Psychiatric Medication Combinations: Generic Alternatives and What You Need to Know
When a single psychiatric medication doesn’t cut it, doctors often turn to psychiatric medication combinations. This isn’t experimental-it’s standard practice for people with treatment-resistant depression, bipolar disorder, or severe anxiety that won’t budge with one drug alone. But here’s the catch: swapping brand-name drugs for generics in these combinations can quietly unravel a carefully balanced treatment plan.
Why Combine Medications at All?
Most people start with one antidepressant-say, sertraline or escitalopram. But for about one in three, that’s not enough. The STAR*D trial, a massive study by the National Institute of Mental Health, showed that after trying one antidepressant, only about 30% of patients reached full remission. That’s why doctors add a second drug. Common combinations include:- SSRI or SNRI + low-dose aripiprazole (Abilify) for depression that won’t lift
- Fluoxetine + olanzapine (Symbyax), a fixed-dose combo approved for treatment-resistant depression since 2003
- SSRI + buspirone to tackle lingering anxiety without the risk of benzodiazepine dependence
- Bupropion + SSRI to fix sexual side effects caused by the antidepressant alone
The Generic Substitution Problem
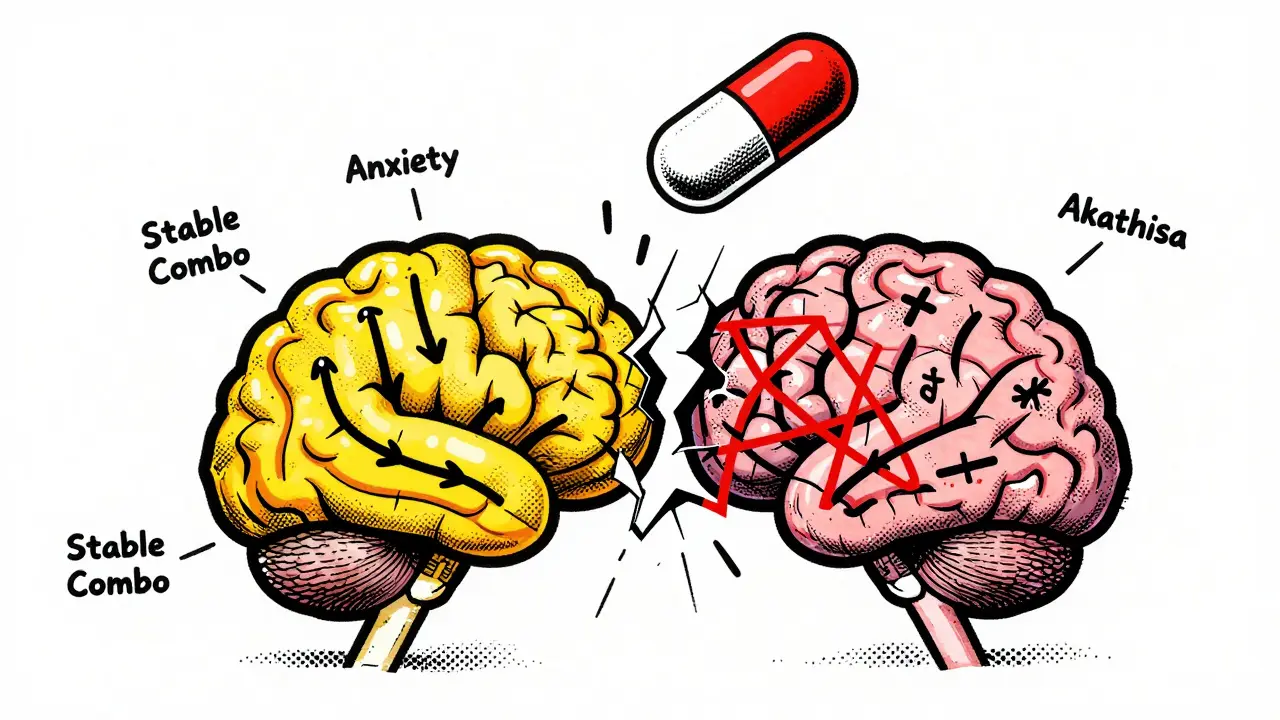
The FDA says a generic drug must be 80-125% as bioavailable as the brand-name version. Sounds fine, right? But in psychiatry, that 45% window is dangerous. Take lithium. It’s used for bipolar disorder. The therapeutic range? 0.6 to 1.2 mmol/L. Go below 0.6, and you risk relapse into depression. Go above 1.2, and you risk toxicity-tremors, confusion, even kidney damage. A 2018 case series from the University of British Columbia tracked three patients who switched from brand-name Eskalith to a generic lithium carbonate. Their blood levels dropped from 0.85 to 0.55 mmol/L-within days. All three relapsed into mania. It’s not just lithium. Generic bupropion XL (Wellbutrin XL) has been flagged by the FDA since 2012. Over 137 adverse event reports describe breakthrough anxiety, mood swings, and depression after switching to certain generic versions. Why? The extended-release beads don’t dissolve the same way. One manufacturer’s beads might release too fast. Another’s too slow. The result? Unpredictable drug levels. Venlafaxine ER (Effexor XR) is another trouble spot. It works by balancing serotonin and norepinephrine at a 2:1 ratio. Different generic makers use different bead technologies. Some alter that ratio. If you’re on venlafaxine plus another medication-say, a mood stabilizer-this tiny shift can destabilize the whole system.What the Data Shows
A 2019 study in the Journal of Clinical Psychiatry looked at nearly 28,500 patients on SSRIs. Those switched to generics had a 22.3% higher chance of treatment failure. That means more doctor visits, more relapses, more hospitalizations. Another analysis in JAMA Internal Medicine found that 7.2% of patients on psychotropic meds had clinical deterioration after switching to generics. The highest rates? Antidepressants (9.1%) and mood stabilizers (8.3%). Real people are reporting this too. On Reddit’s r/depression, a top thread from May 2023 titled “Generic switch ruined my carefully balanced med cocktail” had over 1,200 upvotes and nearly 300 comments. People wrote about:- Switching from brand Lamictal to Apotex generic-then Zoloft stopped working
- Switching Abilify generics-obsessive thoughts returned with full force
- Generic fluoxetine causing akathisia (restlessness so severe it led to hospitalization)

Who’s at Highest Risk?
Not everyone has problems. But some people are far more vulnerable:- Narrow therapeutic index drugs: Lithium, carbamazepine, valproate, clozapine. Even tiny changes in blood levels matter.
- Combination therapy: Two or more psych meds. One generic switch can throw off the balance of the whole system.
- Previous bad reactions: If you’ve had a flare-up after switching before, you’re at higher risk again.
- Older adults or those with liver/kidney issues: Their bodies process drugs slower, making bioequivalence gaps more dangerous.
How to Protect Yourself
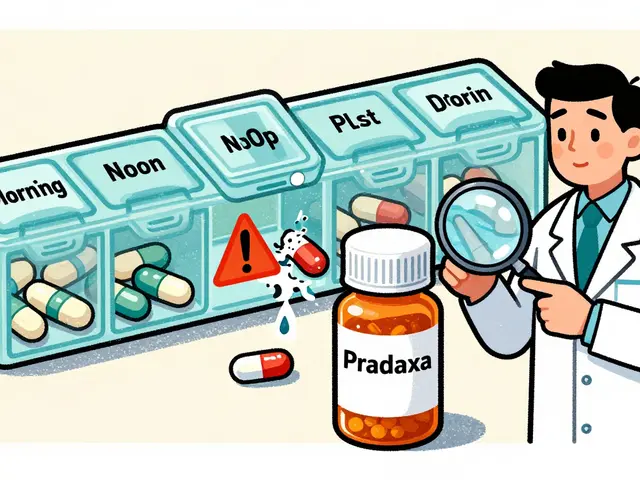
If you’re on a psychiatric combo, here’s what you need to do:- Know your meds. Write down the exact brand and generic name of each drug, plus the manufacturer. If you’re on Abilify, is it from AbbVie? Or a generic from Mylan or Aurobindo?
- Ask before you switch. Tell your pharmacist and prescriber: “I’m on a combination. I need to stay on the same formulation.”
- Get baseline scores. Before any switch, ask your doctor to use a standardized scale like the MADRS (Montgomery-Åsberg Depression Rating Scale). This gives you a real number to compare against later.
- Monitor closely after switching. Schedule a follow-up within 7-10 days. Watch for subtle changes: sleep worsening, irritability, brain fog, panic spikes.
- Request therapeutic drug monitoring. For lithium, valproate, or clozapine, ask for a blood test 7-14 days after a generic switch. Even if you feel fine, levels might be off.
What’s Changing?
The system is starting to wake up. In January 2023, California passed AB 1477, requiring pharmacists to notify prescribers when substituting psych meds in patients on multiple drugs. Michigan saw a 22% drop in ER visits after a similar law. The FDA is now considering tighter bioequivalence rules-90-111% instead of 80-125%-for extended-release psych drugs used in combos. The Department of Veterans Affairs now requires patients stabilized on combo therapy to stay on the same generic manufacturer for at least 12 months. Since the rule started, psychiatric hospitalizations dropped 18.7%. Authorized generics-brand-name drugs sold under a generic label-are becoming more common. Symbyax now has an authorized generic. It’s the same formula, just cheaper. Ask your doctor if one’s available.The Cost vs. Safety Debate
Generic drugs saved the U.S. healthcare system over $300 billion in 2022. That’s huge. But in psychiatry, cutting costs too aggressively can cost lives. A Johns Hopkins economist argues generics are generally safe and necessary. But even he admits: “High-risk combinations-lithium, clozapine-need extra caution.” Meanwhile, Medicaid patients are far more likely to get generics than those with private insurance. That’s not just a cost issue-it’s an equity issue. Lower-income patients are bearing the brunt of substitution risks.The Bottom Line
Psychiatric medication combinations are powerful tools. But they’re fragile. A small change in drug absorption can tip someone from stable to suicidal, from calm to manic. Generic substitutions aren’t always bad-but they’re not risk-free, especially in combos. If you’re on more than one psychiatric drug, don’t assume generics are interchangeable. Ask questions. Track your symptoms. Demand monitoring. Your brain chemistry isn’t a commodity to be swapped for a lower price tag.Stability matters more than savings. And sometimes, the most expensive thing isn’t the brand-name pill-it’s the hospital bed you end up in after a switch gone wrong.




13 Comments
Carolyn Whitehead
February 1 2026Been on a combo for 8 years and never switched generics-best decision I ever made. My mood’s steady, my sleep’s solid, and I don’t have to wonder if today’s weird anxiety spike is me or my pill bottle.
Just say no to the pharmacy’s cost-cutting magic trick.
Rob Webber
February 2 2026So let me get this straight-we’re letting big pharma and insurance companies gamble with people’s sanity because it saves a few bucks per script? This isn’t healthcare, it’s human experimentation with a side of greed.
Someone needs to sue the FDA.
calanha nevin
February 3 2026If you’re on multiple psych meds, never accept a generic switch without a blood test and a follow-up in 7 days.
Write down your manufacturer. Ask for the lot number. Track your symptoms on a simple scale.
You are not a data point. You are a person with a brain that doesn’t tolerate guesswork.
owori patrick
February 4 2026This is why I always ask my pharmacist to show me the label before they hand me the bottle.
Some generics are fine, others feel like different drugs entirely.
Knowledge is power when your brain is on the line.
Lisa McCluskey
February 4 2026I switched to a generic bupropion last year and spent three weeks feeling like I was underwater.
Went back to brand-suddenly I could breathe again.
Don’t wait for a crisis to realize your meds aren’t interchangeable.
Trust your body more than the system.
Claire Wiltshire
February 4 2026The FDA’s 80-125% bioequivalence window is a statistical loophole that ignores neurobiology.
Psychiatric medications aren’t aspirin-they modulate entire neural networks.
When the system treats them like commodities, people suffer.
Advocate for yourself. Document everything. Demand therapeutic drug monitoring.
Stability is not a luxury. It’s a medical necessity.
April Allen
February 6 2026The real issue isn’t generics-it’s the lack of standardized bioequivalence testing for extended-release formulations in psychiatric use.
Pharmacokinetics aren’t one-size-fits-all, yet the regulatory framework treats them like that.
Studies show inter-manufacturer variability in bead dissolution can cause 30-40% fluctuations in peak concentration.
That’s not equivalence. That’s roulette with your neurochemistry.
We need manufacturer-specific prescribing, not just generic substitution.
And yes, this disproportionately harms low-income patients who have no choice.
It’s not just a pharmacological problem. It’s an ethical one.
Jodi Olson
February 7 2026It’s fascinating how we accept bioequivalence in a system where the margin of error could trigger mania or suicidal ideation.
Psychiatry operates on the edge of chaos.
Yet the regulatory architecture is built for mass-market convenience, not individual neurodiversity.
We treat the brain like a machine that can be calibrated with interchangeable parts.
It’s not.
It’s a living, dynamic ecosystem.
And we’re treating it like a car engine you swap out for a cheaper model.
Eventually, the whole system fails.
And the cost isn’t measured in dollars.
It’s measured in sleepless nights, ER visits, and lost years.
We need a paradigm shift, not just policy tweaks.
Bobbi Van Riet
February 8 2026I had a patient who switched from brand Abilify to a generic and went from stable to cycling mania-depression every two weeks.
She didn’t tell anyone because she was afraid they’d think she was ‘noncompliant’.
When she finally spoke up, her doctor was shocked.
Turns out, the generic had different bead coatings that altered release timing.
She got her brand back and within 10 days, her mood stabilized.
Don’t let fear silence you.
If something feels off after a switch, speak up-even if you think you’re overreacting.
Your instincts are your best tool.
And if your doctor dismisses you? Find another one.
You deserve care that sees you, not just your prescription.
Kathleen Riley
February 9 2026There is no such thing as a ‘generic’ when it comes to neurochemistry.
The brain does not care about FDA guidelines.
It cares about synaptic equilibrium.
And when you disrupt that with a different bead formulation, you are not saving money-you are risking personhood.
Capitalism has colonized psychiatry.
And we are all paying the price in fractured minds.
Diana Dougan
February 10 2026Wow. So the solution is… to pay more? How novel.
Let me guess, next you’ll tell us to stop using insulin generics too.
Some of us can’t afford $800/month for brand-name meds.
Maybe instead of scaring people, we should fix the system that makes generics the only option for most.
Or are you just here to feel morally superior while ignoring the real problem?
PS: I switched generics twice and didn’t die. Just saying.
Natasha Plebani
February 10 2026Pharmacokinetic variance in extended-release psychotropics represents a systemic epistemic failure: the reduction of neurobiological complexity to a binary equivalence metric derived from pharmacoeconomic imperatives.
When bioequivalence thresholds are calibrated for mass-market scalability rather than individual neurochemical fidelity, we are not practicing medicine-we are performing pharmaceutical logistics.
The 80-125% window is not a scientific standard-it is a regulatory compromise born of cost containment ideology.
And in psychiatric polypharmacy, where synergistic modulation of monoaminergic, glutamatergic, and dopaminergic pathways is the therapeutic goal, such variance is not noise-it is signal of destabilization.
Therapeutic drug monitoring should be mandatory, not optional.
Manufacturer-specific prescribing should be standard.
And until then, patients on combination regimens are essentially human clinical trials for corporate cost optimization.
That’s not healthcare.
That’s exploitation dressed in medical jargon.
Yanaton Whittaker
February 11 2026THIS is why America is falling apart.
They let some foreign factory make your brain pills and then wonder why people are crashing.
We used to make quality meds here.
Now we import generics from countries that don’t even have FDA oversight.
My cousin got hospitalized after switching to a generic lithium from India.
They don’t care. They just want to cut costs.
Time to stop buying foreign junk and start making real medicine again.
America First. Brain Health First.