Preterm Infants and Medication Side Effects: What NICU Teams Need to Know
NICU Medication Risk Checker
Understanding NICU Medications
Most NICU medications weren't tested on preterm infants. 60% have no FDA approval for infants under 1 year. This tool helps you understand evidence and risks so you can advocate for your baby.
Medication Information
Preterm infants are not small adults - and their medications shouldn’t be treated like they are
Every year, over 1 in 10 babies in the U.S. are born too soon. These preterm infants, especially those born before 28 weeks, face a battlefield of medical interventions just to survive. One of the most dangerous? Medications. What seems like a routine dose of pain relief, antibiotics, or acid blockers can have lasting consequences - not because the drugs are bad, but because preterm infants’ bodies handle them in ways doctors still don’t fully understand.
Here’s the hard truth: 100% of extremely preterm infants in the NICU get at least one medication during their stay. Many get multiple. Opioids. Benzodiazepines. Antibiotics. Caffeine. Proton pump inhibitors. But here’s what most parents - and even some clinicians - don’t realize: most of these drugs were never tested on babies this small. Over 60% of medications used in NICUs have no FDA approval for infants under one year. That means doctors are guessing. And sometimes, those guesses hurt.
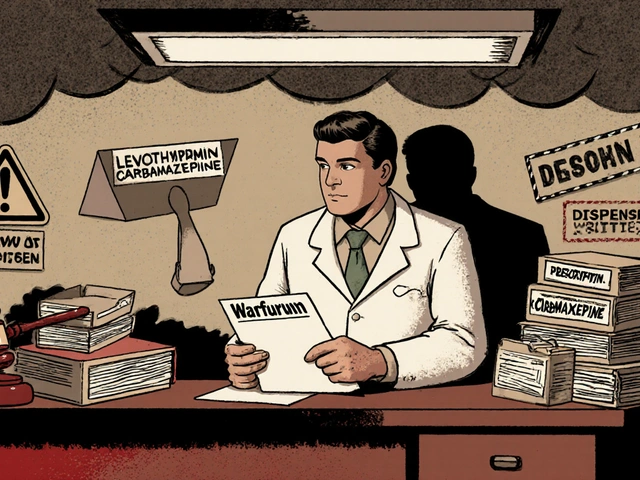
Why dosing preterm infants is like navigating a minefield
It’s not just about weight. A 1,000-gram baby born at 24 weeks doesn’t metabolize drugs like a 3,000-gram baby born at 36 weeks. Their liver is still learning how to break things down. Their kidneys can’t filter waste the way older babies can. Their blood-brain barrier is leaky. Their gut is a fragile ecosystem.
Take caffeine, the go-to drug for apnea of prematurity. It’s effective - but 18.7% of infants on standard doses develop fast heart rates. About 7% can’t tolerate feeding because of it. That’s not rare. That’s common enough that every NICU nurse needs to watch for it. But what if the baby also has a patent ductus arteriosus (PDA)? That single condition can increase the volume of distribution for some drugs by 80%. A dose that’s perfect for one preterm infant could be toxic for another - just because of a heart defect.
And then there’s the clock. Cytochrome P450 enzymes, the liver’s main drug-processing system, are only 30% mature at 32 weeks. They don’t hit adult levels until the baby is 12 months old. That means drugs like morphine or fentanyl - commonly used for pain - stick around longer. The risk of respiratory depression? Higher. The window for safe dosing? Narrower.
The hidden cost of antibiotics: A gut that never recovers
Antibiotics are the most prescribed drugs in the NICU. But they’re not harmless. A 2021 study from Washington University showed that preterm infants exposed to antibiotics had gut microbiomes packed with 47% more harmful bacteria and 32% fewer good ones. These changes didn’t go away after discharge. They lasted 18 months.
Why does that matter? Because the gut microbiome shapes immunity, brain development, and even metabolism. Babies who get broad-spectrum antibiotics early are more likely to develop allergies, asthma, and recurrent infections later. One parent on Reddit shared: “My son got 28 days of antibiotics for suspected sepsis - never confirmed. At age 2, he’s had five ear infections and two rounds of antibiotics.” That’s not an outlier. It’s the pattern.
And here’s the kicker: many of these antibiotics are given for “possible sepsis” - a diagnosis based on vague signs like temperature swings or low blood pressure. But in preterm infants, those signs are often just normal stress responses. Yet, 70% of these babies still get antibiotics. The risk? A gut microbiome that’s permanently altered. The reward? Sometimes, nothing at all.
Anti-reflux drugs: Prescribed often. Proven useless. Dangerous always
One of the most shocking practices in the NICU? Giving proton pump inhibitors (PPIs) like omeprazole to preterm infants for reflux. It’s done in 41% of NICU graduates. Why? Because parents and nurses see spit-up and assume it’s pain. But here’s what the science says: there’s no evidence these drugs help.
The 2022 Cochrane review - the gold standard in medical evidence - found no benefit from acid-suppressing meds in preterm infants. Yet, the risks are real. These drugs increase the chance of necrotizing enterocolitis (NEC) by 67%, late-onset sepsis by 89%, and bone fractures by 130%. Why? Because stomach acid isn’t just for digestion - it’s a barrier. Lowering it lets bad bacteria grow. And in a preterm gut, that’s a recipe for disaster.
Despite this, many NICUs still start PPIs routinely. The AAP updated its guidelines in January 2024 to say: stop. But change moves slowly. And while it does, babies are being put at unnecessary risk.
Neurotoxic drugs: Pain relief that might harm the brain
Preterm infants feel pain - and they feel it deeply. But for decades, doctors avoided giving them pain meds, fearing addiction or breathing problems. That changed in the 1990s. Now, 42.7% get opioids. 28.3% get benzodiazepines. Both are powerful. Both are neurotoxic.
Studies show repeated exposure to these drugs during critical brain development windows can alter neural connections. The result? Higher risk of attention deficits, learning delays, and behavioral issues later in life. The AAP now says: don’t use them routinely. Use them only when pain is confirmed - and then, use the lowest dose for the shortest time.
That’s easier said than done. Pain assessment in nonverbal infants is hard. But tools like the CRIES scale and the CRIES-2 are now standard in top NICUs. Nurses are trained to look for facial grimacing, limb withdrawal, and changes in heart rate - not just crying. And when pain is confirmed, non-drug options come first: swaddling, skin-to-skin contact, sucrose drops. Drugs are the last resort.

What’s changing - and what’s working
Change is happening, but it’s slow. Some NICUs are using pharmacokinetic modeling software like DoseMeRx. It takes into account gestational age, weight, kidney function, and even the presence of PDA to calculate precise doses. In units using it, dosing errors dropped by nearly 60% in babies under 28 weeks.
Standardized weaning protocols for opioids and sedatives are another win. One study found that when NICUs used structured plans to taper these drugs, infants spent 14 fewer days on them - without more pain or distress. That’s a win for the brain and the body.
And then there’s the future. The FDA has fast-tracked NeoFen, the first fentanyl formulation designed specifically for preterm infants. It’s expected to be approved in mid-2025. Researchers are testing “microbiome-sparing” antibiotics that target harmful bugs without wiping out the good ones. The Neonatal Precision Medicine Initiative aims to create individualized dosing models for 25 high-risk drugs by 2026.
What parents should ask
If your baby is in the NICU, you have the right to know what’s being given - and why. Don’t be afraid to ask:
- Is this medication FDA-approved for preterm infants?
- Is there evidence this helps - or is it being used because it’s “what we’ve always done”?
- What are the risks? Can we try non-drug options first?
- How long will my baby be on this? Is there a plan to stop it?
Parents are the most powerful advocates. When they ask these questions, care improves. Studies show NICUs with strong parent engagement have lower rates of medication errors and shorter hospital stays.
The bottom line: Less is often more
Preterm infants don’t need more drugs. They need smarter ones. They need fewer, better-timed, and better-monitored doses. They need clinicians who understand that their bodies aren’t broken adults - they’re developing systems, vulnerable and unique.
The good news? We’re learning. The bad news? Too many babies are still being exposed to drugs with known risks and unproven benefits. The goal isn’t to avoid all medications. It’s to avoid the ones that do more harm than good.
Every dose matters. Every decision counts. And for preterm infants, the right choice today might mean a healthier brain - and a better life - tomorrow.
Are all medications given in the NICU unsafe for preterm infants?
No. Many medications, like caffeine for apnea or surfactant for lung development, are life-saving and well-studied. The problem isn’t medication itself - it’s the overuse and inappropriate use of drugs that haven’t been tested for this population. Opioids, benzodiazepines, antibiotics, and acid blockers are often given routinely, even when evidence doesn’t support their use - and when safer alternatives exist.
Why are so many NICU drugs given off-label?
Because pharmaceutical companies rarely test drugs on preterm infants. Clinical trials are expensive, ethically complex, and slow. As a result, 92% of respiratory medications and over 60% of all NICU drugs are used without FDA approval for this age group. Doctors rely on adult data, animal studies, or small, outdated studies - and then adjust doses based on weight or gestational age. It’s a guess - and sometimes, it’s dangerous.
Can antibiotics cause long-term health problems in preterm babies?
Yes. Studies show preterm infants exposed to antibiotics develop gut microbiomes with fewer beneficial bacteria and more antibiotic-resistant pathogens. These changes persist for at least 18 months and are linked to higher rates of asthma, allergies, eczema, and recurrent infections later in childhood. The more antibiotics given - especially broad-spectrum ones - the greater the risk.
Is it safe to give acid-reducing drugs like omeprazole to preterm infants?
No. Despite being prescribed to 41% of NICU graduates, proton pump inhibitors offer no proven benefit for reflux in preterm infants. The AAP updated its guidelines in 2024 to strongly advise against their use. These drugs increase the risk of necrotizing enterocolitis (NEC), sepsis, and bone fractures - all serious, potentially life-threatening complications.
What can parents do to reduce medication risks in the NICU?
Ask questions. Request a clear reason for every medication. Ask if non-drug options like skin-to-skin contact or swaddling have been tried. Inquire about the duration of treatment and the plan to wean. Keep a log of medications and side effects. Advocate for evidence-based care - and don’t accept “it’s standard practice” as an answer. Your involvement improves outcomes.



9 Comments
Patrick Merk
November 18 2025Man, this post hit different. I work in neonatal transport and see this every shift - meds thrown at preterms like they’re just tiny adults with IVs. That PPI stat? 41%?! No wonder so many of these babies end up with NEC. We’ve cut ours by 70% just by asking ‘Do we really need this?’ before pressing go. Small wins, but they matter.
Liam Dunne
November 19 2025Been in NICU nursing for 12 years. Used to think caffeine was harmless. Then I saw a 24-weeker go into tachy after a standard dose - heart rate hit 240. Turned out her PDA was undiagnosed. Dose was fine for most, but for her? Toxic. Now we check echo reports before every med pass. Knowledge is power, but context is everything.
Jennifer Howard
November 20 2025While I appreciate the sentiment, it is imperative to note that the absence of FDA approval does not equate to medical negligence. The pharmaceutical industry is not obligated to conduct pediatric trials unless incentivized by regulatory provisions such as the Best Pharmaceuticals for Children Act. Furthermore, the cited studies, while compelling, are observational and cannot establish causation. To suggest that clinicians are 'guessing' is both misleading and ethically irresponsible.
Abdul Mubeen
November 21 2025Let’s be real - this whole ‘preterm infant medicine’ thing is just Big Pharma’s way to keep hospitals hooked on profit. They don’t test on babies because they don’t want to be sued. Meanwhile, the AAP changes guidelines every other Tuesday while nurses keep dosing like it’s 2005. Who profits? The drug reps. Who suffers? The babies. Wake up.
mike tallent
November 22 2025THIS. 🙌 I’m a NICU dad of a 26-weeker. We asked about every med - even the ‘routine’ ones. They stopped the PPI after 3 days. Started skin-to-skin 24/7. Used sucrose drops before heel sticks. He’s 2 now - no asthma, no ear infections, no meds. Just a happy kid who loves trains. Ask. Push. Advocate. It works. 💪👶
Joyce Genon
November 24 2025Let’s not romanticize the ‘less is more’ narrative. You’re ignoring the fact that many of these infants would die without antibiotics or opioids. You cite Cochrane reviews like they’re gospel, but you ignore the 30% of preterms who die from untreated sepsis because someone waited for ‘evidence.’ The data you cherry-pick ignores the bigger picture: we’re doing our best with broken tools. Blaming nurses for giving PPIs is like blaming firefighters for using water when the building’s on fire. The system’s broken - not the clinicians.
John Wayne
November 25 2025Interesting. The article reads like a policy brief masquerading as medical insight. One wonders if the author has ever actually held a preterm infant. The emphasis on microbiome disruption is trendy, but the clinical impact remains speculative. And yet, here we are - rewriting protocols based on mouse studies and Reddit anecdotes. Progress, it seems, is now defined by virtue signaling.
Julie Roe
November 25 2025For all the parents reading this - you’re not being too pushy. You’re being brave. I’ve sat in NICU rooms where moms cried because they didn’t know if the meds were helping or hurting. You deserve to know. Ask for the drug name, the indication, the alternatives, and the plan to wean. Write it down. Bring a partner. If they get defensive? That’s a red flag. The best NICUs don’t get mad when you ask - they get grateful. You’re not a hassle. You’re part of the team. And your baby? They’re lucky to have you. 💕
jalyssa chea
November 25 2025I work in pharmacy and let me tell you the truth nobody wants to hear - most of these meds are given because the docs dont want to admit they dont know what to do. I've seen 23 weekers on 5 antibiotics and a PPI because the nurse said 'she looked tired'. No labs no culture no nothing. Just fear. And yeah the gut gets wrecked. But nobody wants to say 'we dont know' so they give the drug and hope. Its not science its damage control