Sulfonamide Allergies and Cross-Reactivity: What Drugs to Avoid and What’s Safe
Sulfonamide Safety Checker
Check if Your Allergy Applies
Based on your past reaction to sulfonamide drugs, determine if you can safely use non-antimicrobial sulfonamides.
More than 1 in 10 people say they’re allergic to sulfa drugs. But here’s the truth: sulfonamide allergy is often mislabeled. Most of the time, it’s not a real allergy at all. It’s a rash that showed up days after taking an antibiotic, or a headache, or nausea - side effects that got tagged as an allergy and stuck in the medical record. And that mistake is costing people better care, more side effects, and even contributing to antibiotic resistance.
What Actually Causes a True Sulfonamide Allergy?
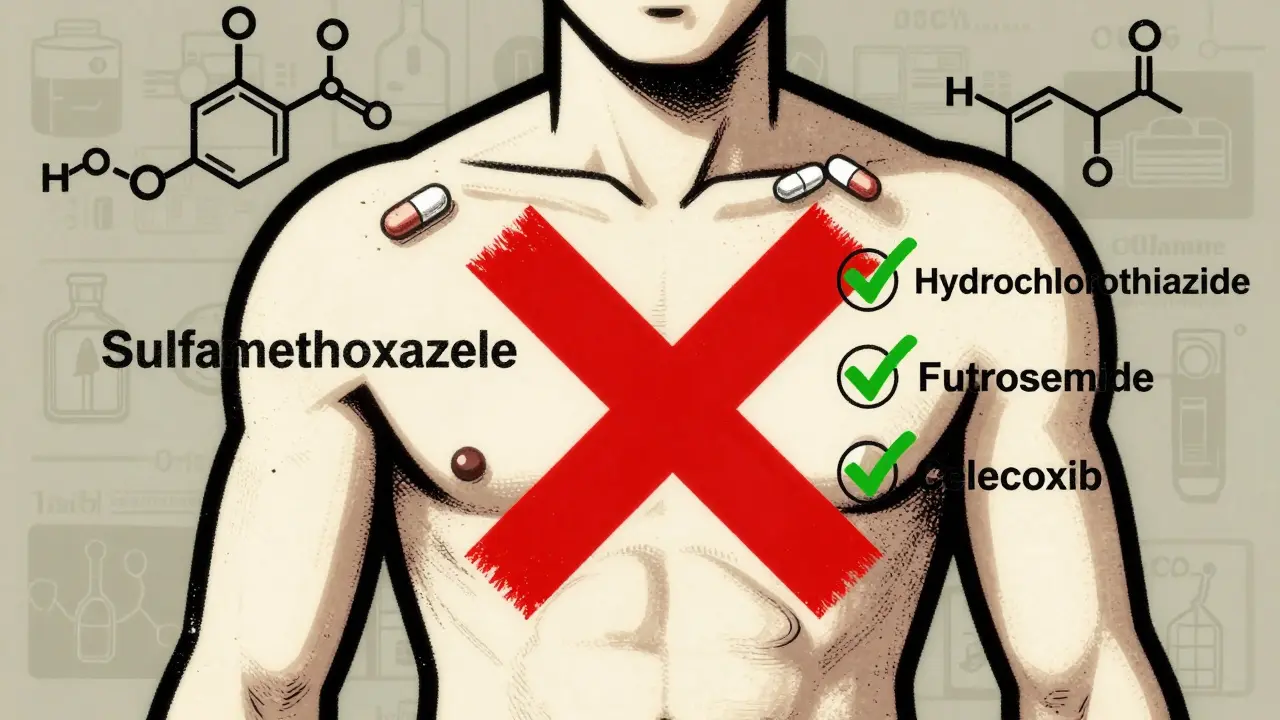
Not all sulfonamide drugs are the same. The ones that trigger real allergic reactions - like rashes, blistering, or anaphylaxis - are the antimicrobial ones. These include sulfamethoxazole (often paired with trimethoprim as Bactrim), sulfadiazine, and sulfacetamide. These drugs have a specific chemical structure: an arylamine group attached at the N4 position and a ring structure at N1. That’s what your immune system reacts to. When your body breaks these drugs down, it creates reactive molecules that bind to proteins and trick your immune system into thinking they’re invaders.
But here’s what most people don’t know: nonantimicrobial sulfonamides don’t have that same structure. Drugs like hydrochlorothiazide (for high blood pressure), furosemide (a water pill), acetazolamide (for glaucoma), and celecoxib (Celebrex) are chemically different. They lack the arylamine group. That means they don’t form the same reactive metabolites. Your immune system doesn’t see them the same way.
Do You Need to Avoid All Sulfonamides?
No. And this is where things get dangerous.
Patients with a documented sulfonamide antibiotic allergy are often told to avoid every drug with “sulfonamide” in the name. That’s wrong. A 2022 review of over 10,000 patients found that the chance of reacting to a nonantimicrobial sulfonamide - like hydrochlorothiazide - is only about 1.1%. That’s almost identical to people with no history of sulfa allergy at all (0.9%). The odds ratio? 1.23. Not even close to significant.
Yet, doctors still avoid prescribing these drugs. Why? Because the label says “sulfa allergy,” and no one wants to take the risk. But that risk is imaginary. In reality, patients with these labels are 2.4 times more likely to get fluoroquinolones like ciprofloxacin or levofloxacin instead. Those drugs carry black box warnings for tendon rupture, nerve damage, and even aortic aneurysms. You’re trading a low-risk, well-tolerated drug for a high-risk one - all because of a mislabeled allergy.
What About Celecoxib, Furosemide, or Acetazolamide?
These are safe for most people with a history of sulfonamide antibiotic allergy. Multiple studies confirm this. One large 2021 study in JAMA Internal Medicine followed more than 10,000 people with a “sulfa allergy” label. Of those, only 1.3% had any reaction to a nonantimicrobial sulfonamide. The control group? 1.1%. No difference.
Even patients who had a mild rash from sulfamethoxazole years ago can usually take hydrochlorothiazide without issue. A 2022 case series at a major allergy clinic gave 47 patients with “sulfa allergy” a graded oral challenge with sulfonamide antibiotics for pneumonia prevention. Ninety-one and a half percent tolerated it perfectly.
One patient, a 68-year-old man with a 15-year-old rash from childhood, was denied hydrochlorothiazide for hypertension because of his “sulfa allergy.” He ended up on a different blood pressure med that gave him constant dizziness. After an allergist did a simple oral challenge, he was cleared. He switched back to hydrochlorothiazide. His dizziness vanished.
The One Exception: Dapsone
There’s one nonantimicrobial sulfonamide that does carry higher risk: dapsone. It’s used to prevent Pneumocystis pneumonia in people with HIV or autoimmune conditions. Dapsone shares structural similarities with antimicrobial sulfonamides - including the arylamine group. Studies show a 13.2% reaction rate in patients with prior sulfonamide antibiotic allergy. That’s not negligible.
If you need dapsone and have a history of a severe reaction - like Stevens-Johnson syndrome or toxic epidermal necrolysis - you should be evaluated by an allergist first. But if your reaction was just a mild rash that appeared days after taking Bactrim, a supervised challenge may still be safe. Don’t assume it’s off-limits.
What About Sulfates, Sulfites, and Sulfur?
Let’s clear up the biggest confusion. Sulfonamide allergy has nothing to do with:
- Sulfates - like magnesium sulfate (used in preeclampsia) or glucosamine sulfate
- Sulfites - preservatives in wine, dried fruit, or processed foods
- Sulfur - the element found in eggs, garlic, and many supplements
These are chemically unrelated. Yet a 2020 survey found that 42.7% of primary care doctors thought patients with sulfa allergy couldn’t take sulfites. That’s a dangerous myth. You can eat wine, take glucosamine, or eat eggs - no problem.
How to Fix a Misdiagnosed Sulfa Allergy
If you’ve been told you’re allergic to sulfa drugs, here’s what to do:
- Check your records. What was the actual reaction? “Rash” isn’t enough. Was it a mild, delayed rash? Or did you have trouble breathing, swelling, or blisters within hours?
- Ask your doctor. If your reaction was mild and occurred more than 72 hours after starting the drug, you’re likely not truly allergic. Ask if you can get a supervised oral challenge with a nonantimicrobial sulfonamide like hydrochlorothiazide.
- See an allergist. If you had a severe reaction - anaphylaxis, blistering skin, fever - get tested. Skin tests and graded challenges can confirm whether you’re truly allergic. Studies show 94.7% of people labeled with sulfa allergy pass these tests.
- Update your chart. Don’t just say “sulfa allergy.” Write: “Mild maculopapular rash after sulfamethoxazole-trimethoprim, resolved after stopping. No anaphylaxis. Likely non-allergic.” This helps future doctors make better decisions.

Why This Matters Beyond Your Own Health
Every time a doctor avoids a sulfonamide antibiotic because of a mislabeled allergy, they reach for something broader - vancomycin, fluoroquinolones, or carbapenems. These drugs are more expensive, harder on the gut, and fuel antibiotic resistance.
A 2021 study found that patients with a “sulfa allergy” label received broader-spectrum antibiotics 32.7% of the time. That’s not just bad for you - it’s bad for everyone. The CDC reports that this kind of inappropriate prescribing increases resistance in E. coli by 8.3% and Staphylococcus aureus by 12.7%.
And the cost? An estimated $1.2 billion a year in the U.S. alone - extra hospital stays, more expensive drugs, longer recovery times.
What’s Changing Now?
Things are shifting. In 2023, the American Academy of Allergy, Asthma & Immunology and the Infectious Diseases Society of America launched the Sulfonamide Allergy De-labeling Initiative. Hospitals are starting to use EHR alerts that flag vague “sulfa allergy” entries and prompt doctors to clarify.
Some systems now require doctors to specify the reaction type before the alert triggers. Others use the SULF-RISK score - a validated tool that predicts true allergy risk with over 90% accuracy. And by 2025, 75% of major health systems plan to have automated protocols in place to reduce unnecessary avoidance.
Meanwhile, new blood tests are being developed. A sulfamethoxazole-specific IgE assay is in Phase II trials and shows 89.7% accuracy in identifying true allergies. This could one day replace guesswork with science.
Bottom Line: Don’t Let a Label Limit Your Care
If you’ve been told you’re allergic to sulfa drugs, you might not be. Most people aren’t. The drugs you’re being denied - hydrochlorothiazide, furosemide, acetazolamide, even celecoxib - are safe for you. Avoiding them isn’t protecting you. It’s hurting you.
Take action. Review your history. Talk to your doctor. Ask about an allergist referral. Get the facts. Your next prescription shouldn’t be chosen out of fear. It should be chosen because it’s the right one.




15 Comments
Stephen Tulloch
January 17 2026Bro this is the kind of post that makes me want to hug a doctor 🤗. So many people are walking around with "sulfa allergy" stamped on their chart like it's a tattoo from a bad decision at 2am. I had a rash from Bactrim in college - turned out it was just heat + bad laundry detergent. Took me 7 years to get my records fixed. Now I take hydrochlorothiazide like it's candy. Stop letting ghost allergies dictate your meds.
Bianca Leonhardt
January 18 2026Let me guess - you're one of those "I read one study on PubMed" types who thinks every doctor is an idiot. My grandma had Stevens-Johnson from sulfamethoxazole. She spent three weeks in the ICU. You think a "1.1% reaction rate" matters when your kid could be next? Stop reducing human suffering to statistics.
Riya Katyal
January 19 2026Ohhh so now it’s all just "misdiagnosed"? Like, your rash from Bactrim wasn’t your immune system screaming? It was just… bad vibes? 😏 Next you’ll tell me penicillin allergies are just people being dramatic because they ate too much cheese.
Melodie Lesesne
January 19 2026This is such a needed conversation. I’m a nurse and I’ve seen so many patients get stuck with terrible meds just because their chart says "sulfa allergy" without details. One lady was on vancomycin for a UTI because she was "allergic" - turns out she got a rash once at 14 and never got tested. We did a challenge, she’s now on HCTZ and feels like a new person. Small changes = huge wins.
Rob Deneke
January 19 2026Man I wish more docs knew this. I had a doc refuse to give me furosemide because I took Bactrim once 10 years ago. I ended up with swollen ankles for months. Finally went to an allergist - they gave me a tiny dose of hydrochlorothiazide in front of them and I was fine. No drama. No hospital. Just common sense. Why is this so hard
Travis Craw
January 21 2026im not a doctor but i read this whole thing and it makes sense. i had a rash from sulfa drugs too but it was like 5 days later and it was just red spots. no swelling no breathing issues. i always thought i was allergic but now i think maybe it was just my body being weird. maybe i should ask my doc about it
brooke wright
January 21 2026Wait so you're saying I can finally drink wine again? I've been terrified of it since I got that rash from Bactrim in 2012. I thought sulfites were the same thing. I’ve been ordering sparkling water at parties like some kind of sobriety poster child. This changes everything. Thank you.
Nick Cole
January 22 2026I had a cousin who died from a reaction to sulfa. It was brutal. I don’t trust these "it’s probably fine" narratives. Not everyone gets a second chance. Just because the stats say 94% are fine doesn’t mean the 6% don’t matter. I get the intent but please don’t downplay real trauma.
kanchan tiwari
January 24 2026THIS IS A PHARMA CONSPIRACY. They want you to take hydrochlorothiazide because it’s cheaper. They don’t want you to know that the real allergy is caused by glyphosate in the pills. The FDA knows. The WHO knows. But they’re silencing doctors who speak out. Your "1.1%" statistic? That’s the number of people who didn’t die. The rest? They’re in the morgue. And they’re calling it "side effects."
Bobbi-Marie Nova
January 26 2026OMG I’m crying. I’ve been avoiding celecoxib for 8 years because of a stupid rash. My knees hurt so bad I can’t play with my dog. I just called my doctor and asked for a challenge. She said yes. I’m so relieved. You just gave me my life back 🥹💖
john Mccoskey
January 26 2026The entire premise of this post is a fallacy rooted in reductionist biomedical ideology. You treat the immune system like a faulty algorithm that can be "debugged" by reclassifying chemical structures. But allergies are not merely structural - they are phenomenological. The body remembers. The soul remembers. Even if the arylamine group is absent, the trauma of the initial reaction persists in the somatic memory. To say "it’s safe" is to ignore the epistemological rupture that occurs when the body is violated by pharmaceuticals. You cannot quantify lived experience with percentages. You are not healing - you are colonizing the patient’s autonomy with data.
Samyak Shertok
January 28 2026Oh so now sulfa allergies are fake but gluten is real? Wait, no - gluten is real. But sulfa is fake? But wait - what if your body is just sensitive to sulfur? But sulfur is everywhere. So if you’re allergic to sulfur then you can’t eat eggs, garlic, or breathe air? Oh wait - you said sulfonamide ≠ sulfur. But then why do you say sulfites are unrelated? Aren’t they both sulfur-based? You’re just rearranging deck chairs on the Titanic. I’m not buying it.
Joie Cregin
January 29 2026My aunt got mislabeled with a sulfa allergy after a weird rash from a UTI med. She spent 15 years on blood pressure meds that made her feel like a zombie. Then she finally saw an allergist - got cleared for HCTZ - and suddenly she could walk without dragging her feet. She started gardening again. She’s 78 now and grows tomatoes like she’s trying to win a prize. This isn’t just medicine - it’s a second chance at joy.
evelyn wellding
January 29 2026YES YES YES!! I’ve been saying this for years!! I took Bactrim once in college and got a tiny rash - no big deal. But my doctor kept writing "sulfa allergy" and I couldn’t get the right meds for my migraines. I finally pushed back and got tested - turned out I’m fine! Now I take furosemide like a boss 💪❤️
Chelsea Harton
January 30 2026so if i had a rash from sulfa but no anaphylaxis im probably fine? just check with a doc? sounds easy. why dont more people know this