Biosimilars: What They Are, How They Compare to Biologics, and Why They Matter
When you hear biosimilars, highly similar versions of complex biologic drugs that are not exact copies but are proven to work the same way. Also known as follow-on biologics, they are a major shift in how we treat chronic conditions like rheumatoid arthritis, cancer, and diabetes. Unlike regular generics—which are simple chemical copies of old drugs—biosimilars are made from living cells. That means they’re more like a close cousin than a twin. They can’t be identical, but they must perform just as safely and effectively as the original biologic drug, according to strict FDA and global standards.
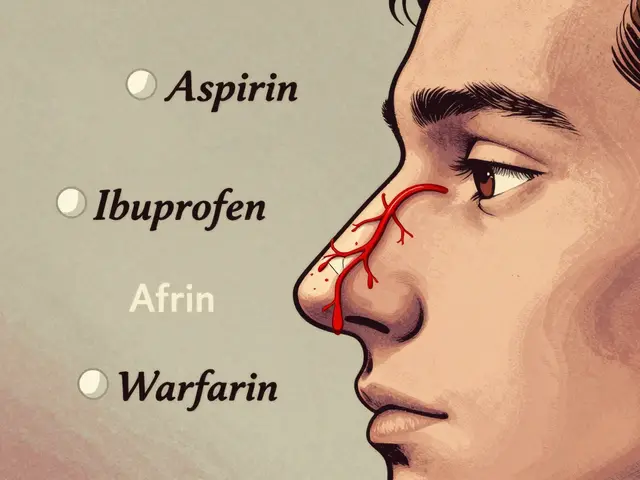
Why does this matter? Because biologics, large, complex drugs made from living organisms, often used for serious diseases can cost over $100,000 a year. A single course of Humira or Enbrel might wipe out a family’s savings. Biosimilars cut those prices by 15% to 35%, sometimes more. Insurers love them—not because they’re cheaper to make, but because they finally give patients real options without sacrificing results. But here’s the catch: biosimilars aren’t the same as generic drugs, simple, chemically identical copies of small-molecule medications. You can’t swap them like aspirin and ibuprofen. Switching from a brand-name biologic to a biosimilar needs careful planning, especially if you’re stable on your current treatment.
Some patients worry biosimilars are "second-rate." But the data doesn’t support that. The FDA requires over 100 tests before approval—checking protein structure, purity, how the body absorbs it, and even immune responses. Real-world studies from Europe and the U.S. show patients switching to biosimilars don’t see more side effects or loss of effectiveness. In fact, one 2023 study tracking over 5,000 rheumatoid arthritis patients found no difference in flare-ups between those on the original drug and those on its biosimilar. That’s not luck—it’s science.
But access isn’t always easy. Some pharmacies won’t substitute without your doctor’s OK. Insurers sometimes make you try the biosimilar first, even if you’re doing fine on the brand. And not all biosimilars are approved for every use the original drug is. That’s why knowing your exact medication name and condition matters. If you’re on a biologic for Crohn’s, for example, the biosimilar approved for rheumatoid arthritis might not be right for you.
What you’ll find below are real, practical posts that cut through the noise. You’ll learn how biosimilars fit into insurance formularies, why some doctors hesitate to prescribe them, how they compare to other cost-saving options like compounded meds, and what to do if your insurer tries to force a switch. No fluff. Just what you need to understand your options, ask the right questions, and keep your treatment on track without breaking the bank.

Specialty pharmacies handle generic specialty drugs with the same care as branded ones-due to complex administration, safety protocols, and patient support needs. Providers must understand why distribution doesn't change just because the price drops.
Continue Reading

Patent expiry means big savings on medications-but only if you're prepared. Learn how patients and healthcare systems can navigate the transition to generics and biosimilars to cut costs without risking care.
Continue Reading