Omeprazole and Diabetes: Essential Facts for Patients
Omeprazole Blood Sugar Impact Estimator
Estimate Omeprazole's Effect on Your Blood Sugar
This tool helps estimate potential changes to your blood sugar control based on research data. It is not a medical recommendation.
Key Points You Can Use Today
- Omeprazole lowers stomach acid but may affect blood‑sugar control in some people.
- Both Type 1 and Type 2 diabetes patients should watch for changes when starting a PPI.
- Genetic variations in the enzyme CYP2C19 can make the drug act stronger or weaker.
- Regular monitoring of HbA1c and daily glucose readings helps catch problems early.
- Talk to your prescriber before stopping or switching any medication.
When you see Omeprazole is a proton‑pump inhibitor (PPI) that reduces stomach acid production by blocking the H+/K+ ATPase enzyme in the gastric parietal cell, it’s easy to think of it only as a heartburn fix. Yet a growing number of clinicians notice a puzzling link between this acid‑suppressing drug and changes in blood‑sugar levels, especially in people living with diabetes. This article unpacks the science, reviews real‑world studies, and gives practical advice you can act on right away. Omeprazole and diabetes are often talked about together because of this potential overlap.
What Is Omeprazole, Exactly?
Omeprazole belongs to the class Proton Pump Inhibitors (PPIs), a group of medications that shut down the final step in gastric acid secretion. By inhibiting the H+/K+ ATPase pump, they raise the pH of the stomach, providing relief from gastroesophageal reflux disease (GERD), peptic ulcers, and Zollinger‑Ellison syndrome. The drug is taken once daily, usually before breakfast, and reaches its peak effect within two hours. Because it works systemically, small amounts circulate throughout the body, which is why researchers started looking beyond the gut for side effects.
How Does Diabetes Fit Into the Picture?
Diabetes is a chronic metabolic disorder characterized by high blood‑glucose levels due to insufficient insulin secretion, impaired insulin action, or both. The two most common forms are Type 1, an autoimmune attack on pancreatic beta cells, and Type 2, where cells become resistant to insulin’s signal. Managing diabetes means keeping the HbA1c (average blood glucose over three months) within target range, typically below 7% for most adults. Any medication that interferes with glucose metabolism can make that goal harder to reach.
Why Might a Stomach Acid Pill Touch Blood Sugar?
The link isn’t obvious at first glance, but several biological pathways provide plausible explanations. First, altering Gastric Acid Secretion changes the gut’s microbiome composition. A less acidic environment can favor bacteria that influence carbohydrate digestion and insulin sensitivity. Second, PPIs like Om omeprazole can affect the enzyme CYP2C19, which metabolizes not only the drug itself but also certain antidiabetic agents such as Metformin. Genetic differences in CYP2C19 activity mean some people process the drug slowly, leading to higher systemic exposure and a greater chance of off‑target effects on glucose handling. Finally, chronic PPI use has been associated with reduced magnesium levels, and low magnesium can impair insulin signaling.
What the Research Says
Several observational studies and a handful of small trials have examined blood‑glucose trends in patients on PPIs. The evidence isn’t uniform, but a pattern emerges: long‑term users, especially those with existing diabetes, often show modest increases in fasting glucose and HbA1c.
| Study | Design | Sample Size (Diabetics) | Duration | Glucose Effect |
|---|---|---|---|---|
| Huang et al., 2022 | Retrospective cohort | 1,845 | 2‑3 years | +0.3 % HbA1c on average |
| Martinez‑Garcia et al., 2021 | Prospective cross‑over | 210 | 12 weeks (omeprazole vs. placebo) | No significant change |
| Kwon et al., 2020 | Case‑control | 3,210 | 5 years | Higher odds (OR 1.45) of needing insulin escalation |
| Lee et al., 2023 | Randomised pilot | 95 | 8 weeks | Trend toward lower fasting glucose in metformin‑only group |
What these numbers tell us is that the effect is usually modest and may depend on dose, duration, and individual metabolism. If you’re on a low‑dose regimen for a few weeks, the impact might be negligible. But for chronic GERD sufferers who take Omeprazole daily for years, the cumulative effect can become clinically relevant.
Who Should Pay Extra Attention?
Not everyone will notice a change, but certain groups are more vulnerable:
- People with Type 2 Diabetes already battling insulin resistance - any extra strain can push glucose higher.
- Patients who are CYP2C19 poor metabolizers (about 2‑5 % of Europeans). Their bodies clear Omeprazole slowly, leading to higher plasma levels.
- Those on multiple PPI doses or using the drug for more than a year.
- Individuals supplementing with magnesium or vitamin B12, because PPIs can interfere with absorption of these nutrients, indirectly affecting insulin action.
- Patients on Metformin or other oral hypoglycemics that share CYP pathways.
If you fall into any of these categories, proactive monitoring is a smart move.
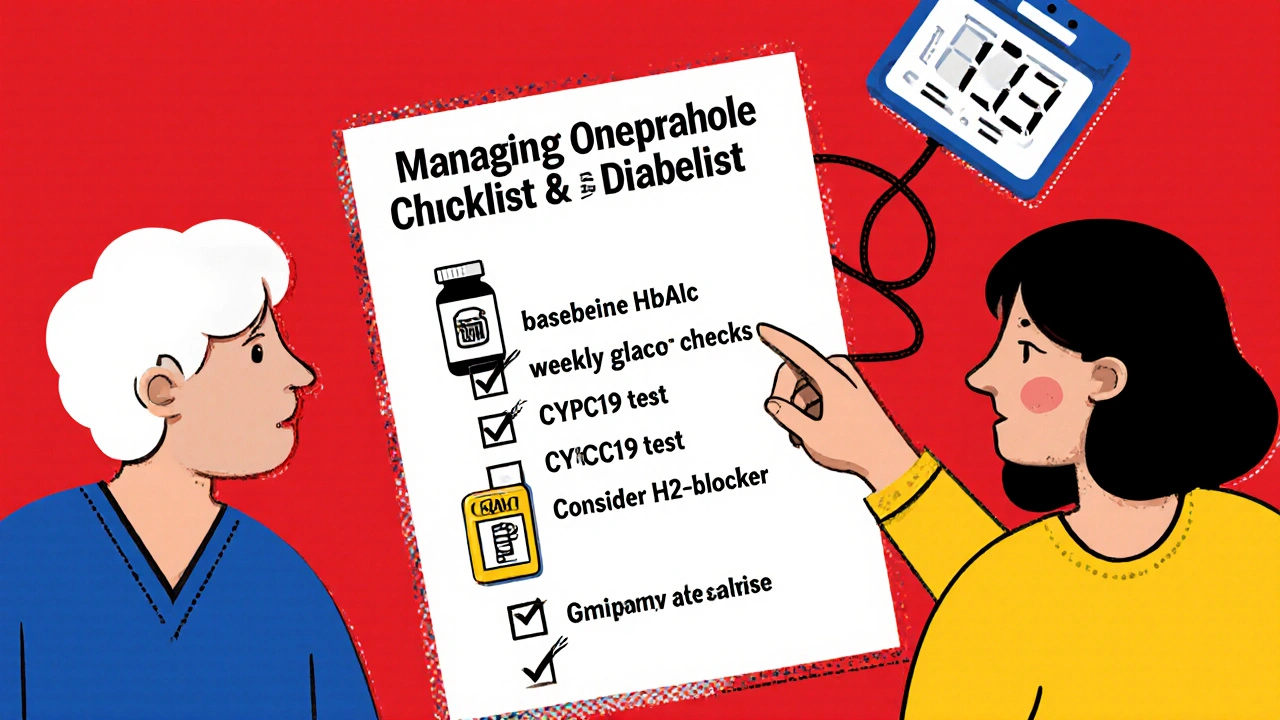
Practical Steps for Managing Both Conditions
Below is a simple checklist you can follow when your doctor prescribes Omeprazole:
- Ask whether a lower‑dose or an on‑demand regimen could work for your GERD symptoms.
- Schedule a baseline HbA1c test before starting the medication.
- Check fasting glucose weekly for the first month; note any upward trends.
- Discuss with your pharmacist whether a CYP2C19 genetic test is warranted.
- If you need long‑term acid suppression, consider alternatives such as H2‑blockers (Ranitidine, Famotidine) that have a different metabolic pathway.
- Maintain adequate magnesium intake through diet (nuts, leafy greens) or supplements if advised.
Remember, never stop Omeprazole abruptly without medical guidance; sudden rebound acid secretion can be uncomfortable and potentially harmful.
Frequently Asked Questions
Can Omeprazole cause diabetes?
No, the drug does not cause diabetes. It may modestly raise blood‑glucose levels in people who already have the disease, especially with long‑term use.
Do all PPIs affect blood sugar the same way?
Evidence is strongest for Omeprazole and Esomeprazole, but other PPIs share the same enzyme target, so a similar, though not identical, risk exists.
Should I get a genetic test for CYP2C19?
If you have a history of unusual drug reactions or belong to an ethnic group with higher poor‑metabolizer rates, a test can help your doctor choose the right dose or alternative.
Is switching to an H2‑blocker safer for my diabetes?
H2‑blockers act earlier in the acid‑production chain and are not linked to glucose changes, making them a reasonable alternative for many patients.
How often should I monitor my blood sugar after starting Omeprazole?
Check fasting glucose at least twice a week for the first month, then align with your routine diabetes monitoring schedule. Alert your clinician if values rise more than 10 mg/dL above baseline.
Wrapping Up
Omeprazole is a safe and effective tool for managing acid‑related disorders, but like any medication it can interact with other body systems. For people living with diabetes, the key is awareness and regular monitoring. By understanding the mechanisms, keeping an eye on laboratory values, and having an open conversation with your healthcare team, you can enjoy the benefits of heartburn relief without compromising glucose control.


18 Comments
Shan Reddy
October 21 2025I've found that keeping a simple log of fasting glucose before and after starting omeprazole really helps spot any subtle shifts early on.
Even a small upward trend can be caught before it affects your HbA1c.
CASEY PERRY
October 24 2025The CYP2C19 polymorphic influence on omeprazole pharmacokinetics warrants further pharmacogenomic stratification.
Naomi Shimberg
October 26 2025Although the article emphasizes vigilance, it overlooks the substantial body of population‑level data where proton‑pump inhibitors have not been linked to clinically significant hyperglycaemia, suggesting that the alleged association may be overstated.
kenny lastimosa
October 28 2025One might consider that the pursuit of perfect glycaemic control is itself a balance between therapeutic necessity and the body's adaptive capacity, and that an occasional PPI may simply be a minor perturbation in a complex system.
Heather ehlschide
October 30 2025Omeprazole is undeniably effective for acid‑related disorders, but its systemic exposure means it can interact with metabolic pathways in ways that are often underappreciated.
First, the drug’s inhibition of the H+⁄K+ ATPase reduces gastric acidity, which can subtly remodel the gut microbiome, a factor increasingly recognized as a modulator of insulin sensitivity.
Changes in microbial composition have been shown to affect short‑chain fatty acid production, and those metabolites can either enhance or blunt peripheral glucose uptake.
Second, the CYP2C19 enzyme, responsible for metabolising omeprazole, also processes several oral hypoglycaemic agents, most notably certain formulations of metformin.
Patients who are poor metabolizers of CYP2C19 may accrue higher plasma concentrations of both omeprazole and co‑administered drugs, potentially leading to an additive effect on glucose homeostasis.
Moreover, chronic suppression of gastric acid can impair the absorption of magnesium and vitamin B12, nutrients that are essential cofactors in insulin signalling cascades.
Hypomagnesemia, in particular, has been correlated with reduced insulin receptor autophosphorylation, a mechanism that can precipitate modest rises in fasting glucose.
The observational studies cited in the article, such as Huang et al. (2022) and Kwon et al. (2020), consistently report a mean HbA1c increase of around 0.3 % among long‑term users, a figure that, while numerically small, may be clinically relevant for patients already near their target.
That said, the prospective cross‑over trial by Martinez‑Garcia et al. (2021) failed to demonstrate a statistically significant change, underscoring the heterogeneity of patient responses.
Individual risk factors-such as baseline insulin resistance, duration of PPI therapy, dosage, and genetic makeup-appear to modulate the magnitude of the effect.
For clinicians, this means that a one‑size‑fits‑all recommendation is insufficient; instead, a personalized monitoring plan should be instituted when initiating omeprazole in diabetic patients.
A practical approach includes obtaining a baseline HbA1c, scheduling weekly fasting glucose checks for the first month, and reassessing the need for continued acid suppression thereafter.
If persistent upward trends emerge, consider switching to an H2‑blocker, which operates via a different metabolic route and has not been associated with glycaemic disturbances.
Additionally, patients should be counseled on maintaining adequate dietary magnesium, either through leafy greens, nuts, or supplementation if laboratory values indicate deficiency.
Finally, in an era of precision medicine, discussing a CYP2C19 genotype test with patients who have a family history of unusual drug reactions can inform dosing decisions and potentially avert adverse metabolic outcomes.
In summary, while omeprazole remains a cornerstone therapy for GERD, awareness of its nuanced interplay with glucose regulation empowers both patients and providers to optimise treatment without compromising glycaemic goals.
Kajal Gupta
November 2 2025Hey folks, just a heads‑up that if you’re popping omeprazole for a while, sprinkle some magnesium‑rich snacks into your meals – it’s a cheap hack that can keep your sugar levels steadier.
Zachary Blackwell
November 4 2025Don't be fooled by the pharma press releases; they purposely downplay the metabolic side‑effects of PPIs to keep you glued to their branded meds while the hidden labs study the long‑term glucose spikes in silence.
prithi mallick
November 6 2025i totally get that reading all this can be overwhelming, but remember u r not alone – many have walked this path and found that a simple daily log + a chat with ur doc makes a world of differecne.
Michaela Dixon
November 9 2025So basically when you take omeprazole you’re not just calming your stomach you’re also sending ripples through your gut flora which in turn can whisper to your pancreas about when to release insulin and sometimes those whispers get a little loud especially if you’ve been on the drug for months and your body is trying to adapt and you might see those numbers creep up on your meter without any obvious reason
Dan Danuts
November 11 2025Great rundown! If you’re on omeprazole, set a reminder on your phone to check your glucose on Mondays – consistency is key and you’ll thank yourself later.
Dante Russello
November 13 2025Excellent points, Heather; the detailed breakdown you provided really clarifies how multiple mechanisms converge, and I’d add that clinicians should also consider patient‑specific factors such as age, renal function, and concomitant medications, which can further modulate the interaction, so a holistic assessment is paramount.
James Gray
November 15 2025yeah i totally agree, and maybe toss in a quick tip – keep a spare bottle of famotidine handy, it’s less likely to mess with your sugar levels, just sayin.
Scott Ring
November 18 2025From a cultural perspective, many communities rely on herbal antacids, which might offer a gentler alternative without the same pharmacogenomic concerns.
Shubhi Sahni
November 20 2025When counseling patients, it’s helpful to frame the monitoring plan as a partnership: "We'll track your numbers together and adjust the regimen as needed," which often improves adherence.
Danielle St. Marie
November 22 2025The over‑hyped fear of PPIs is just noise. 😒
keerthi yeligay
November 25 2025Check your mg levels; low magnesium can nudge glucose up.
Peter Richmond
November 27 2025In clinical practice, a risk‑benefit analysis should guide the decision to continue long‑term omeprazole therapy in diabetic patients.
Bonnie Lin
November 29 2025Stay aware and keep monitoring.