Stroke and Recovery: Effective Rehabilitation After Brain Injury
What Happens After a Stroke?
When a stroke happens, part of the brain loses blood flow and can’t send signals properly. That’s why people might lose movement on one side, struggle to speak, or have trouble swallowing. But here’s the truth: stroke isn’t the end. The brain has an amazing ability to heal itself - if given the right support. Recovery doesn’t mean going back to exactly how you were before. It means learning to live well again, even with changes.
Most people don’t recover fully in a week or even a month. It takes months, sometimes years. And the biggest factor isn’t luck - it’s consistent, smart rehabilitation. The sooner you start, the better. Studies show that starting therapy within 24 hours of a stroke can improve mobility outcomes by 35%. That’s not a small gain. That’s the difference between needing help to walk and walking on your own.
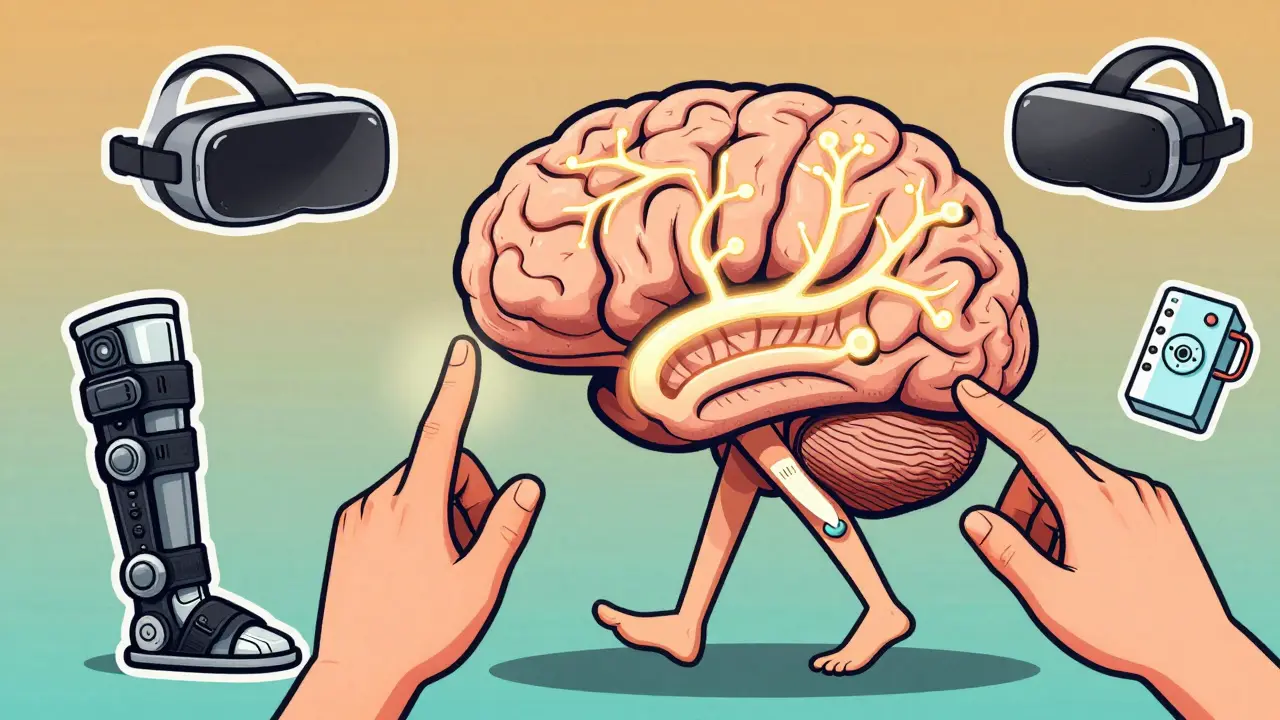
How the Brain Heals: Neuroplasticity Explained
Your brain isn’t a fixed map. It’s more like a city that can rebuild roads after a crash. When one area is damaged, other parts can take over. This is called neuroplasticity. It’s not magic - it’s science. Every time you practice a movement, even a small one like lifting your fingers a few degrees, your brain forms new connections. Functional MRI scans show these changes happening in as little as two weeks.
Think of it like learning to ride a bike. At first, you wobble. But keep trying, and your brain learns the pattern. After a stroke, you’re relearning how to walk, talk, or hold a cup. The repetition is what rewires your brain. That’s why therapists push for hours of practice - not because they’re being tough, but because every rep counts.
The Three Phases of Recovery
Recovery doesn’t happen all at once. It comes in stages, and each one needs a different focus.
Early Recovery (Days to Weeks): Right after the stroke, swelling goes down and the body starts to stabilize. This is when therapists focus on preventing problems - like muscles tightening up (spasticity) or joints freezing from lack of movement. Passive exercises - where someone else moves your arm or leg - are done 2-3 times a day. Positioning matters too. Lying in the wrong way can cause long-term stiffness. Early mobility, even just sitting up in a chair, reduces the risk of blood clots and depression.
Retraining (Weeks to Months): This is where the real work begins. You’re not just moving - you’re learning. Occupational therapists help you practice daily tasks: buttoning a shirt, brushing your teeth, pouring a drink. Physical therapists work on walking, balance, and strength. Speech therapists help with talking and swallowing. You’ll use cues - like pointing to a wheelchair brake - so your brain learns to associate the action with the goal. Small goals are key. Moving your hand 5 degrees more this week? That’s progress.
Adaptation (Months to Years): Some changes are permanent. That’s okay. Adaptation isn’t giving up - it’s adjusting. This stage is about finding new ways to do things. Maybe you use a reacher tool to grab things off high shelves. Maybe you install grab bars in the bathroom. Maybe you use voice commands to control your lights. This is also when emotional support becomes critical. Up to one in three stroke survivors develop depression. Talking to a psychologist isn’t a sign of weakness - it’s part of healing.
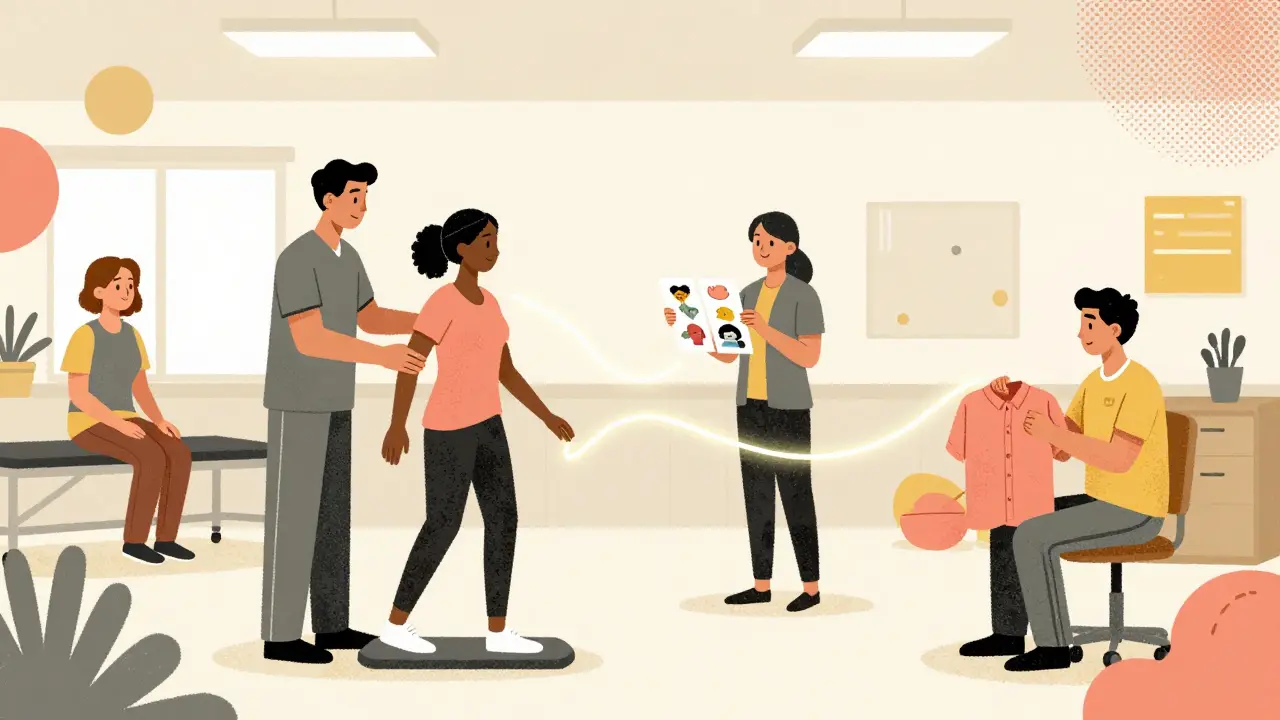
The Team Behind Your Recovery
No single person can do it all. Recovery needs a team. That means doctors, nurses, physiotherapists, speech therapists, occupational therapists, social workers, psychologists, and nutritionists - all working together. And it includes you and your family.
Studies show that facilities with regular team meetings see 22% better outcomes than those without. Why? Because communication matters. If your speech therapist notices you’re struggling to swallow, they need to tell the nutritionist so your meals can be adjusted. If your physical therapist sees you’re too tired to walk, the nurse needs to know to check your blood pressure or sleep patterns. Everyone needs to be on the same page.
Family involvement makes a huge difference. When loved ones help with exercises, attend appointments, and encourage daily routines, patients stick to their rehab plan 37% more often. It’s not about doing everything for you - it’s about walking beside you.
Therapies That Actually Work
Not all therapies are created equal. Some are just busywork. Here are the ones backed by real data:
- Motor-skill exercises: Repeating movements like reaching, grasping, or stepping improves strength and coordination. After 12 weeks, many patients see a 40-60% improvement in walking speed.
- Constraint-induced therapy: If one arm is weaker, you wear a mitt on the stronger arm for 90% of the day. That forces you to use the affected one. Mayo Clinic studies found this leads to 30% more motor improvement than standard care.
- Range-of-motion therapy: Spasticity affects 65-78% of stroke survivors. Stretching and positioning prevent joints from locking up.
- Functional electrical stimulation: Small electrical pulses help weak muscles contract. This can boost wrist and hand strength by 25-45%.
- Robotic therapy: Devices like the Lokomat guide your legs through walking motions. Patients using it improve walking speed by 50% more than those doing only traditional therapy.
- Virtual reality: Playing games in a simulated environment - like catching falling fruit - improves arm function by 28% compared to standard exercises.
- Wireless activity monitors: These track your steps. Just seeing your daily count increases movement by 32%. Accountability works.
Technology isn’t replacing therapists - it’s giving them better tools. And it’s making therapy more engaging. Who wouldn’t rather play a game than do 50 repetitive arm lifts?
How Much Therapy Is Enough?
The American Stroke Association says medically stable patients should get three hours a day, five days a week in an inpatient rehab setting. That’s not a suggestion - it’s the standard for best results. But not everyone can stay in a facility. That’s where outpatient and telerehabilitation come in.
Recent studies show telerehabilitation - therapy done over video calls - is 85% as effective as in-person sessions for many tasks. You can do balance exercises, speech drills, or arm training from your living room. All you need is a tablet and a quiet space. For people in rural areas or with transportation issues, this is life-changing.
Balance training is especially important. Six in ten stroke survivors have trouble with balance. That means a high risk of falling. A structured program - standing on one foot, shifting weight, stepping over lines - reduces fall risk by nearly half.

The Nine Factors That Make or Break Recovery
Recovery isn’t just about therapy. Nine things determine how well you do:
- Your overall health before the stroke
- How much movement you still have
- Your muscle strength
- Control over bladder and bowels
- What your life was like before - were you active? Independent?
- Your home and social support
- How quickly you learn new things
- Your motivation
- Your ability to cope with change
Of all these, motivation is the biggest predictor. Studies show it accounts for up to 40% of recovery success. You can have the best therapist, the latest tech, and perfect care - but if you don’t believe you can get better, progress stalls. That’s why celebrating small wins matters. Did you stand up without help today? That’s a victory.
What About the Future?
Research is moving fast. Transcranial magnetic stimulation (TMS) - a non-invasive brain stimulation technique - is showing 15-20% greater motor recovery when added to therapy. Medications that boost brain-derived neurotrophic factor (BDNF), a protein that helps neurons grow, are in trials. Artificial intelligence is being used to create personalized rehab plans based on your brain scans and movement patterns.
And community-based programs are becoming more common. Most stroke survivors need ongoing support after leaving the hospital. Group classes, walking clubs, and home visits help keep people active and connected. Isolation kills progress. Social interaction isn’t a luxury - it’s medicine.
What You Can Do Right Now
If you or someone you love has had a stroke:
- Start rehab as soon as doctors say it’s safe - don’t wait.
- Ask about the team: Who’s involved? Are they communicating?
- Set tiny, daily goals. Progress isn’t always big.
- Include family. They’re part of your care team.
- Move every day - even if it’s just shifting in your chair.
- Rest when you’re tired. Fatigue slows healing.
- Don’t ignore your mood. Depression is common and treatable.
- Use tech if it helps - apps, monitors, video calls.
Recovery isn’t linear. Some days you’ll feel strong. Others, you’ll feel stuck. That’s normal. What matters is that you keep going. The brain doesn’t heal on a schedule - it heals when you give it the chance, every single day.




8 Comments
Edith Brederode
January 18 2026I’ve been doing telerehab for 8 months now and it’s literally saved my life. My therapist sends me VR games to play while I’m on the couch. I didn’t think I’d ever move my hand again, but now I can hold my coffee cup without spilling. 🙌
clifford hoang
January 20 2026They’re hiding the truth. Neuroplasticity? Nah. The brain doesn’t ‘rebuild roads’-it’s all electromagnetic frequency manipulation by Big Pharma and the WHO. They want you dependent on ‘therapy’ so they can sell you devices. Look at the stats-every rehab center is owned by a hospital conglomerate. 🤔
Arlene Mathison
January 20 2026Okay but seriously-celebrating the tiny wins changed everything for me. I used to cry because I couldn’t button my shirt. Then one day I did it. Just. One. Button. I danced in my kitchen like a maniac. That’s the real victory. Not the 50% improvement stats. The joy. 💃
Carolyn Rose Meszaros
January 21 2026This post made me cry. My mom had a stroke last year and I didn’t know how to help. Now I sit with her every morning and we do 5 minutes of arm stretches. She smiles now. Not because she’s ‘better’-but because she feels seen. Thank you for writing this. 🫂
Greg Robertson
January 21 2026I’m a PT and I just want to say-yes, three hours a day is the gold standard. But if you’re doing 45 minutes at home with your spouse? That’s still huge. Don’t let anyone make you feel like you’re not doing enough. Consistency > intensity. You’re doing better than you think.
Nadia Watson
January 22 2026It is of paramount importance to underscore that the rehabilitation paradigm must be holistic, encompassing not only the somatic dimensions but also the psychosocial and existential dimensions of recovery. The integration of community-based social support structures is not ancillary-it is foundational. One must not underestimate the therapeutic efficacy of sustained interpersonal engagement, as isolation engenders neurochemical degradation. Furthermore, the utilization of assistive technologies must be guided by patient autonomy, not institutional convenience. A thoughtful, dignified approach is non-negotiable.
Shane McGriff
January 22 2026I’ve seen too many people give up after three months because ‘they didn’t see results.’ But recovery isn’t a sprint-it’s a slow burn. My brother didn’t walk again until 14 months out. He had zero hope. Then one day he stood up to turn off the TV. No one was there. Just him. That’s when I knew he was going to make it. Keep going. Even when it feels pointless.
Jacob Cathro
January 22 2026LMAO at the ‘robotic therapy’ and ‘VR’ stuff. All that fancy tech and they still can’t fix the fact that most stroke patients are just old and tired. They’re selling hope like it’s a subscription box. I’ve seen 80-year-olds doing 3 hours of rehab daily. They’re exhausted. The real therapy? Letting them rest. And maybe a good nap. 😴