the sum of their parts. Sildenafil (Viagra) plus nitroglycerin? That’s a medical emergency. Both relax blood vessels. Together, they can drop your blood pressure so low you pass out-or worse.
- Antagonistic: One drug cancels out the other. Naloxone reverses opioid overdoses by kicking opioids off brain receptors. That’s lifesaving. But if you take a beta-blocker with a beta-agonist (like albuterol), they fight each other. Your asthma control suffers.
These interactions are especially common in the brain. Antidepressants, antipsychotics, and opioids often mix in dangerous ways. Serotonin syndrome, caused by mixing SSRIs with MAO inhibitors, can lead to fever, seizures, and even death. It doesn’t matter how much of each drug you take-what matters is that they’re both hitting the same system.
Why the Difference Matters for Treatment
Here’s the key: you manage these two types of interactions in totally different ways.With pharmacokinetic interactions, you can often fix the problem by adjusting the dose. If you need to take clarithromycin and simvastatin, your doctor won’t say “avoid it.” They’ll drop the simvastatin dose to 10mg. They’ll monitor your liver enzymes and muscle pain. It’s a trade-off, but it’s manageable.
With pharmacodynamic interactions, dose changes rarely help. If two drugs are fighting each other or amplifying each other too much, you can’t just lower the dose. You have to pick one. The UK’s Specialist Pharmacy Service says 78% of serious CNS drug interactions are pharmacodynamic-and most require avoiding the combo entirely.
Think about it this way: if you’re on an ACE inhibitor for blood pressure and start taking ibuprofen, the ibuprofen blocks the prostaglandins that help the ACE inhibitor work. Your blood pressure doesn’t drop as much. You might think the medicine isn’t working. But it’s not the dose-it’s the interaction. You need to switch to a different painkiller, like paracetamol.
Who’s Most at Risk?
Older adults are the most vulnerable. About 15% of people over 65 take five or more medications daily. That’s a recipe for interaction chaos. In the UK, 6.7% of hospital admissions are due to bad drug interactions. That’s tens of thousands of people every year.Narrow therapeutic index drugs are especially risky. These are medicines where the difference between a safe dose and a toxic one is tiny. Warfarin, digoxin, phenytoin, lithium-they all fall in this category. Pharmacokinetic interactions make up 68% of serious issues with these drugs.
But it’s not just the elderly. People with chronic conditions-diabetes, heart disease, depression-are often on multiple meds. A recent study found that 42% fewer adverse events happened when pharmacists reviewed all medications systematically. That’s not magic. That’s just knowing which interactions matter.
How Doctors and Pharmacists Spot These Interactions
It’s not guesswork. Tools exist. Electronic health records now flag over 2,200 high-risk interactions. Epic’s system alone lists 1,247 pharmacokinetic and 983 pharmacodynamic interactions based on the latest Flockhart Table.Therapeutic drug monitoring (TDM) helps with PK interactions. For drugs like phenytoin or vancomycin, your doctor checks your blood levels to make sure you’re in the safe range. If a new drug is added, they retest.
For PD interactions, they watch for signs. If you’re on multiple sedatives, they check your breathing. If you’re on blood thinners, they watch your INR. If you’re on heart meds, they check your blood pressure. It’s not just about labs-it’s about what you feel.
Pharmacogenomics is now part of the picture too. If you’re a slow metabolizer of CYP2D6, even a normal dose of codeine might not work-or might turn into too much morphine. The CPIC guidelines now list 32 gene-drug pairs that change how you respond to meds.
What You Can Do
You don’t need to be a scientist to stay safe. Here’s what works:- Keep a list of every medication you take-including supplements, OTC painkillers, and herbal products. Don’t assume they’re harmless.
- Ask your pharmacist every time you get a new prescription. “Will this interact with anything else I’m taking?” That’s a valid question.
- Watch for new symptoms after starting a new drug. Dizziness, confusion, unusual bruising, muscle pain, or sudden swelling? Tell your doctor immediately.
- Don’t mix alcohol with sedatives, antidepressants, or painkillers. It’s not just “a drink.” It’s a pharmacodynamic amplifier.
- Use one pharmacy if you can. They can track everything you’re taking and spot conflicts you might miss.
There’s no magic bullet. But understanding the difference between pharmacokinetic and pharmacodynamic interactions gives you power. You’re not just a patient. You’re part of the team keeping you safe.
What’s Changing Now
The science is moving fast. The FDA now requires testing for 11 CYP enzymes and 8 transporters-up from 7 just a few years ago. New biologic drugs, like immune checkpoint inhibitors, are showing unexpected PD interactions with immunosuppressants. Machine learning models are now predicting PD interactions with 89% accuracy-better than old tables.And the stakes are high. The WHO estimates that better management of these interactions could prevent 1.3 million adverse events worldwide by 2030. That’s not just numbers. That’s lives.
What’s the difference between pharmacokinetic and pharmacodynamic drug interactions?
Pharmacokinetic interactions change how your body handles the drug-how it’s absorbed, broken down, or cleared. Pharmacodynamic interactions change how the drug affects your body-like making effects stronger, weaker, or causing new side effects by targeting the same system.
Can you fix a pharmacokinetic interaction by changing the dose?
Yes, often you can. For example, if you need to take clarithromycin with simvastatin, your doctor might lower the simvastatin dose to 10mg instead of stopping it completely. Monitoring blood levels helps manage these safely.
Why are pharmacodynamic interactions harder to predict?
Because they don’t change drug levels-they change how your body responds. Two drugs might be fine alone, but together they can cause severe low blood pressure, serotonin syndrome, or breathing trouble. These effects depend on your physiology, not just chemistry.
Which drugs are most likely to cause serious interactions?
Drugs with a narrow therapeutic index-like warfarin, digoxin, phenytoin, and lithium-are high risk. So are CNS drugs like antidepressants, opioids, and benzodiazepines. Blood thinners, antibiotics, and statins also frequently cause interactions.
Can supplements cause drug interactions?
Absolutely. St. John’s wort can reduce the effectiveness of birth control, antidepressants, and blood thinners. Garlic and ginkgo can increase bleeding risk with warfarin. Even vitamin K can interfere with warfarin. Always tell your doctor what supplements you take.
How do pharmacists help prevent these interactions?
Pharmacists review your full medication list, check for known interactions using updated databases, flag high-risk combinations, and suggest safer alternatives. Studies show pharmacist-led reviews reduce adverse events by up to 42%.


11 Comments
Michael Harris
October 28 2025This is the kind of post that makes me want to scream at every GP who prescribes without checking interactions. I’ve seen patients on simvastatin and clarithromycin walk into the ER with rhabdo. Not because they were careless-because their doctor didn’t look past the script. CYP3A4 isn’t a suggestion, it’s a landmine. And don’t even get me started on how hospitals still let people take Tums with cipro. That’s not negligence, that’s malpractice by inertia.
Pharmacokinetics isn’t ‘jargon’-it’s the reason half the ICU is full of people who took perfectly fine drugs in perfectly fine doses. The system is broken, and we’re paying for it in muscle necrosis and kidney failure.
Stop calling it ‘medication management.’ Call it what it is: triage for people who didn’t get a real safety net.
Anna S.
October 29 2025It’s wild how we treat our bodies like vending machines-pop in a pill, get a result. But we’re not machines. We’re messy, biological poetry. And when you stack drugs on top of each other like Lego towers, you’re not just risking side effects-you’re disrespecting the entire rhythm of your own biology.
Warfarin and aspirin? That’s not ‘additive.’ That’s your blood saying ‘I’ve had enough.’
Why do we think we can outsmart evolution with a pharmacy receipt?
Maybe the real interaction isn’t between drugs-it’s between our arrogance and our mortality.
Prema Amrita
October 31 2025St. John’s wort is the silent killer in many households. I’ve seen elderly patients in rural India take it for ‘mood’ while on warfarin or digoxin. No one tells them. No one asks. The pharmacy doesn’t track it. The family thinks it’s ‘natural’ so it’s safe.
It’s not. Natural doesn’t mean harmless. The CYP enzymes don’t care if it’s a plant or a pill.
Always disclose supplements. Always. Even if it’s ‘just turmeric.’
Pharmacists are your last line of defense. Use them.
And if you’re on lithium? Never change your salt intake. That’s not a myth. That’s physiology.
Robert Burruss
October 31 2025I... I just... I mean, I didn’t realize that when you take ibuprofen with an ACE inhibitor, you’re not just ‘reducing efficacy’-you’re actively undermining the entire mechanism of action, and your body doesn’t even know it’s happening until your BP spikes, or your kidneys start to whisper… and by then, it’s too late… and you just… you just thought it was a headache… and now… I’m just… I’m just… overwhelmed… by how many things are silently, invisibly, happening inside us… every day… and we don’t even know…
Bryan Heathcote
October 31 2025Love this breakdown. I’m a med student and this is the exact stuff they skip in lectures. We get 10 minutes on drug interactions and then get tested on obscure side effects of drugs we’ll never prescribe.
But here’s the real kicker: the FDA now requires testing for 11 CYP enzymes? That’s insane. Most prescribers don’t even know what CYP3A4 stands for. We need mandatory pharmacogenomics training in med school. Like, right now.
Also-paracetamol over ibuprofen for hypertensives? That’s gold. I’m printing this and handing it to my grandma.
Snehal Ranjan
November 1 2025Dear Friends In The Global Community I Am Deeply Grateful For This Insightful Post Which Illuminates The Critical Nature Of Pharmacokinetic And Pharmacodynamic Interactions In Our Daily Health Practices In India Where Polypharmacy Is Common Among Elderly Populations And Access To Pharmacists Is Limited We Must Advocate For Community Pharmacies To Be Equipped With Basic Interaction Screening Tools And For Health Workers To Be Trained In Simple Medication Review Techniques Even A Single Question Asked By A Nurse Can Prevent A Catastrophe Let Us Not Wait For Technology To Save Us Let Us Begin With Compassion And Consistency In Every Interaction With Every Pill Every Supplement Every Drop Of Alcohol And Every Silent Patient Who Does Not Know To Ask
Sabrina Aida
November 2 2025Let’s be honest-this whole post is just pharmaceutical industry propaganda wrapped in a lab coat.
Who says we need to ‘manage’ interactions? Maybe the body knows better than your EHR. Maybe serotonin syndrome is just your soul trying to wake you up. Maybe lowering simvastatin dose is a cop-out for not addressing the root cause: your fear of death.
And why are we so afraid of drugs interacting? Maybe they’re supposed to. Maybe the body is a symphony, not a spreadsheet.
Why are we treating medicine like a puzzle to be solved instead of a mystery to be lived?
Also-have you tried fasting? Or crystals? Just saying.
Alanah Marie Cam
November 4 2025This is exactly the kind of education that saves lives-and it’s not just for doctors or pharmacists. It’s for every person who takes any kind of medication, even aspirin.
If you’re reading this and you’re on more than three meds, please, take five minutes today and write down everything you take. Include the herbal tea you drink every night. Include the magnesium you started for ‘sleep.’
Bring it to your pharmacist. Ask: ‘Could any of these be fighting each other?’
You don’t need to be an expert. You just need to care enough to ask.
And if you’re a caregiver? Do this for your loved ones. They might not remember. But you can.
Small steps. Big impact.
Patrick Hogan
November 5 2025So you’re telling me that if I take my Adderall with my coffee, I’m not just ‘extra alert’-I’m playing Russian roulette with my heart rate? And I thought I was just being productive.
Also, my mom takes 17 pills. And she calls them ‘her little friends.’
God help us all.
Also, I just Googled ‘can I take melatonin with warfarin’ and the first result was a Reddit thread from 2016. That’s our healthcare system in a nutshell.
prajesh kumar
November 5 2025Bro this is so important I wish every family in India had this printed and taped on their fridge
My uncle took digoxin and got sick because he started eating too many oranges-potassium messed with his levels and no one told him
Doctors are busy but you can be the one who asks
Write it down
Ask your pharmacist
Don’t assume it’s fine
It’s not just about you
It’s about your mom your dad your grandma who thinks ‘natural’ means safe
We can do better
And we will
One pill at a time
Arpit Sinojia
November 7 2025I used to think drug interactions were just for old people in hospitals. Then my cousin took cipro and Tums before bed and didn’t get better for a week. Turned out the antacid blocked 90% of the antibiotic. He didn’t even know it was a thing. Just thought the pill was ‘weak.’
Now I ask everyone: ‘What else you taking?’
Even if it’s just ginger tea.
Turns out, the body’s got a lot of secrets.