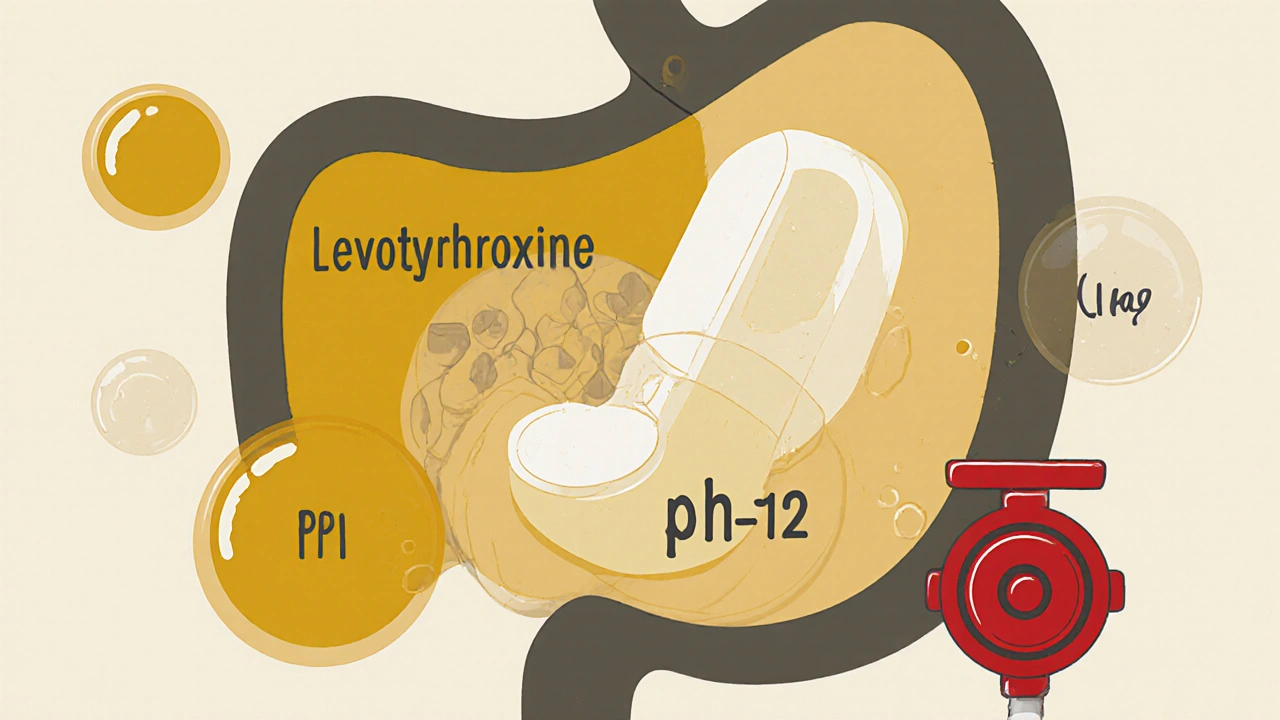
Levothyroxine and Proton Pump Inhibitors: How They Interfere with Absorption
Levothyroxine-PPI Dose Adjustment Calculator
How PPIs Affect Your Levothyroxine
Proton pump inhibitors (PPIs) reduce stomach acid, which can decrease levothyroxine absorption. Studies show 15-20% of patients need dose increases when taking both medications.
Suggested Adjustment
Based on clinical studies showing 15-20% increase needed when taking PPIs. Average adjustment: 12.5-25 mcg.
Important Medical Note
Never adjust your thyroid medication without consulting your doctor. This calculator provides estimated guidance based on published studies.
When you’re taking levothyroxine for hypothyroidism, even small changes in how your body absorbs the drug can throw your whole system off. That’s why so many patients end up feeling tired, gaining weight, or struggling with brain fog - not because their thyroid is worsening, but because something else is blocking their medication from working. One of the most common but often overlooked culprits? Proton pump inhibitors, or PPIs, the drugs millions of people take daily for heartburn and acid reflux.
Why Levothyroxine Needs Acid
Levothyroxine isn’t like most pills. It doesn’t just dissolve and get absorbed anywhere in your gut. It needs an acidic environment - specifically, a stomach pH between 1 and 2 - to dissolve properly and enter your bloodstream. Without that acidity, the tablet stays mostly intact, passing through your system without doing its job. That’s why doctors tell you to take it on an empty stomach, at least 30 to 60 minutes before breakfast. But if you’re also taking a PPI like omeprazole (Prilosec), esomeprazole (Nexium), or pantoprazole (Protonix), you’re essentially turning your stomach into a neutral zone.
PPIs work by shutting down the acid pumps in your stomach lining. They’re powerful. One dose can keep your stomach pH at 4 to 6 for up to 24 hours. That’s not just mildly less acidic - it’s a complete overhaul of the environment levothyroxine needs. Multiple studies, including a 2021 systematic review in the Journal of General Internal Medicine, show that when these two drugs are taken together, thyroid-stimulating hormone (TSH) levels rise. And when TSH goes up, it means your thyroid isn’t getting enough hormone signal - because your body isn’t absorbing enough levothyroxine.
The Numbers Don’t Lie
It’s not rare. About 18% of people taking levothyroxine are also on a PPI. That’s nearly 2.7 million Americans alone. And according to data from the Mayo Clinic, about 15 to 20% of those patients need a higher dose of levothyroxine to stay in range. The average increase? Between 12.5 and 25 micrograms per day. That’s not a tiny tweak - it’s a full dose adjustment, often missed because doctors don’t connect the dots.
A 2023 study published in PubMed followed patients on 40mg of pantoprazole daily for just six weeks. Even though they were taking levothyroxine in the morning and pantoprazole at night, TSH levels still jumped. The researchers tried separating the doses by hours - morning levothyroxine, evening PPI - and it made no difference. Why? Because PPIs don’t just turn off acid for a few hours. Their effect lasts for days. One dose can suppress acid production for up to 72 hours. So timing doesn’t fix it. The suppression is too long-lasting.
What Happens When Levothyroxine Doesn’t Work
If your body isn’t absorbing enough levothyroxine, your thyroid hormone levels drop. That’s when symptoms creep in: fatigue, weight gain, cold intolerance, depression, brain fog. Many patients assume they’re just getting older, or stressed, or eating too much. But the real issue? Their medication isn’t working.
Online forums like Reddit’s r/Hashimotos have thousands of posts from people who discovered this interaction the hard way. One analysis of 147 posts from October 2023 found that 68% of long-term PPI users reported needing higher levothyroxine doses. Seventy-two percent said they felt more tired. Fifty-eight percent noticed unexplained weight gain. These aren’t side effects of the disease - they’re side effects of a hidden drug interaction.

What You Can Do
There are real solutions - but they require action, not just waiting for your next TSH test.
- Test your TSH before starting a PPI. If you’re about to begin acid reflux treatment, get a baseline TSH level. That way, if it rises later, you know why.
- Retest after 6 to 8 weeks. The American Association of Clinical Endocrinologists recommends this. Don’t wait six months. If your TSH is up, your dose likely needs adjusting.
- Consider switching your acid reducer. H2 blockers like famotidine (Pepcid) don’t suppress acid as strongly or as long as PPIs. A 2018 study in Pharmacotherapy showed no significant TSH changes when famotidine was taken with levothyroxine. It’s not as strong as a PPI, but for mild reflux, it might be enough.
- Try liquid levothyroxine. Tirosint-SOL is a liquid formulation that doesn’t need stomach acid to be absorbed. A 2019 study in the Journal of Clinical Endocrinology & Metabolism confirmed it works just fine with PPIs. The catch? It costs $350 a month, compared to $15-$25 for generic tablets. But for people who’ve struggled with dose adjustments for years, it can be life-changing.
What Doesn’t Work
Many people think, “I’ll just take my levothyroxine four hours before my PPI.” That’s what some websites still recommend. But the science says otherwise. The 2021 NIH review and the 2023 pantoprazole study both found that spacing doses doesn’t help. Why? Because PPIs don’t work like antacids. They don’t just neutralize acid for a few hours. They shut down your stomach’s ability to make acid for days. So even if you take levothyroxine in the morning and PPI at night, your stomach is still too neutral by morning.
Short-term PPI use - less than four weeks - is usually fine. But if you’ve been on it for three months or longer, your body has adapted to low acid. And that’s when levothyroxine absorption drops.

The Future Is Changing
Drug manufacturers are paying attention. The FDA released draft guidance in 2023 specifically about labeling thyroid medications with PPI interaction warnings. New formulations are in the works, including enteric-coated levothyroxine pills designed to dissolve in the small intestine instead of the stomach. Phase 3 trials are ongoing.
Meanwhile, the patent for Tirosint-SOL expires in 2025. That could mean cheaper generic versions of liquid levothyroxine hitting the market - potentially making this solution accessible to millions who can’t afford the current price.
What to Do Right Now
If you’re taking both levothyroxine and a PPI:
- Check your last TSH result. Is it above your target range?
- Ask your doctor if your PPI is necessary. Could you try H2 blockers instead?
- If you need the PPI and your TSH is high, ask about switching to Tirosint-SOL.
- Don’t change your dose on your own. Adjustments need to be guided by blood tests.
This isn’t about avoiding PPIs. For many, they’re essential. But it’s about recognizing that your thyroid medication doesn’t work the same way when your stomach isn’t acidic. And that’s not a flaw in you - it’s a flaw in how we treat these two conditions separately, instead of together.
Thyroid health is delicate. Levothyroxine is a precise tool. When you add something that changes how it’s absorbed, you change the outcome. Pay attention. Test. Ask questions. Your energy, your weight, your mood - they’re all connected to how well that little pill gets into your blood.
Can I take levothyroxine and a PPI at the same time?
No, taking them together reduces levothyroxine absorption. Even spacing them by several hours doesn’t help because PPIs suppress stomach acid for up to 72 hours. The best approach is to either switch to a different acid reducer like famotidine or use liquid levothyroxine, which doesn’t require stomach acid.
Why does my TSH keep going up even though I take my thyroid medication?
If you’re also taking a proton pump inhibitor (PPI), it’s likely interfering with how your body absorbs levothyroxine. PPIs reduce stomach acid, which is needed for the tablet to dissolve properly. This causes your thyroid hormone levels to drop, making your TSH rise. A simple blood test and a review of your medications can confirm this.
Is famotidine (Pepcid) safer than PPIs with levothyroxine?
Yes. Studies show that famotidine doesn’t significantly affect levothyroxine absorption. While it’s not as strong as PPIs at reducing acid, it’s often sufficient for mild to moderate heartburn and doesn’t interfere with thyroid medication like PPIs do.
Should I stop taking my PPI if I’m on levothyroxine?
Don’t stop your PPI without talking to your doctor. If you have severe acid reflux or GERD, stopping it could cause serious complications. Instead, work with your provider to find a solution - like switching to famotidine, using liquid levothyroxine, or adjusting your levothyroxine dose based on TSH levels.
How often should I get my TSH checked if I take both medications?
Get your TSH tested before starting a PPI, then again 6 to 8 weeks after starting. If your dose needs adjustment, retest every 6 to 8 weeks until your levels stabilize. Once stable, routine testing every 6 to 12 months is usually enough - unless your medications change.
Is liquid levothyroxine worth the cost?
If you’ve struggled with inconsistent thyroid levels despite dose adjustments, and you’re on long-term PPI therapy, yes. Tirosint-SOL costs about $350 a month, compared to $15-$25 for generic tablets. But for many, it eliminates the need for frequent dose changes, reduces symptoms like fatigue and weight gain, and improves quality of life. It’s an investment in stability.



15 Comments
Peter Aultman
November 15 2025Just found out my TSH was creeping up and I was on omeprazole for years. Never connected the dots. Switched to famotidine and my energy came back in two weeks. No joke. This post saved me from another year of feeling like a zombie.
Dilip Patel
November 15 2025India me bhi yehi problem hai log levothyroxine lete hai aur PPI bhi lete hai aur phir doctor ko blame karte hai. Kya pata kisi ko science ki koi baat hai?
gent wood
November 16 2025This is the kind of post that should be mandatory reading for every endocrinologist and GP. I’ve seen so many patients misdiagnosed as ‘just stressed’ or ‘depressed’ when the real issue is a silent drug interaction. The fact that PPIs suppress acid for 72 hours makes spacing doses pointless. It’s not about timing-it’s about chemistry. And yet, most patients aren’t warned until their TSH is through the roof.
I had a patient last month who’d been on 125mcg of levothyroxine for years. Her TSH was 8.5. We cut the PPI, switched to Pepcid, and within six weeks she was at 1.8. She cried in the office. Not from sadness-from relief. She hadn’t felt this clear-headed in five years.
It’s not just about dosage. It’s about awareness. We treat thyroid and GI as separate systems, but they’re not. The stomach isn’t just a pipe-it’s a gatekeeper. And when you lock that gate with a PPI, you’re starving your thyroid of its fuel.
And don’t get me started on how long it takes for doctors to even consider this. Patients come in with fatigue, weight gain, brain fog… and we blame their lifestyle, their sleep, their diet. Meanwhile, the simplest fix is hiding in plain sight: their medication list.
The FDA draft guidance is a start. But it needs to be louder. Pharmacies should flag this interaction at checkout. Electronic health records should scream it. We need alerts, not just studies.
And yes, Tirosint-SOL is expensive. But if you’re spending hundreds on labs, specialist visits, and failed dose adjustments, it’s cheaper in the long run. Quality of life isn’t a luxury-it’s a baseline.
Stop treating symptoms. Start treating systems.
Barry Sanders
November 18 2025Typical American medical incompetence. You take a pill for heartburn, then another for the side effects of the first pill, then another for the side effects of that. It’s a pyramid scheme of pharmaceutical dependency.
Sean Hwang
November 19 2025My mom was on Nexium for 10 years and her thyroid dose kept going up. We finally switched her to Pepcid and boom-her levels stabilized. She’s got more energy now than she did in her 50s. Don’t overcomplicate it. If you’re on a PPI and your thyroid meds aren’t working, talk to your doc about H2 blockers.
Jane Johnson
November 21 2025It is imperative to note that the physiological interplay between gastric acid suppression and levothyroxine bioavailability is not merely a pharmacokinetic curiosity-it is a clinically significant phenomenon requiring systematic intervention.
Brittany C
November 21 2025As a clinical pharmacist, I’ve seen this pattern repeatedly. PPIs alter gastric pH, which affects the solubility of levothyroxine’s crystalline structure. The consequence is reduced Cmax and delayed Tmax-meaning less hormone enters circulation. Liquid formulations bypass this entirely. Tirosint-SOL isn’t a ‘premium option’-it’s a physiologically appropriate alternative for patients on chronic acid suppression.
kshitij pandey
November 22 2025Bro, this is so important. In India, people just buy PPIs over the counter and take them forever. No one checks TSH. My cousin was gaining weight, sleeping all day, and the doctor said ‘eat less’. I showed him this post. He switched to Pepcid and now he’s running 5Ks. Thank you for writing this.
Sean Evans
November 23 2025Of course this happens. Big Pharma doesn’t want you to know you can fix this with a $10 H2 blocker. They make billions selling you PPIs AND higher-dose levothyroxine. 🤡
Peter Aultman
November 23 2025Yeah, I tried spacing them out for months. Morning levo, night PPI. Still had the same TSH. I thought I was doing everything right. Turns out, I was just wasting time.
Brian Bell
November 24 2025My doctor didn’t even know about this. I had to bring him the study. Now he’s asking every thyroid patient if they’re on PPIs. Small change, big impact.
Anjan Patel
November 26 2025People are so lazy they’d rather take 3 pills a day than fix their diet. Eat less spicy food. Stop drinking coffee on an empty stomach. Stop eating late. Then you won’t need PPIs. But nooo, let’s just pump your stomach full of chemicals.
Scarlett Walker
November 26 2025My TSH was 11. I was convinced I had Hashimoto’s getting worse. Turned out I’d been on pantoprazole for 2 years. Switched to Pepcid. Two months later, TSH was 2.3. I didn’t need more meds-I just needed to stop one.
Hrudananda Rath
November 28 2025It is an epistemological failure of contemporary medical education that the pharmacodynamic interaction between proton pump inhibitors and levothyroxine remains underappreciated in primary care settings. The absence of standardized screening protocols constitutes a systemic dereliction of duty.
Chris Ashley
November 29 2025I took my levothyroxine at 6am and my PPI at 8pm. Thought I was being smart. Turns out my stomach was still neutral at 6am. So I switched to liquid. Best decision ever. Now I’m not tired all the time. No more brain fog. No more weight gain. Just… normal.