Questions to Ask About Your Prescription Label at the Pharmacy
Every year, over 1.3 million medication errors happen in the U.S. - and nearly one in five of them come from people simply not understanding their prescription label. You pick up your pill bottle, glance at the tiny print, and assume you got it right. But what if you missed something critical? What if the label says to take it with food, but you’ve been taking it on an empty stomach? What if the storage instructions say refrigerate, but you left it on the counter for weeks? These aren’t rare mistakes. They’re common - and they’re preventable.
The prescription label is your most important safety tool. It’s not just a sticker with instructions. It’s a legal document approved by the FDA, packed with details that can mean the difference between healing and harm. But here’s the problem: most people never ask questions. They take what’s printed at face value. That’s risky. The average prescription label contains 25 to 35 data points - patient name, drug name, strength, dosage, refill count, expiration, storage, pharmacy contact - and none of them are optional. If you don’t verify them, you’re gambling with your health.
What’s on Your Prescription Label? The 9 Mandatory Elements
By law, every prescription label in the U.S. must include nine key pieces of information. If any of these are missing, the pharmacy is out of compliance. Don’t just assume they’re there - check.
- Patient name - Is it spelled correctly? Is it your name? A mix-up here can lead to someone else’s medication being taken - and that’s how deadly errors start.
- Prescriber name - Who ordered this? If it’s a doctor you don’t recognize, ask why.
- Drug name - Both brand and generic should be listed. If you’re used to taking Lisinopril but the label says Zestril, that’s the same drug. But if it says something completely different, stop and ask.
- Strength - Is it 5 mg, 10 mg, or 20 mg? A simple mistake here can cause overdose or underdose. Blood pressure meds, diabetes drugs, and opioids are especially dangerous if the strength is wrong.
- Dosage form - Is it a tablet, capsule, liquid, or patch? If you expected a pill but got a liquid, confirm it’s the right form.
- Quantity - How many pills are in the bottle? If you were told you’d get 30 and there are only 20, that’s a red flag.
- Directions for use - "Take one by mouth daily" sounds simple. But what does "daily" mean? Morning? Night? With food? On an empty stomach? Ask for clarification.
- Number of refills - How many times can you refill? If you need more than what’s listed, you’ll need a new prescription.
- Pharmacy contact info - Can you reach them if something’s wrong? Save the number. Call if you’re unsure.
These aren’t suggestions. They’re the bare minimum. If you don’t see all nine, ask why.
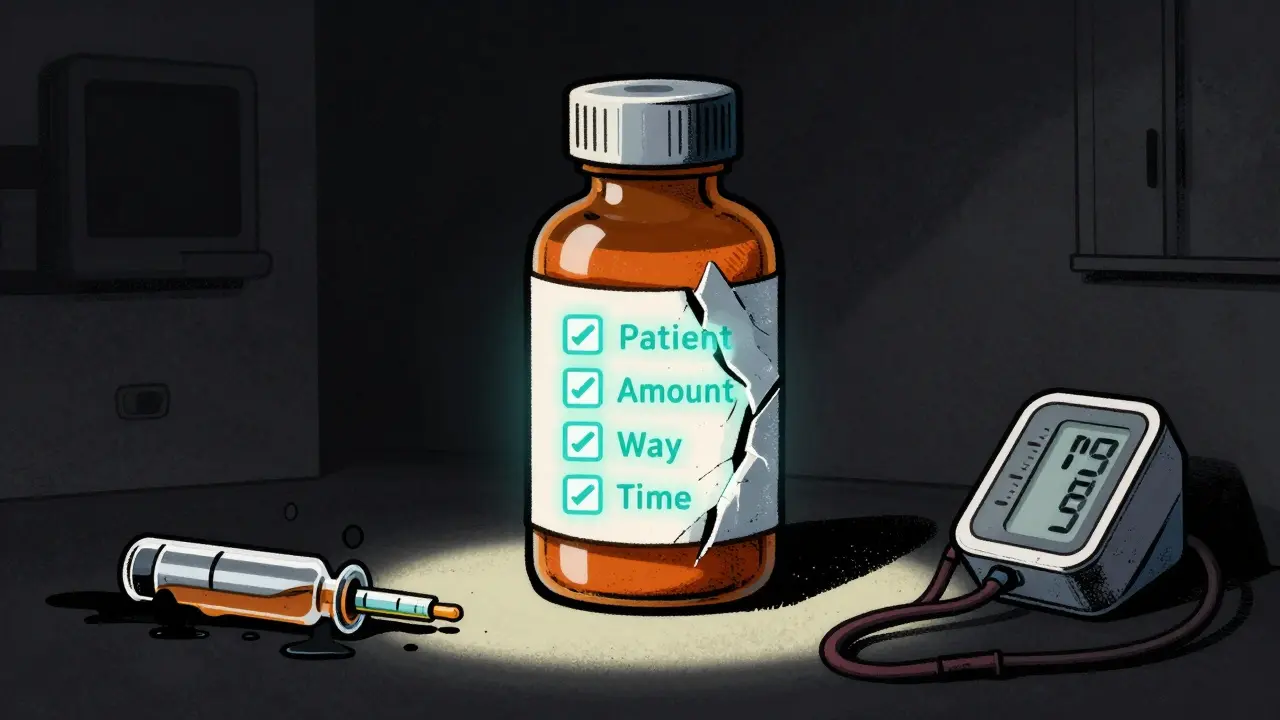
The "5 Rights" - Your Personal Safety Checklist
The Institute for Safe Medication Practices created the "5 Rights" system decades ago. It’s still the gold standard. Use it every time you pick up a prescription.
- Right Patient - Does your name match your ID? Even if the pharmacist says "it’s for Anna Smith," double-check. Names get mixed up.
- Right Medicine - Does the drug name match what your doctor told you? If you were prescribed metformin but the label says glipizide, speak up.
- Right Amount - Is the strength correct? A 5 mg tablet isn’t the same as a 50 mg tablet. Don’t guess.
- Right Way - Should you swallow it? Chew it? Apply it to your skin? Take it with water? With food? Some meds lose effectiveness if taken with dairy. Others cause nausea if taken on an empty stomach.
- Right Time - Once a day? Twice? Every 8 hours? At bedtime? If the label says "take as needed," ask what "as needed" means for you.
Repeat these out loud to the pharmacist. If they don’t encourage it, ask why. A 2022 study from the American Society of Health-System Pharmacists found that patients who used the 5 Rights reduced medication errors by 58%.
Storage: Where Your Meds Can Go Wrong
Most people think: "If it’s in the bottle, it’s fine." Not true. Medications can lose potency - or become dangerous - if stored wrong.
According to a 2022 American Pharmacists Association survey:
- 78% of prescriptions need room temperature storage (68-77°F / 20-25°C)
- 15% must be refrigerated (36-46°F / 2-8°C)
- 7% have special needs - like keeping them dry, away from light, or not freezing
Think about insulin, epinephrine auto-injectors, or certain antibiotics. If they’re left out too long, they stop working. One Reddit user reported leaving their blood pressure med at room temperature for two weeks because the storage note was printed in tiny font on the back of the label. The medication degraded. Their pressure spiked. They ended up in the ER.
Ask: "Where should I store this?" Then ask: "What happens if I don’t?" Don’t assume. Don’t guess. Confirm.

Expiration Dates and Why They Matter
The expiration date isn’t just a suggestion. It’s the last day the manufacturer guarantees the drug is fully potent and safe. After that, it doesn’t necessarily become toxic - but it might not work at all.
For example, antibiotics like amoxicillin lose effectiveness after expiration. Taking a weak dose can lead to antibiotic resistance. Insulin that’s expired can cause dangerously high blood sugar. Even common pain relievers like ibuprofen can degrade and form harmful byproducts over time.
Always check the expiration date. If it’s less than 3 months away, ask if you can get a newer batch. Some pharmacies will swap it out.
Refills: How Many? When? What If I Need More?
Some prescriptions allow refills. Others don’t. If your label says "No refills," you’ll need a new prescription from your doctor. If it says "3 refills," you can get it three more times - not four. And each refill has a time limit. Most pharmacies won’t let you refill early - even if you’re out - because of federal rules.
Ask: "How many refills are left?" Then ask: "What do I do if I run out before my next appointment?" Don’t wait until you’re out. Call ahead. If you’re on a long-term medication, ask if your doctor can set up an automatic refill program.
Language, Literacy, and Accessibility
One in three U.S. adults has trouble understanding medical instructions. That’s not a small group. That’s 80 million people. And it’s not just about education - it’s about how the label is written.
The FDA’s 2023 Draft Guidance on Patient-Friendly Labeling is pushing for clearer language, but most labels still use jargon: "q.d.", "bid," "t.i.d."
- "q.d." = once daily
- "bid" = twice daily
- "t.i.d." = three times daily
These abbreviations are outdated and dangerous. The FDA has banned them in new drug approvals, but they’re still on old labels. If you see them, ask for plain English.
Also ask: "Can I get a large-print version?" "Can I get this in Spanish?" "Can you read it to me?"
By law, pharmacies receiving federal funds must provide translation services. You don’t have to pay for it. You don’t have to ask twice. Just say: "I need this explained in my language."
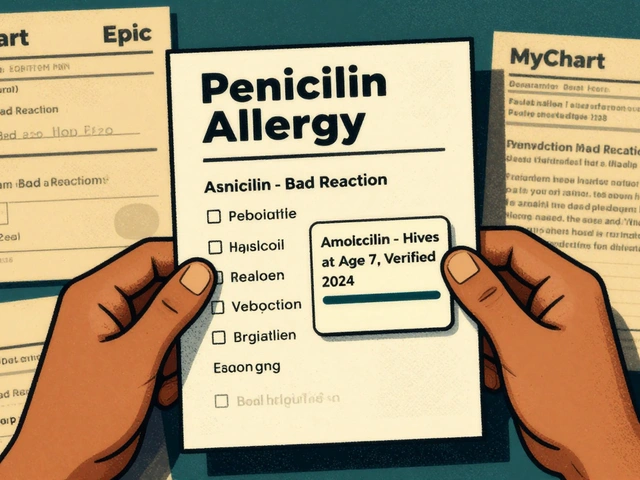
What to Do If Something Doesn’t Look Right
Here’s the truth: pharmacists aren’t perfect. Mistakes happen. A 2023 study from the University of Alabama at Birmingham found that 12% of prescriptions had at least one error on the label - from wrong dosage to missing refill info.
If anything feels off - the pill looks different, the instructions are confusing, the name doesn’t match - don’t walk away. Say: "I’m not sure about this. Can we double-check?"
Ask to speak with the pharmacist directly. Not the technician. Not the cashier. The pharmacist. They’re the ones trained to catch errors.
And if they brush you off? Go to another pharmacy. Or call your doctor. You have the right to ask. You have the right to be sure.
Technology Is Changing Labels - But You Still Need to Ask
Some pharmacies now use QR codes on labels. Scan it, and you get a video showing how to take the medicine. Others use AI systems that flag mismatches between the prescription and the label. Walgreens and CVS are testing augmented reality labels - point your phone at the bottle, and instructions appear on screen.
That’s great. But technology isn’t foolproof. A QR code might not work. The video might be in English when you need Spanish. The AI might miss a typo.
Even with fancy tech, the safest thing you can do is still this: read the label. Ask questions. Repeat the instructions back. Make sure you understand.
Dr. Lucinda Maine of the American Association of Colleges of Pharmacy says: "Patients who actively engage with their prescription labels reduce adverse drug events by up to 47%." That’s not a small number. That’s nearly half the dangerous mistakes you could avoid.
You’re not being difficult. You’re being smart. You’re not wasting their time. You’re saving your life.



12 Comments
Jonathan Noe
February 15 2026I used to just grab my scripts and run until my aunt nearly died from a mislabeled blood thinner. Now I read every word, call the pharmacy if something looks off, and even take a photo of the label to compare with my doctor’s notes. Seriously, if you’re not doing this, you’re playing Russian roulette with your liver and kidneys.
Pro tip: Ask for a printed copy of the FDA-approved patient info sheet - it’s way clearer than the bottle label.
andres az
February 16 2026The FDA doesn’t regulate labels - they’re just rubber-stamping what Big Pharma wants. The real issue? Pharmacies are incentivized to dispense fast, not explain clearly. That’s why you see the same 25-point label across 10 different drugs - it’s designed to confuse so you don’t ask questions.
They don’t want you to know that 70% of 'medication errors' are actually pharmacy-induced. The system is rigged.
Stephon Devereux
February 17 2026This is one of the most important public health pieces I’ve read in years. You’re absolutely right - the label isn’t just instructions, it’s a contract between you and your health.
I work in a clinic and I’ve seen patients die because they didn’t question a 10x dosage error. The 5 Rights aren’t just a checklist - they’re a survival protocol.
Pro tip: Write the instructions in your own words on your phone. If you can’t explain it simply, you don’t understand it. And if you don’t understand it, don’t take it.
Robert Petersen
February 18 2026I love this so much. My grandma used to say 'ask twice, die once' and she was right. I always ask my pharmacist to read it out loud to me - it’s way easier than squinting at tiny print.
Also, if they seem annoyed? That’s a red flag. A good pharmacist will be thrilled you’re paying attention. I’ve had them thank me for catching errors before I even left the counter.
Just do it. It takes 90 seconds. Could save your life.
Craig Staszak
February 20 2026I’ve been on 7 different meds over the last 5 years and I never thought to check the refill count until I ran out mid-trip and had to drive 3 hours to another pharmacy.
Now I write the date I’ll run out on the bottle cap with a Sharpie. And I call the pharmacy 3 days before. Simple. Free. Lifesaving.
Also - if the pill looks different? Always ask. Colors change all the time but shape and imprint don’t. Learn to read those.
alex clo
February 21 2026The legal requirement for nine mandatory elements is codified under 21 CFR Part 211. The FDA mandates this under the Federal Food, Drug, and Cosmetic Act. Noncompliance may result in civil penalties.
It is also worth noting that the Joint Commission requires verification of patient identity and medication reconciliation at point of dispensing. Failure to comply constitutes a breach of standard of care.
Alyssa Williams
February 22 2026OMG YES. I just had this happen last week - got a pill that looked totally different and didn’t say anything about taking with food. Called them and they were like 'oh sorry we swapped the bottle with someone else’s.'
They gave me a free refill and apologized. But imagine if I’d taken it? I’m so glad I checked.
PS: Ask for the big print version. They’ll give it to you. No shame.
Ernie Simsek
February 23 2026I once took a med that said 'take at bedtime' but I took it in the morning because I'm a morning person. Ended up with a 3 hour panic attack because it was a stimulant. 🤯
Now I screenshot the label, text it to my bro, and ask him 'is this gonna make me hallucinate?'
Also - if the bottle smells weird? Don't take it. That's not normal. 🤢
Joanne Tan
February 24 2026I’m so glad you wrote this. I’m diabetic and I’ve had two wrong insulin doses because the label said 10 units but the bottle had 20. I didn’t catch it because I was in a rush.
Now I always hold the bottle up to the light and count the drops. I also keep a little notebook with my meds, doses, and storage notes.
It’s not extra work - it’s just how I stay alive.
Reggie McIntyre
February 24 2026This isn’t just about pills - it’s about reclaiming your autonomy in a world that treats you like a data point. The pharmacy is not a vending machine. You’re not a transaction.
Every time you ask a question, you’re doing radical self-care. You’re saying: I matter. My body matters. My life matters.
And honestly? The more people who do this, the harder it becomes for the system to ignore us. So keep asking. Keep checking. Keep being weirdly meticulous. The world needs more of you.
Carla McKinney
February 24 2026I’ve reviewed over 200 pharmacy errors in my 12 years as a medical compliance auditor. Most patients don’t read the label because they’re lazy. Or they assume the pharmacist is doing their job.
Wrong. The average pharmacist handles 120 prescriptions an hour. They’re not going to explain every detail. It’s your responsibility.
If you don’t check, you’re not a victim - you’re negligent.
Ojus Save
February 24 2026i just read this and i feel so bad for my mom she took her blood pressure med for 3 months without knowing it needed to be refrigerated. she said the label was too small and she was tired. now she keeps it in the fridge and uses a magnifying glass. i love her.