Diuretics for Hypertension: What You Need to Know
Diuretics are one of the oldest and most used medicines for high blood pressure. They help the body remove extra salt and water, which lowers blood volume and eases pressure on the heart. If your doctor mentioned diuretics, here’s a clear, practical guide to what they do, the main types, side effects, and simple tips to use them well.
How diuretics work and main types
Think of diuretics as helpers that make your kidneys dump excess fluid. There are three common groups used for hypertension:
- Thiazide and thiazide-like diuretics: These are first-line for many people with high blood pressure. Examples are hydrochlorothiazide (HCTZ), chlorthalidone, and indapamide. They work well at low doses and often cut heart attack and stroke risk when combined with other medicines.
- Loop diuretics: Furosemide is the classic one here. Loops are stronger and used when fluid builds up in the lungs or legs (heart failure, kidney disease). They lower blood pressure too but are mainly for fluid control.
- Potassium-sparing diuretics: Spironolactone and eplerenone keep potassium from being lost. They’re useful when potassium drops or in specific conditions like resistant hypertension. Watch for high potassium with these, especially when combined with ACE inhibitors or potassium supplements.
Practical tips, side effects, and monitoring
Want to avoid surprises? Take diuretics in the morning to cut down on nighttime bathroom trips. Stay consistent with dosing and follow up with your clinician for simple blood tests: potassium, sodium, and creatinine are the main ones. These checks catch low potassium, low sodium, or kidney changes early.
Common side effects include increased urination, dizziness (especially when standing up fast), and muscle cramps. Thiazides can raise blood sugar, uric acid, and cholesterol a bit—so people with diabetes or gout need closer monitoring. Spironolactone can cause breast tenderness or changes in hormones for some people.
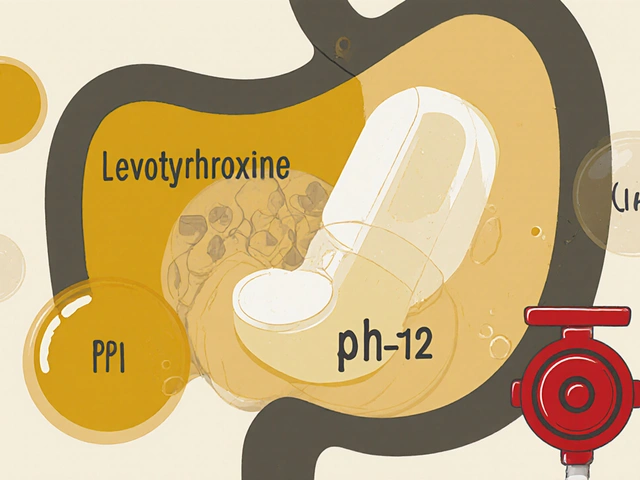
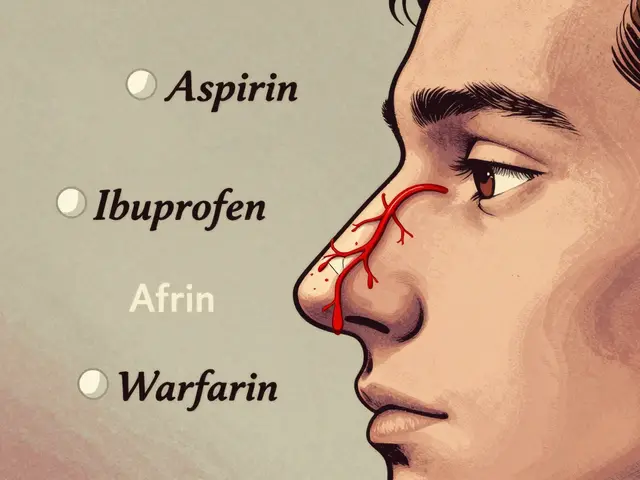
Drug interactions matter: NSAIDs like ibuprofen can make diuretics less effective. Combining potassium-sparing diuretics with ACE inhibitors or ARBs raises the risk of high potassium. Tell your doctor about all meds and supplements so they can adjust doses safely.
Who should be cautious? Older adults need slower dose changes because they’re more likely to get low sodium or dehydration. If you’re pregnant or breastfeeding, talk to your provider—some diuretics aren’t recommended during pregnancy.
Diuretics work best with lifestyle changes. Cut back on salt, keep active, lose weight if needed, and limit alcohol. These actions often let your medication work better or allow a lower dose.
If you feel faint, have very irregular heartbeat, severe muscle weakness, sudden swelling, or unusually low urine output, contact your healthcare provider right away. Diuretics are safe for millions, but like any medicine, they need smart use and periodic checks.
Want help understanding your specific diuretic or lab results? Bring them to your next visit and ask for plain answers about dose, side effects, and what to watch for.

Lasix alternatives, such as Torsemide, Bumetanide, and Chlorthalidone, provide effective treatment for conditions like edema and hypertension. Each option comes with its own set of pros and cons, making it essential to understand which might be most suitable for individual needs. From loop diuretics to potassium-sparing options, these medications significantly impact fluid retention and blood pressure management. Additionally, Valsartan offers a unique approach as an angiotensin II receptor blocker, extending therapeutic choices for heart failure and hypertension. This article provides a comprehensive comparison of these alternatives to aid informed decision-making.
Continue Reading