Asthma: What if your blue inhaler isn't the whole answer?
What if your blue inhaler isn't the whole answer? For many people with asthma, relief comes from mixing the right medicine, device, and daily habits. You can breathe better without relying on quick fixes alone.
Asthma is inflammation of the airways. That makes breathing tight, wheezy, and sometimes scary. Symptoms often flare with colds, pollen, smoke, exercise, or strong smells. Knowing your triggers is step one. Track attacks, note timing, and what you were around. That data helps your doctor pick better treatments.
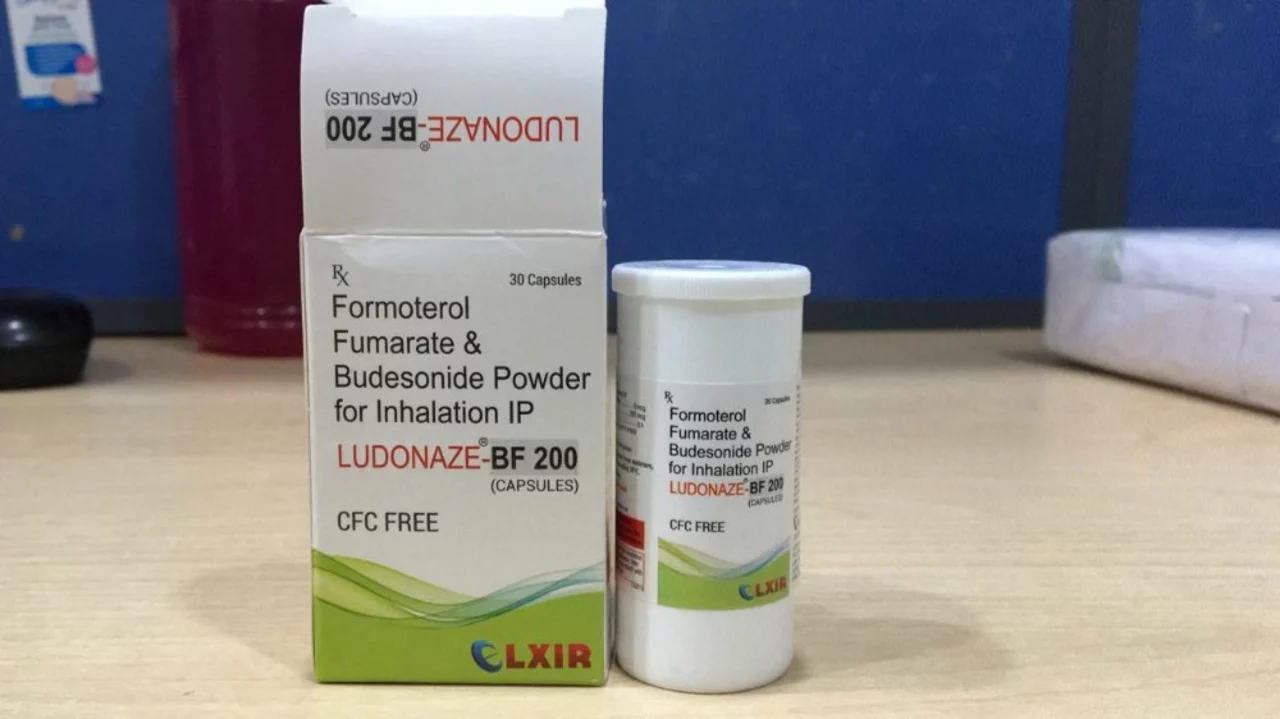
Inhaler and device choices
Short-acting inhalers like albuterol (the blue one) stop attacks fast. Long-acting inhalers reduce inflammation and cut flare-ups over time. There are other options too: dry powder inhalers, nebulizers, and new biologic shots for severe cases. Device choice matters. If you use an inhaler badly, the drug won't work well. Practice with a spacer or ask your nurse to show your technique.
Dry powder inhalers are small and portable. Nebulizers turn medicine into mist you inhale, which can help young kids or people who struggle with sprays. Biologics target the immune signals causing severe asthma. They can cut hospital visits for the right patients. Talk to your doctor about side effects, cost, and how often you need treatment.
Simple daily steps
Keep a written action plan. Know when to use your rescue inhaler and when to call for help. Take controller meds every day if prescribed. Skipping doses makes flares likelier. Wash bedding weekly if dust mites trigger you. Avoid smoking and smoky places. Exercise can help lung strength, but warm up and use your inhaler before exertion if exercise brings wheeze.
If attacks increase, or you need rescue inhaler more than twice a week, call your doctor. Adjusting therapy might stop worse problems. Emergency signs are hard to speak, fast heart rate, or blue lips. Seek urgent care if those happen.
Changes add up. Using the right device, practicing technique, and following a plan lower attacks and hospital trips. Want more detail? Read our posts on inhaler choices and alternatives to Ventolin. They break down options, pros, and how to choose. You can find those under the "asthma" tag on this site.
I know living with asthma can feel overwhelming sometimes. Start small: track symptoms, ask about devices, and follow your plan. Small wins make breathing easier over time. Explore our guides for practical tips and step- by- step help.
A peak flow meter gives numbers you can track at home. It helps spot worsening before symptoms get bad. Allergy control like HEPA filters, mold fixes, and pet plans cuts triggers. Stay up to date on flu and COVID shots; infections often spark flares. Traveling? Pack extra inhaler doses, spacer, prescriptions, and printed action steps. Airlines can accept spacers and inhalers in carry-on bags.
Kids need clear plans too. Teach them and caregivers who to call in emergency. Use cartoons or simple sheets so schools know steps. For teens, talk honestly about risks of skipping meds and vaping, which can make asthma worse.
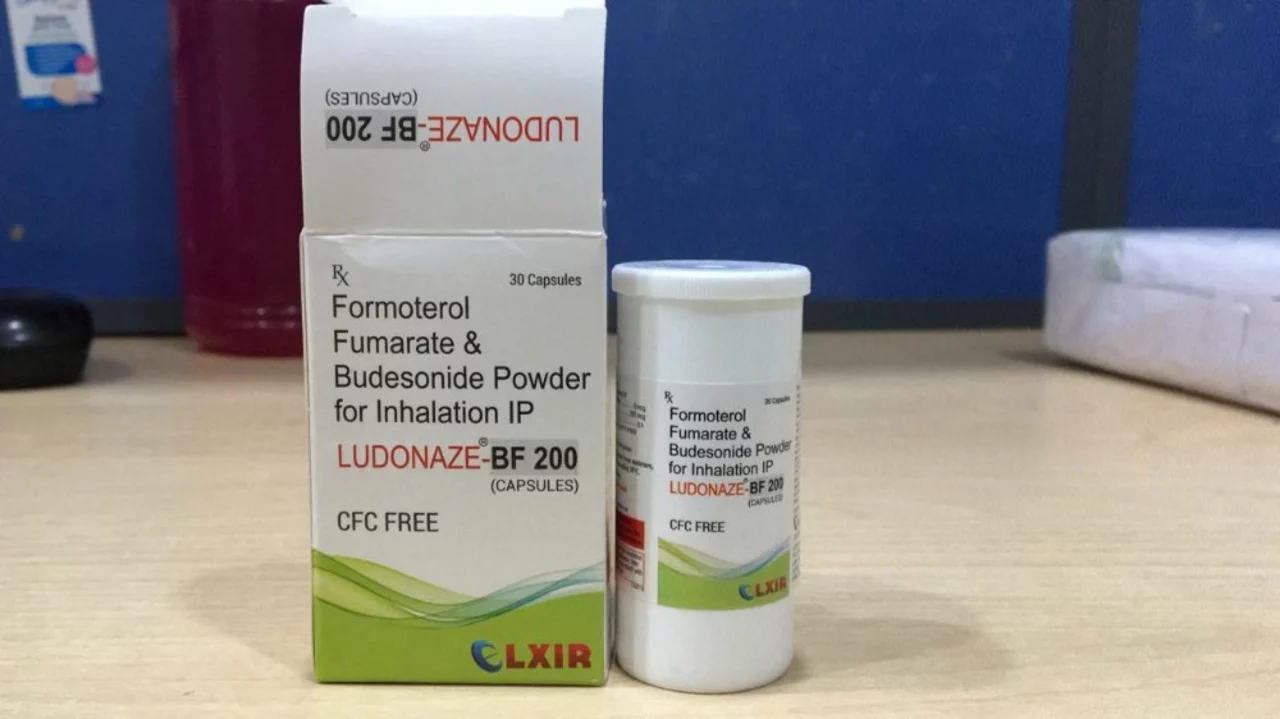
Traveling with my budesonide formoterol inhaler is easy and stress-free when I follow these simple tips. First, I always keep it in my carry-on bag to ensure it's readily accessible during my journey. Second, I carry a copy of my prescription and a doctor's note to avoid any issues at security checkpoints. Third, I make sure to pack enough medication to last the entire trip, plus some extra in case of delays. Lastly, I stay mindful of my asthma triggers and take necessary precautions to prevent flare-ups while exploring new destinations.
Continue Reading