Exercise, Meds, and Moving Better
Exercise does more than burn calories. It changes blood sugar, affects inflammation, shifts mood, and can alter how some medicines work. That matters if you take drugs for diabetes, asthma, pain, blood thinners, or mental health. Small changes in what you do can make a big difference in how safe and effective your treatment is.
How exercise helps — and when to be careful
For people on diabetes meds like metformin, regular activity can improve blood sugar control and even mimic parts of exercise at the cellular level. A recent study showed metformin activates pathways similar to intense workouts, which helps explain why combining the drug with steady exercise often gives better weight and glucose results.
If you use inhalers, a short-acting bronchodilator before workouts can prevent exercise-triggered asthma. For arthritis or gout, low-impact movement—walking, swimming, cycling—reduces stiffness and keeps joints moving without making pain worse. But during a gout flare, skip intense sessions until swelling eases.
Blood thinners such as rivaroxaban lower clot risk but raise bleeding risk. That means avoiding high-contact sports and taking extra care with activities that could cause falls. NSAIDs like diclofenac or Celebrex help pain but can hide injury pain and cause stomach or heart risks when used heavily. Relying only on painkillers to push through pain is risky.
Mental health meds interact with exercise too. Movement often helps mood and cognition, sometimes boosting medication effects. Still, some antidepressants can cause dizziness or fatigue—start slow and watch how your body reacts.
Practical, no-nonsense tips to exercise safely with meds
1) Tell your provider what you do. Share your typical workout, not just “I exercise.” That helps them pick meds and doses that fit your routine.
2) Start slow after a med change. New drugs can alter balance, heart rate, or energy. Give your body a week of easy sessions before pushing intensity.
3) Time meds smartly. For asthma, use a rescue inhaler before activity. For drugs that cause dizziness, try taking them after workouts or at bedtime—ask your clinician first.
4) Watch for red flags: unusual bruising on blood thinners, severe shortness of breath with inhaler use, or sudden pain masked by NSAIDs. If anything feels off, stop and call your healthcare provider.
5) Pick safe activities. Swimming, cycling, brisk walking, and resistance bands give results with lower injury risk. If you have joint pain, water workouts are often the best starting point.
Exercise is one of the best tools alongside medication. Use it wisely: communicate with your provider, listen to your body, and adjust when needed. Check the related articles on this site for specifics—like metformin and weight loss, inhaler options, rivaroxaban, or pain meds for gout—to match exercise tips to your treatment.
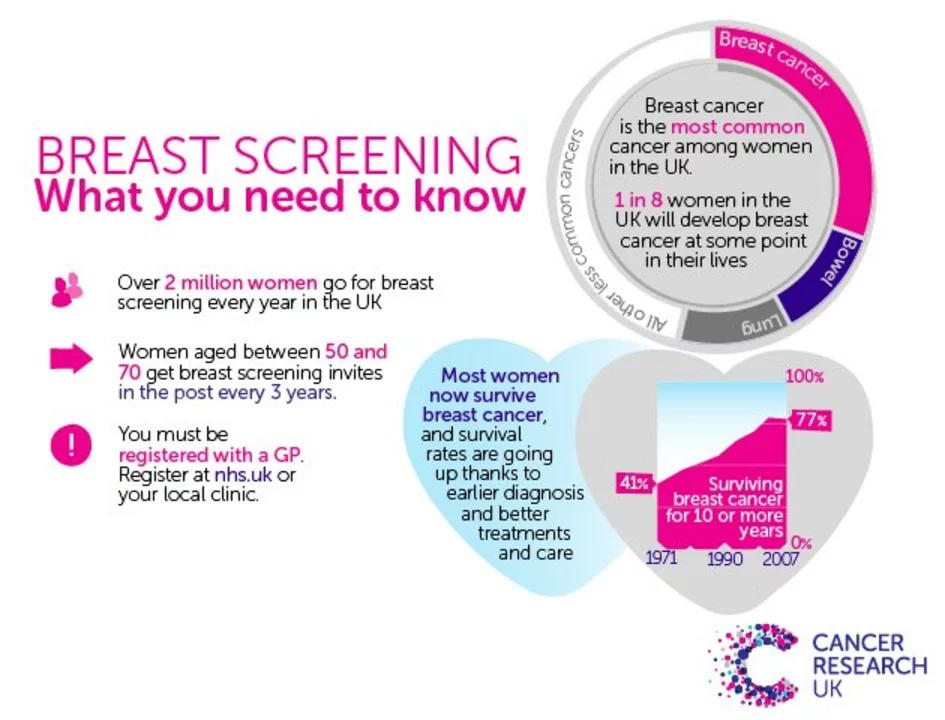
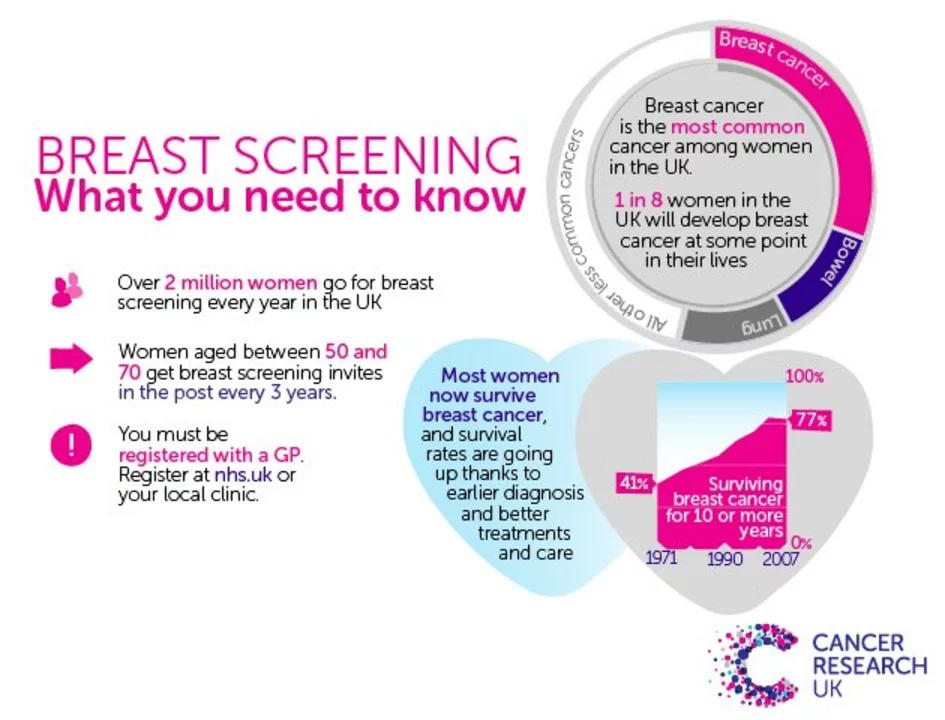
As a blogger, I've come to understand the importance of exercise in our lives, especially for women. Recent studies have shown that engaging in regular physical activity can play a significant role in both the prevention and recovery from breast cancer. This is because exercise helps maintain a healthy body weight and boosts the immune system, which can lower the risk of developing the disease. Additionally, it has been proven that exercise can improve mood and energy levels, which are crucial factors in the recovery process. So ladies, let's get moving and take charge of our health!
Continue Reading