Batch Release Testing: Final Checks Before Pharmaceutical Distribution
Every pill, injection, or capsule that reaches a pharmacy shelf has passed through one final, non-negotiable gate: batch release testing. This isn’t just paperwork. It’s the last line of defense between a patient and a potentially dangerous product. If a batch fails here, it never leaves the factory. No exceptions.
What Exactly Happens During Batch Release Testing?
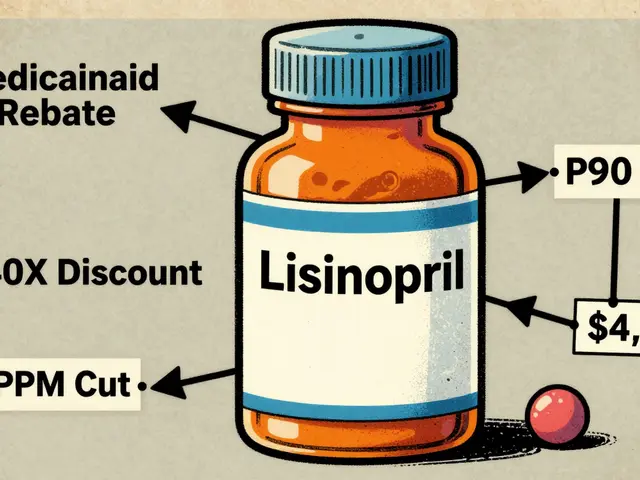
Batch release testing is a full forensic review of every single batch of medicine before it’s shipped. Think of it like a final inspection on a car before it rolls off the assembly line-but instead of checking paint scratches, you’re verifying that the active ingredient is at the exact right strength, that no toxic impurities are hiding in the mix, and that the product won’t grow mold or bacteria in your medicine cabinet. For each batch, labs run a set of standardized tests. These aren’t optional. They’re written into law by the FDA, EMA, and other global regulators. Common tests include:- Identity testing: Does this tablet contain the right drug? HPLC or NMR machines confirm the chemical fingerprint matches the approved formula.
- Assay/potency: Is there enough active ingredient? The acceptable range is usually 90-110% of the labeled amount. Too little? The medicine won’t work. Too much? It could be dangerous.
- Impurity profiling: Are there any unwanted chemicals? ICH guidelines limit unknown impurities to 0.10% in new drugs. Even tiny amounts can cause allergic reactions or long-term harm.
- Microbial limits: Is the product clean? For non-sterile products, no more than 100 colony-forming units per gram are allowed. Sterile products? Zero tolerance.
- Dissolution: Will the pill break down properly in your body? Generic drugs must match the brand-name version’s dissolution profile with an f2 similarity factor of at least 50.
- Endotoxin and particulate testing: Especially critical for injectables. A single contaminated vial can cause sepsis.
Why Is This So Strict? The Human Cost of Failure
One failed batch can cost millions-and lives. In 2023, the FDA reported that pharmaceutical recalls averaged $10.7 million per incident. But money isn’t the real cost. In 2022 alone, batch release testing blocked about 1,200 unsafe drug batches from reaching U.S. patients, according to former FDA director Dr. Jane Smith. That’s 1,200 chances to avoid poisoning, organ damage, or death. The most common failure points? Dissolution (32%), impurities (28%), and microbial contamination (23%). A single batch of a monoclonal antibody with subpotent levels was released in 2023 due to poor review procedures. The result? 12,000 vials recalled, a $9.2 million loss, and an 18-month import ban on the facility. This isn’t theoretical. People die when these checks slip. That’s why regulators demand double-checks: two analysts must independently review every test result before a batch is approved.Who Signs Off? The Qualified Person (QP)
In the European Union, no batch can leave the factory without a Qualified Person (QP) signing off. The QP isn’t just a manager-they’re a legally accountable expert with at least five years of GMP experience and formal certification. They don’t just look at numbers. They verify the entire manufacturing process was followed, documentation is complete, and deviations were properly investigated. The problem? Europe is short by 32% of qualified QPs, according to the EMA’s 2024 report. This creates bottlenecks. A complex biologic batch can take 40-60 hours just to review the paperwork. Some companies are now hiring QPs from outside the EU, but training takes 18-24 months. There’s no shortcut. In the U.S., there’s no single QP role, but the Quality Unit must certify the batch. The standards are just as strict.
Technology Is Changing How Testing Is Done
Traditional batch release testing takes days-or weeks-for biologics. But new tools are emerging. Some companies now use Process Analytical Technology (PAT) to monitor quality in real time during manufacturing. The FDA launched a pilot in 2025 for “predictive release testing,” allowing certain facilities to skip final lab tests if real-time data proves consistency. Only 12 companies qualified by October 2025. Others use AI to predict batch success based on historical data. One manufacturer cut batch failures by 34% using machine learning. But regulatory approval for these systems takes 18 months. And the FDA still demands 99.9% confidence before fully accepting them. Laboratory Information Management Systems (LIMS) are also making a difference. Companies using integrated LIMS reported 22% faster release cycles. Thermo Fisher’s SampleManager was cited in 41% of those success stories.The Hidden Struggles: Data, Training, and Delays
Behind the scenes, quality teams fight daily battles. - Method transfer failures: When R&D hands off a test to manufacturing, 78% of QC analysts say it goes wrong. Average fix time? 14.7 business days. - Data integrity issues: 31% of FDA 483 observations cite missing or altered records. A single unsigned printout can delay a batch for weeks. - Documentation overload: For biologics, you need 42 specific data points per batch. Paper records are gone-electronic batch records are now mandatory for firms with over $1 million in annual sales. On forums like Biophorum and Reddit, quality professionals say staffing is the biggest problem. One analyst wrote: “I’m reviewing three batches at once. I’m not sleeping. I’m terrified I’ll miss something.”Regulatory Differences: U.S. vs. EU vs. China
Global drug supply chains mean one batch might be made in India, tested in Germany, and sold in Canada. But rules vary. - The EU requires full testing on every batch. No exceptions. - The FDA allows reduced testing for manufacturers with proven process control-especially in continuous manufacturing facilities. - China’s NMPA now requires batch release testing for all imported vaccines, adding 14-21 days to the timeline. This divergence makes global compliance a nightmare. A company can’t just follow one set of rules. They must map every test to every jurisdiction’s requirements.
Costs Are Rising-and So Are Expectations
The global batch release testing market hit $2.8 billion in 2024 and is growing at 6.7% per year. Why? Because products are getting more complex. - Small molecule generics: 7-10 days to release - Complex generics: 14-21 days - Biologics: 21-35 days Testing costs have risen 22% since 2020. Why? More sensitive instruments, stricter limits, and longer stability studies. A single stability run for a biologic can take three years. New guidelines are making things even harder. As of January 1, 2025, USP <1033> requires full biological assay validation for all potency tests. ICH Q14 (effective November 2024) lets companies design smarter, risk-based tests-but only if they can prove the change won’t compromise safety.What’s Next? The Future of Batch Release
By 2028, McKinsey predicts 45% of batch release decisions will use AI-driven analytics. But regulators are cautious. The EMA’s 2024 pilot found AI matched traditional methods 78% of the time. The FDA wants 99.9%. The real shift? Moving from “batch testing” to “continuous quality verification.” Facilities using advanced manufacturing may only test 1 in 10 batches by 2030. But for now, 97% of industry experts agree: some form of discrete batch verification will still be needed through 2040. The goal isn’t to eliminate testing. It’s to make it smarter, faster, and more reliable-without ever compromising patient safety.Final Thought: It’s Not About Compliance. It’s About Trust.
Patients don’t know what batch release testing is. They shouldn’t have to. But when they take a pill, they trust it’s safe. That trust is built on thousands of hours of lab work, signed reports, and people who refuse to cut corners. This isn’t just a regulatory step. It’s a moral one.Is batch release testing required by law?
Yes. It’s legally required in every major pharmaceutical market, including the U.S. (21 CFR 211.165), the EU (Directive 2003/94/EC), and China. No batch can be legally distributed without passing all required tests and receiving formal certification.
What happens if a batch fails release testing?
The batch is quarantined and held for investigation. If the failure can’t be explained or corrected, the batch is destroyed. In rare cases, if the issue is minor and fixable (like a labeling error), it may be reworked under strict supervision-but only if regulators approve.
How long does batch release testing take?
It varies by product type. Small molecule generics take 7-10 days. Complex generics and injectables take 14-21 days. Biologics, like monoclonal antibodies, can take 21-35 days due to complex stability and potency tests. Some companies use predictive methods to reduce this, but full testing remains standard.
Who is responsible for batch release in the EU?
A Qualified Person (QP), a certified expert with at least five years of GMP experience. The QP must review all test results, manufacturing records, and deviations before signing off. They are legally liable if a defective batch is released.
Can AI replace human reviewers in batch release?
Not yet. AI can help predict outcomes, flag anomalies, and speed up data review-but final approval still requires human oversight. Regulators like the FDA require near-perfect accuracy (99.9%) before allowing AI to make release decisions. Human judgment is still needed to interpret context, investigate root causes, and ensure ethical compliance.
Why are testing costs rising?
Newer drugs (like biologics and gene therapies) require more complex, sensitive, and time-consuming tests. Stricter regulatory limits on impurities, increased documentation requirements, and the need for real-time environmental monitoring have all added to costs. Since 2020, average testing expenses have risen by 22%.
What’s the biggest cause of batch release delays?
Method transfer failures between R&D and manufacturing teams. When a test developed in the lab doesn’t work the same way on the production floor, it causes delays. This is cited as the top issue by 78% of quality control professionals, with an average resolution time of nearly 15 business days.
Do all batches of a drug get tested the same way?
Yes, for traditional manufacturing. Every batch must pass the same set of tests defined in the marketing authorization. However, under new continuous manufacturing models, the FDA allows reduced testing if real-time data proves consistent quality-only approved for select facilities as of 2025.




12 Comments
Sohini Majumder
December 1 2025Okay but like... who even HAS the time to review 42 data points per batch??? I’m just here for the pills and the vibes. 😩
tushar makwana
December 2 2025This is so important. People don’t realize how much work goes into every pill. I’m from India, and we rely on these medicines too. Thank you to the people doing this work.
Richard Thomas
December 2 2025The regulatory architecture underpinning batch release protocols constitutes a non-negotiable bulwark against systemic pharmaceutical failure. The confluence of ICH guidelines, GMP compliance, and QP accountability reflects an epistemological commitment to patient safety that transcends mere bureaucratic formalism. To entertain the notion of algorithmic substitution without 99.9% confidence is not merely imprudent-it is ontologically reckless.
Peter Lubem Ause
December 2 2025You’re right to highlight the QP shortage. In Nigeria, we wait weeks for some medicines just because there aren’t enough certified people to sign off. This isn’t just a US/EU problem-it’s global.
linda wood
December 3 2025So let me get this straight… we have AI that can predict if a batch will pass… but humans still have to stare at spreadsheets for 40 hours because ‘trust’? Bro. We’re doing this wrong.
LINDA PUSPITASARI
December 4 2025I work in QC and this post made me cry 😭 Seriously-every time I sign off on a batch, I think of someone’s grandkid taking it. The data overload? Yeah. The stress? Oh yeah. But this matters. 🙏
gerardo beaudoin
December 4 2025Method transfer failures are the real villain here. I’ve seen labs spend months fixing a simple HPLC method because R&D didn’t document the solvent temp. It’s not sexy, but it’s everything.
Joy Aniekwe
December 6 2025Oh wow. So the ‘Qualified Person’ is the only human between me and a lethal batch? And we’re short 32% of them? I feel safer already. 🙃
Latika Gupta
December 8 2025I read this whole thing. I’m not sure what to say. I just… I just hope they’re not rushing.
Sullivan Lauer
December 9 2025This is the most important thing happening in healthcare and NO ONE is talking about it. Think about it-every time you swallow a pill, you’re trusting a person who spent 60 hours verifying a number on a screen. That’s heroism. That’s dignity. That’s the quiet backbone of modern medicine. We owe them everything.
Matthew Higgins
December 10 2025I used to think this was just corporate bureaucracy. Then my mom got a bad batch of generic blood pressure meds. She ended up in the ER. This isn’t theory. It’s life or death. Thanks for writing this.
Mary Kate Powers
December 11 2025I’m so proud of the people doing this work. Even if no one sees it, even if no one thanks you-you’re keeping people alive. Keep going. We see you.