DOAC Bleeding: What You Need to Know About Risks and Management
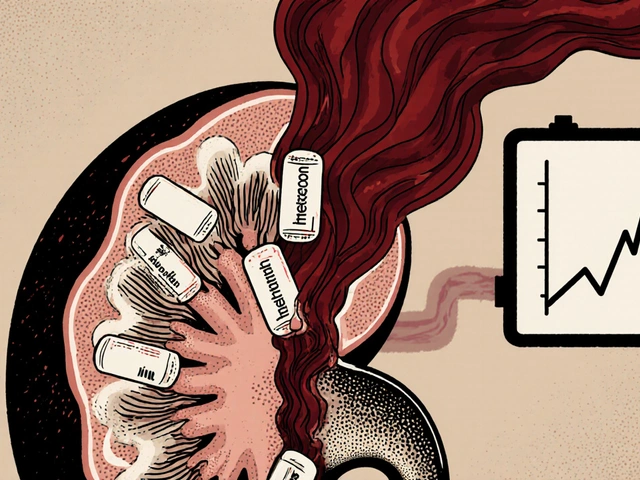
When you take a direct oral anticoagulant, a type of blood thinner used to prevent clots in people with atrial fibrillation, deep vein thrombosis, or pulmonary embolism. Also known as DOAC, it works by blocking specific clotting factors in your blood—making it harder for dangerous clots to form. But this same mechanism is what makes DOAC bleeding a real concern. Unlike older blood thinners like warfarin, DOACs don’t need regular blood tests, but they also don’t have a simple antidote for every situation. That’s why knowing the risks and what to do if bleeding happens is just as important as taking the pill.
DOAC bleeding isn’t rare. Studies show that about 1 to 3 out of every 100 people taking these drugs each year will have a serious bleed—like a stomach bleed, brain bleed, or major bruising that won’t stop. The risk goes up if you’re older than 75, have kidney problems, take other meds like NSAIDs or aspirin, or have a history of ulcers or falls. Some DOACs, like dabigatran, are more likely to cause stomach bleeding, while others, like rivaroxaban, carry a slightly higher risk of brain bleeds. And if you’re on more than one blood thinner, your risk multiplies. It’s not about fear—it’s about awareness. Your doctor checks your kidneys, your fall risk, and your other meds before prescribing a DOAC for a reason.
What happens if you start bleeding? The first step is to stop the bleeding—apply pressure, stay calm, and get help. In hospitals, doctors have reversal agents for some DOACs: idarucizumab for dabigatran, and andexanet alfa for factor Xa inhibitors like apixaban and rivaroxaban. But these aren’t always available, and they’re expensive. That’s why prevention matters more than cure. If you’re on a DOAC, avoid alcohol-heavy nights, skip ibuprofen, use an electric razor, and tell every doctor you see—dentist, surgeon, even your physical therapist—that you’re on a blood thinner. Many people don’t realize that even a minor procedure like a tooth extraction can turn dangerous if your doctor doesn’t know you’re on a DOAC.
What you’ll find in the posts below isn’t just theory. It’s real-world insight from people who’ve dealt with medication risks—like how kidney disease makes drugs build up and turn toxic, how drug interactions can sneak up on you, and how even common heartburn meds can interfere with your treatment. You’ll see how doctors think about balancing clot prevention with bleeding danger, and what steps actually work to stay safe. This isn’t about scaring you. It’s about giving you the facts so you can talk smarter with your doctor and make choices that fit your life.

Severe bleeding from blood thinners like apixaban or warfarin can be life-threatening. Learn the warning signs, who’s at highest risk, and exactly what to do in an emergency-backed by 2025 clinical guidelines and real patient data.
Continue Reading