Graft‑Versus‑Host Disease (GVHD): What to Watch For After a Transplant
If you or someone you care for had a stem cell or bone marrow transplant, GVHD is a real concern. GVHD happens when donor immune cells attack the recipient’s tissues. That sounds scary, but knowing the signs, when to call the transplant team, and what treatments are available makes a big difference.
GVHD comes in two main types: acute and chronic. Acute GVHD usually appears in the first 100 days after transplant. It mostly hits the skin, gut, and liver. Chronic GVHD shows up later and can affect many organs, cause dry mouth and eyes, joint stiffness, or lung issues. Timing gives doctors a big clue, but symptoms and tests confirm the diagnosis.
Signs, tests, and when to act
Watch for new rashes, itchy or blistering skin, persistent diarrhea, belly pain, or yellowing of the skin (jaundice). For chronic GVHD, look for long-lasting cough, shortness of breath, tightening of skin, or new dryness in mouth and eyes. Don’t shrug off subtle changes—early calls to your transplant center can speed up care.
Doctors use blood tests (liver enzymes), stool checks, and biopsies of skin or gut to confirm GVHD. Biopsy results help decide how aggressive treatment should be. If tests are unclear, your team may try short-term treatment while monitoring closely.
Treatment options and practical tips
First-line treatment for many acute cases is steroids like prednisone to calm the immune attack. For steroid-resistant cases, newer drugs and approaches are used. Ruxolitinib is now an approved option for steroid-refractory acute GVHD. Chronic GVHD has its own set of tools: steroids, calcineurin inhibitors (for example, tacrolimus or cyclosporine), ibrutinib for some chronic cases, and extracorporeal photopheresis (ECP) for skin or lung involvement.
Supportive care matters. Keep skin moisturized, protect from sun, use gentle soaps, and report any signs of infection right away—GVHD and its treatments lower your infection defenses. Nutrition matters too: severe gut GVHD can cause poor absorption, so dietitians often help with plans or temporary tube feeding.
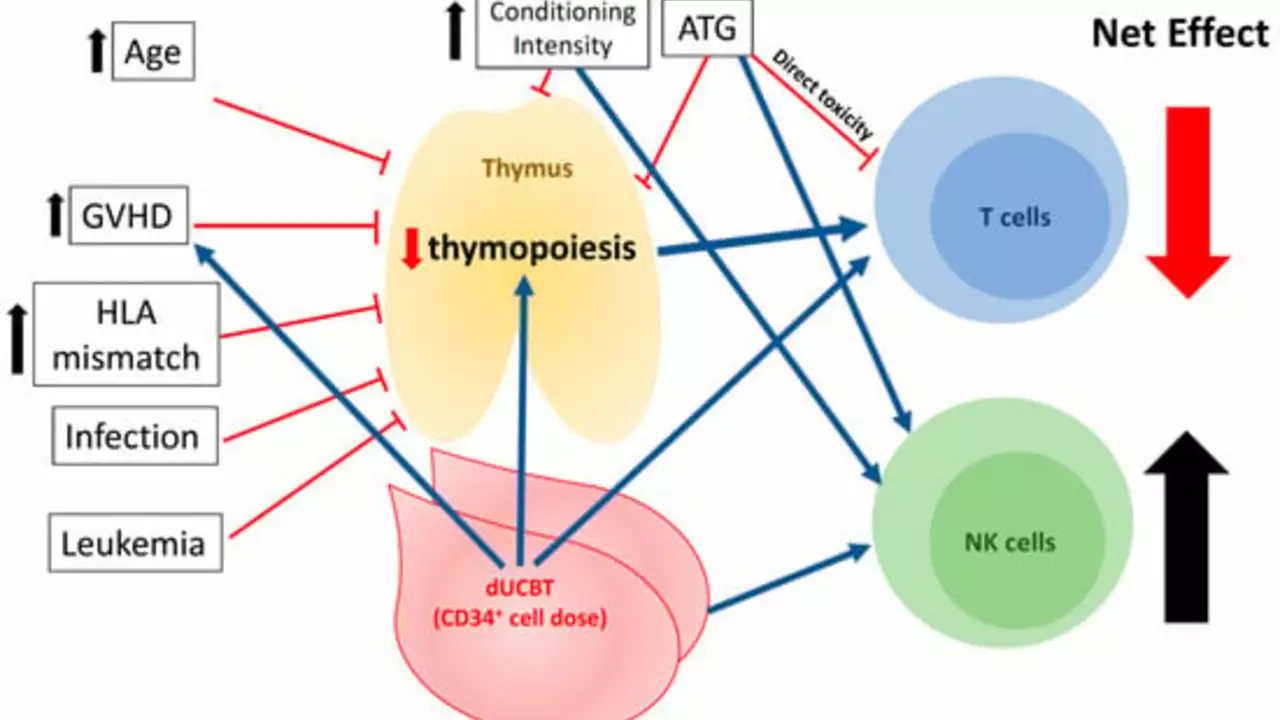
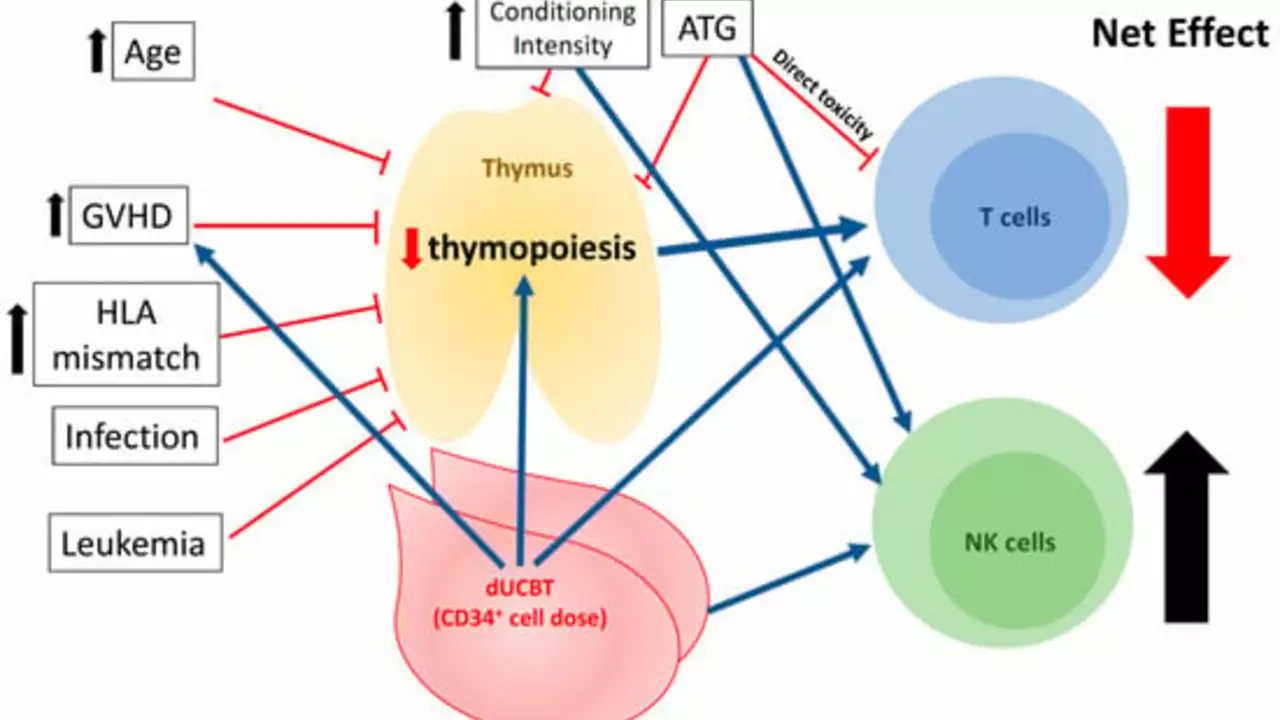
Prevention starts before transplant. Better donor matches, careful conditioning regimens, and prophylactic drugs like methotrexate or calcineurin inhibitors lower GVHD risk. Your transplant team will explain the balance between preventing GVHD and avoiding too much immune suppression, which raises infection risk.
Questions to ask your team: What type of GVHD is most likely for me? Which symptoms require an urgent call? What are the side effects of proposed treatments? Having clear answers makes decisions easier during stressful moments.
GVHD can be serious, but many people respond well when it’s caught early. Stay alert to changes, keep close contact with your transplant center, and follow their guidance on meds, skin care, and infection prevention.
After delving into the topic, I've learned that lenalidomide is increasingly being utilized in the management of graft-versus-host disease (GVHD). This is a common complication following a bone marrow or stem cell transplant, where the donor cells start to attack the patient's body. Lenalidomide has shown promising results in mitigating this reaction, helping to improve patient outcomes. There's definitely more research needed here, but the initial results are encouraging. So, in the future, we may see lenalidomide becoming a standard part of GVHD treatment.
Continue Reading