Causality Assessment for Adverse Drug Reactions: How the Naranjo Scale Works in Real-World Practice
What Exactly Is the Naranjo Scale?
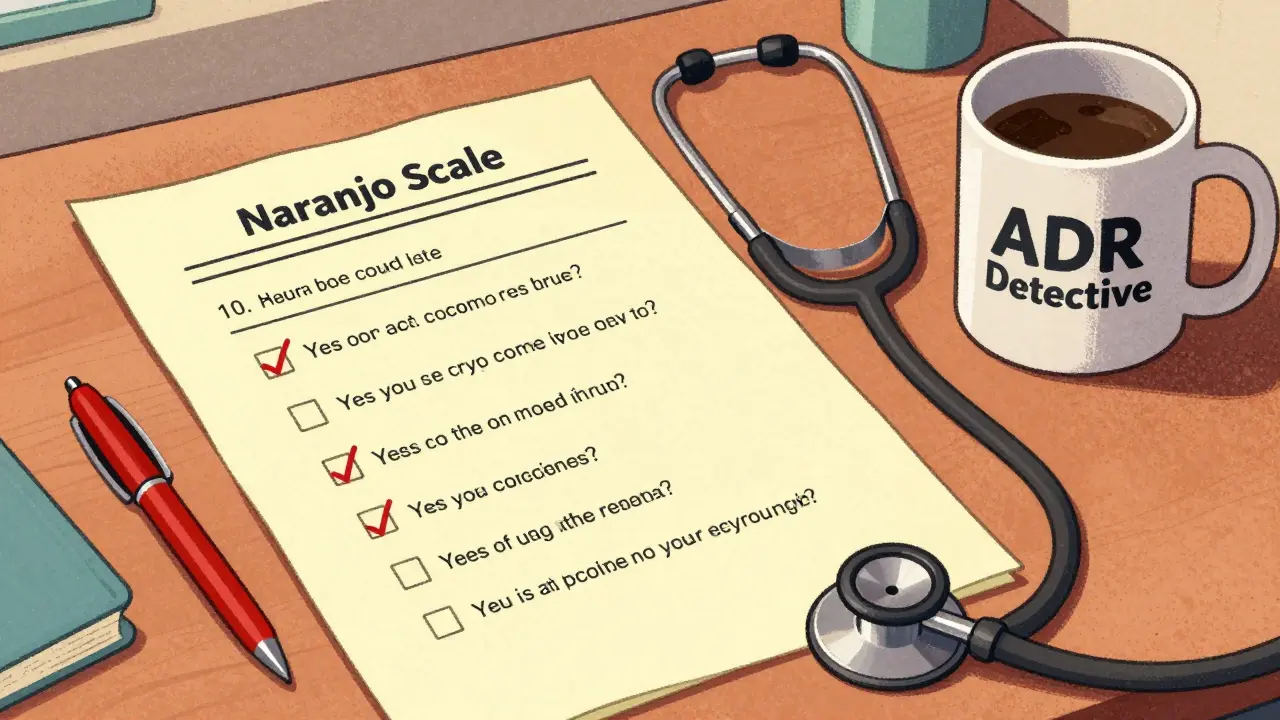
The Naranjo Scale is a standardized, 10-question tool used by healthcare professionals to determine whether an adverse drug reaction (ADR) was likely caused by a specific medication. It was first published in 1981 by Dr. Carlos A. Naranjo and his team in Clinical Pharmacology and Therapeutics. Before this, doctors often guessed whether a side effect was due to a drug or something else-like an infection, another medication, or the patient’s underlying condition. The Naranjo Scale changed that by turning guesswork into a clear, repeatable process.
It’s not a fancy algorithm or a high-tech device. It’s a simple checklist you can use on paper, in an electronic form, or even in your head. But don’t let its simplicity fool you. This tool is used in hospitals, pharmacies, and regulatory agencies around the world to decide if a patient’s bad reaction to a drug was actually caused by the drug.
How the Naranjo Scale Scores Your ADR
The scale has 10 yes-or-no questions. Each answer gets a score: +2, +1, 0, or -1. You add them up, and the total tells you how likely it is the drug caused the reaction.
- Score of 9 or higher = Definite ADR. The timing fits, the reaction improved when the drug was stopped, and there’s no better explanation.
- Score of 5 to 8 = Probable ADR. The evidence is strong, but maybe you couldn’t rechallenge the patient (which we’ll get to), or there’s a small chance something else was involved.
- Score of 1 to 4 = Possible ADR. The drug could be the culprit, but other factors like an infection or another medication make it unclear.
- Score of 0 or lower = Doubtful ADR. The reaction likely came from something else-maybe the disease itself, a different drug, or even coincidence.
Each question targets a different kind of evidence. For example:
- Question 2: Did the reaction happen after the drug was given? (+2 if yes, -1 if it happened before)
- Question 3: Did the reaction get better when the drug was stopped? (+1 if yes)
- Question 5: Could something else have caused it? (-1 if yes, +2 if no)
- Question 4: Did the reaction come back when the drug was given again? (+2 if yes, -1 if it got worse)
Some of these are straightforward. Others? Not so much.
Why the Naranjo Scale Still Matters Today
Even in 2026, with AI and machine learning tools popping up everywhere, the Naranjo Scale is still the most-used tool for ADR assessment in published case reports. A 2022 study found it was used in 78% of ADR case studies in medical journals-far more than any other method.
Why? Because it’s transparent. Every score has a reason. If you’re a pharmacist documenting a reaction for the FDA or the European Medicines Agency, you need to show your work. The Naranjo Scale gives you that paper trail.
Regulators like the FDA and EMA explicitly mention the Naranjo Scale in their guidelines. It’s not optional-it’s the baseline. If you’re reporting a serious side effect, you’re expected to use it. Even if you use a newer tool, you’ll still need to justify your conclusion using the same logic the Naranjo Scale teaches.
Where the Naranjo Scale Falls Short
It’s not perfect. In fact, it was designed in the 1980s for simple, single-drug reactions. Today, most patients take five, six, or even ten medications. That’s where the Naranjo Scale starts to struggle.
Take Question 4: Did the reaction return when the drug was restarted? In real life, you almost never do this. If a patient had a life-threatening rash or liver failure from a drug, no doctor is going to give it back to them just to see if it happens again. So you answer “don’t know.” That knocks your score down, and suddenly a definite reaction becomes probable.
Then there’s Question 6: Did the reaction improve with a placebo? That’s a red flag. Giving a placebo to someone who had a bad reaction? That’s unethical now. Most clinicians skip this question entirely or mark it “don’t know.”
And what about biologics, immunotherapies, or gene therapies? These drugs can cause reactions months after stopping. The Naranjo Scale assumes reactions happen quickly. It doesn’t account for delayed immune responses. Experts say it’s not built for modern medicine.
How Real Clinicians Use It
On Reddit’s r/Pharmacology, a 2023 thread with over 40 comments showed that 68% of pharmacists and clinical pharmacologists use the Naranjo Scale daily. But they don’t use it the way the textbook says.
One pharmacist from Massachusetts General Hospital said: “We use it to force ourselves to think systematically. Without it, we’d just say, ‘Yeah, that looks like a drug reaction,’ and move on.”
But they adapt. They skip the rechallenge question. They ignore the placebo one. They treat Question 5 (alternative causes) as the most important-because in a 78-year-old on eight meds, figuring out what else could be causing the problem is the real challenge.
Many hospitals now use digital versions. A 2023 study found that when clinicians used a Python-based calculator, they finished assessments in 4.2 minutes instead of 11.3. Errors dropped from 28% to 9%. That’s huge.
Still, the biggest barrier isn’t tech-it’s training. A 2021 study showed that doctors with less than five years of experience took 37% longer to score the scale accurately than pharmacovigilance specialists. Why? Because they don’t know the drug’s typical side effect profile. You can’t answer Question 9 (Has this reaction happened before with this drug?) if you don’t know what reactions this drug usually causes.
What’s Replacing It? Not Much.
There are alternatives. The WHO-UMC system is simpler but less precise. The Liverpool Scale handles multiple drugs better. The PADRAT is designed for kids. But none of them are used as widely.
Why? Because the Naranjo Scale is the only one with decades of validation. Thousands of studies have tested it. It’s been used in clinical trials, regulatory filings, and court cases. You can’t just replace that overnight.
Instead of replacing it, the field is layering on tools. Some hospitals now use the Naranjo Scale as a first pass, then cross-check with the ALDEN algorithm for complex cases. Others use AI tools to predict likelihoods, but still ask a human to score the Naranjo questions to stay compliant.
Even the International Council for Harmonisation (ICH) is considering updates. In 2024, they proposed replacing the placebo question with one about therapeutic drug monitoring-something more realistic and ethical.
How to Learn It
You don’t need a PhD. Most people get comfortable after 3-5 practice cases. There are free resources: Fiveable has 12 interactive case studies used by over 15,000 students. The Nebraska ASAP group offers a downloadable worksheet. GitHub has open-source calculators.
Start with one real case. Pick a patient who had a reaction. Ask the 10 questions. Don’t guess. Look at the chart. When did the drug start? When did the reaction appear? Was it stopped? Did it improve? What else could explain it?
After five tries, you’ll start seeing patterns. You’ll notice that certain drugs almost always cause certain reactions. You’ll learn that a rash after starting a new antibiotic is almost always probable. A sudden drop in blood pressure after a new beta-blocker? That’s often definite.
It’s not about memorizing scores. It’s about thinking like a detective.
Final Thought: A Tool, Not a Rule
The Naranjo Scale doesn’t tell you what happened. It tells you how likely the drug caused it. That’s different. A score of 7 means “probable,” but maybe you have other evidence-a lab test, a biopsy, a known drug interaction-that makes it certain. Don’t let the score override your clinical judgment.
It’s a tool to reduce bias, not replace it. Used right, it helps you catch dangerous reactions you might have missed. Used wrong, it gives you false confidence.
It’s not the future of pharmacovigilance. But for now, it’s still the foundation. And if you work with drugs and patients, you need to know how to use it.
Is the Naranjo Scale still used in 2026?
Yes. As of 2026, the Naranjo Scale is still the most widely used tool for causality assessment in adverse drug reactions, especially in hospitals, regulatory agencies, and clinical research. It’s referenced in FDA and EMA guidelines and used in over 75% of published ADR case reports.
Can the Naranjo Scale be used for multiple drugs?
Not well. The scale was designed for one drug at a time. In patients taking five or more medications-which is common in older adults-it’s hard to pinpoint which one caused the reaction. Tools like the Liverpool ADR Probability Scale were created to handle multiple drugs, but they’re not as widely adopted.
Why is rechallenge rarely done in practice?
Rechallenge means giving the drug again to see if the reaction returns. It’s risky. If a patient had a severe reaction like anaphylaxis, liver failure, or Stevens-Johnson syndrome, re-administering the drug is unethical and dangerous. Most clinicians mark this question as “don’t know,” which lowers the score but keeps the patient safe.
Is the placebo question in the Naranjo Scale still relevant?
No, and it’s being phased out. Asking whether a placebo improved the reaction is considered unethical today. You can’t deliberately give a placebo to someone who had a serious side effect just to test it. Most professionals skip this question or mark it “don’t know.” Proposed updates to the scale aim to replace it with questions about drug level monitoring.
Do I need special training to use the Naranjo Scale?
You don’t need formal certification, but you do need clinical knowledge. Understanding how drugs work, their common side effects, and how diseases mimic drug reactions is crucial. Most people get comfortable after 3-5 cases. Free training tools from Fiveable and Nebraska ASAP can help you practice without formal classes.
Can AI replace the Naranjo Scale?
Not yet. AI tools can speed up scoring and flag potential reactions, but they still rely on the same data the Naranjo Scale uses. The scale’s strength is its transparency-every decision point is visible. AI models are black boxes. Regulators still require structured, human-interpretable assessments, so the Naranjo Scale remains the gold standard for documentation.
Is the Naranjo Scale used outside of hospitals?
Rarely. Over 87% of its use is in institutional settings-hospitals, pharmaceutical companies, and regulatory agencies with pharmacovigilance teams. Individual doctors or community pharmacists rarely use it unless they’re part of a reporting system. It’s not meant for quick clinical decisions-it’s for formal documentation and analysis.
Next Steps: What to Do If You Suspect an ADR
If you’re a clinician and think a drug caused a reaction:
- Stop the drug if it’s safe to do so.
- Document the reaction: timing, symptoms, severity.
- Review all medications-new and old.
- Run through the 10 Naranjo questions. Be honest. Don’t guess.
- Use a digital calculator if available to avoid scoring errors.
- Report it to your institution’s pharmacovigilance team or national database (like FAERS in the U.S.).
Don’t wait for the perfect tool. Use what’s proven. The Naranjo Scale isn’t flashy, but it’s reliable. And in drug safety, reliability beats innovation every time.


9 Comments
Katie Schoen
January 6 2026Honestly? I use the Naranjo scale every day but skip Q4 and Q6 without a second thought. It's not about the score-it's about forcing myself to slow down and not blame the drug just because it was new. The checklist saves lives, even if it's outdated.
Also, why is everyone still pretending rechallenge is a thing? That's how people die.
Matt Beck
January 7 2026I love this tool 😍 But let’s be real-it’s like using a rotary phone in 2026 📞😂 The placebo question? Bro, that’s not just outdated-it’s unethical. And yet we still check ‘don’t know’ like it’s a ritual. We need to update this before someone gets sued because a score was wrong due to a question that shouldn’t exist.
Mukesh Pareek
January 9 2026The Naranjo Scale’s structural limitations are statistically significant when applied to polypharmacy cohorts. The algorithmic assumption of monotherapy causality introduces Type II error bias in geriatric populations, where polypharmacy confounders exceed the scale’s discriminative capacity. Alternative frameworks like Liverpool ADR Probability Scale demonstrate superior sensitivity in multi-drug contexts.
Jeane Hendrix
January 10 2026I get why people hate the placebo question... but honestly, I just mark it 'don't know' and move on. The real issue is Question 5-figuring out what else could be causing it when someone’s on 8 meds. That’s the only one that actually makes you think. The rest is just checkbox gymnastics.
Kelly Beck
January 12 2026You guys are overthinking this 😊 The Naranjo Scale isn’t perfect, but it’s the only thing that keeps us from jumping to conclusions. I started using it after a patient had a weird rash-I thought it was the antibiotic, but turns out it was the new thyroid med. Without the checklist, I would’ve blamed the wrong drug.
Don’t throw it out-just adapt it. Skip the scary questions, use the digital tool, and trust your gut. You’ve got this!
Melanie Clark
January 12 2026Ive been in pharma for 20 years and i can tell you the Naranjo scale is a joke. The FDA uses it because its easy to audit not because its accurate. Most of the time its used to cover someones back not to help patients. And dont get me started on the rechallenge question-its not just unethical its illegal in 12 states. They keep it because its in the manual and no one wants to change the manual. This whole system is a bureaucratic ghost. The real solution? AI. But theyll never let it happen because humans like control even when its wrong
Tiffany Adjei - Opong
January 13 2026Wait, so we’re still using a 1981 tool because it’s ‘proven’? That’s like using a typewriter because ‘it’s never failed’. The placebo question is a relic. Rechallenge is a death sentence. And we’re pretending this works for patients on 12 meds? The scale doesn’t just fall short-it’s actively misleading. If you score it and don’t question its flaws, you’re not a clinician. You’re a bureaucrat.
Tom Swinton
January 14 2026I just want to say thank you to everyone who keeps using this tool even when it’s frustrating. I’ve seen nurses cry because they spent 20 minutes filling this out for a patient who didn’t even survive to see the report. But they did it anyway-because they knew someone, someday, might read it and catch a pattern.
Yeah, it’s clunky. Yeah, it’s outdated. But it’s the only thing that makes us slow down and ask: ‘What if I’m wrong?’ And that… that matters more than any algorithm. Keep going. We need you.
Lily Lilyy
January 15 2026I am so proud of how we use this tool. Even with all its flaws, we still try. We still care. We still write it down. That is what makes us good. Do not give up on the Naranjo Scale. Just make it better. One question at a time.