Anticonvulsant Medications: Types, Uses, and Safety Tips
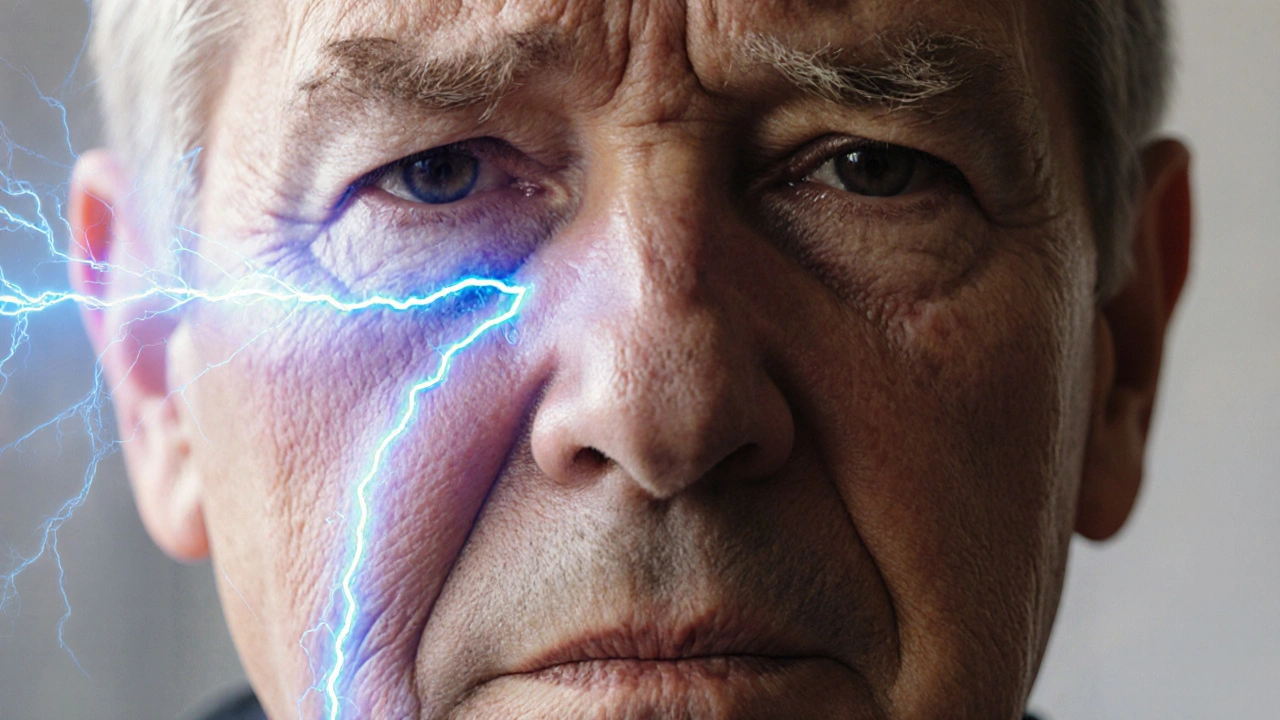
When dealing with anticonvulsant medications, drugs designed to prevent or lessen the frequency of seizures. Also known as seizure control drugs, they play a central role in managing conditions where abnormal brain activity triggers convulsions.
One of the most common conditions they target is epilepsy, a chronic neurological disorder characterized by recurring seizures. Epileptic seizures can vary from brief lapses in awareness to full‑body convulsions, and the choice of medication often hinges on the seizure type. Closely related is the broader category of seizure disorders, which includes epilepsy as well as less‑common syndromes such as febrile seizures or panic‑induced episodes. Understanding the specific disorder helps clinicians match the right drug to the right patient, reducing trial‑and‑error and speeding up seizure control.
Key Factors to Consider When Choosing an Anticonvulsant
Beyond the diagnosis, three practical pillars shape the prescribing decision: side‑effect profile, drug‑interaction risk, and therapeutic drug monitoring. Drug side effects, adverse reactions ranging from mild fatigue to serious rash or liver issues, differ markedly between agents. For example, sodium channel blockers often cause dizziness, while enzyme‑inducing drugs may affect cholesterol or bone health. Monitoring these effects early can prevent discontinuation.
Because many anticonvulsants affect liver enzymes, they can clash with other prescriptions, over‑the‑counter meds, or even certain foods. This drug interaction, the way one medication alters the metabolism of another, is especially relevant for patients on anticoagulants, oral contraceptives, or psychiatric drugs. A clear medication list and a quick check with a pharmacist often save headaches later.
Finally, most older anticonvulsants require therapeutic drug monitoring, regular blood tests to keep drug levels within a safe, effective range. Maintaining the sweet spot helps avoid breakthrough seizures while minimizing toxicity. Newer agents may need less frequent checks, but doctors still look for signs of accumulation, especially in kidney‑impaired patients.
Dosage is another piece of the puzzle. Starting low and titrating up slowly is the standard approach, allowing the body to adapt and giving providers a chance to spot side effects early. Pediatric dosing often follows weight‑based formulas, while elderly patients may need reduced amounts due to slower metabolism.
When you weigh these factors—diagnosis, side‑effect tolerance, interaction potential, and monitoring needs—you get a clearer picture of which anticonvulsant fits best. Below you’ll find articles that break down specific drugs, compare brand‑name versus generic options, and share real‑world tips for living with seizure control therapy.
A clear, evidence‑based guide on how anticonvulsant drugs like carbamazepine and oxcarbazepine treat trigeminal neuralgia, including effectiveness rates, side‑effects, dosing tips and FAQs.
Continue Reading