Blood thinners: what they do and when you need them
Blood thinners lower the chance of dangerous clots that can cause strokes, deep vein thrombosis (DVT), or pulmonary embolism (PE). They don’t actually "thin" blood — they stop platelets or clotting proteins from making clots. That small change can prevent life‑threatening events, but it also raises bleeding risk. If you or a loved one is starting treatment, a few practical facts make a big difference.
Types of blood thinners and how they differ
There are two main groups: anticoagulants and antiplatelets. Anticoagulants (often called blood thinners) include warfarin and newer direct oral anticoagulants — apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa), and edoxaban. These target different steps in the clotting cascade. Warfarin needs regular blood tests (INR) and food/drug checks. DOACs usually don’t need routine labs and have fixed dosing, but they can still interact with other drugs.
Antiplatelets like aspirin and clopidogrel (Plavix) work differently: they stop platelets from sticking together. Doctors often use them after stents or for certain heart conditions. Sometimes people take both types after specific procedures—your doctor will weigh clot vs bleeding risks to make that call.
Practical safety tips everyone should know
Follow dosing exactly. Missing doses or doubling up can be dangerous. If you miss a dose, check the medication leaflet or call your pharmacist — advice varies by drug.
Watch for bleeding: unusual bruising, blood in urine or stool, heavy nosebleeds, coughing up blood, or prolonged bleeding from a cut. If you notice fast heartbeat, fainting, severe headache, or sudden weakness, get emergency help—these can signal serious bleeding or stroke.
Tell every healthcare provider you’re on a blood thinner before surgeries, dental work, or new prescriptions. Some procedures need temporary stopping or dose changes. For warfarin users, keep steady vitamin K intake (leafy greens) and get INR checks on schedule. For DOAC users, ask about timing around procedures and kidney function checks; some DOACs need dose changes in renal impairment.
Drug and supplement interactions matter. Common culprits: antibiotics, antifungals, certain heart meds, NSAIDs (ibuprofen, naproxen), and herbal supplements like St. John’s wort or high-dose fish oil. Alcohol can increase bleeding risk if used heavily.
Pregnancy and breastfeeding require special handling—some blood thinners are unsafe. If you travel, carry a list of your meds, a letter from your doctor, and extra pills. Keep emergency contact and local medical info handy.
Ask your clinician clear questions: Why this drug? How long will I take it? What side effects should I expect? When should I call for help? Simple, direct answers will help you use blood thinners safely and confidently.
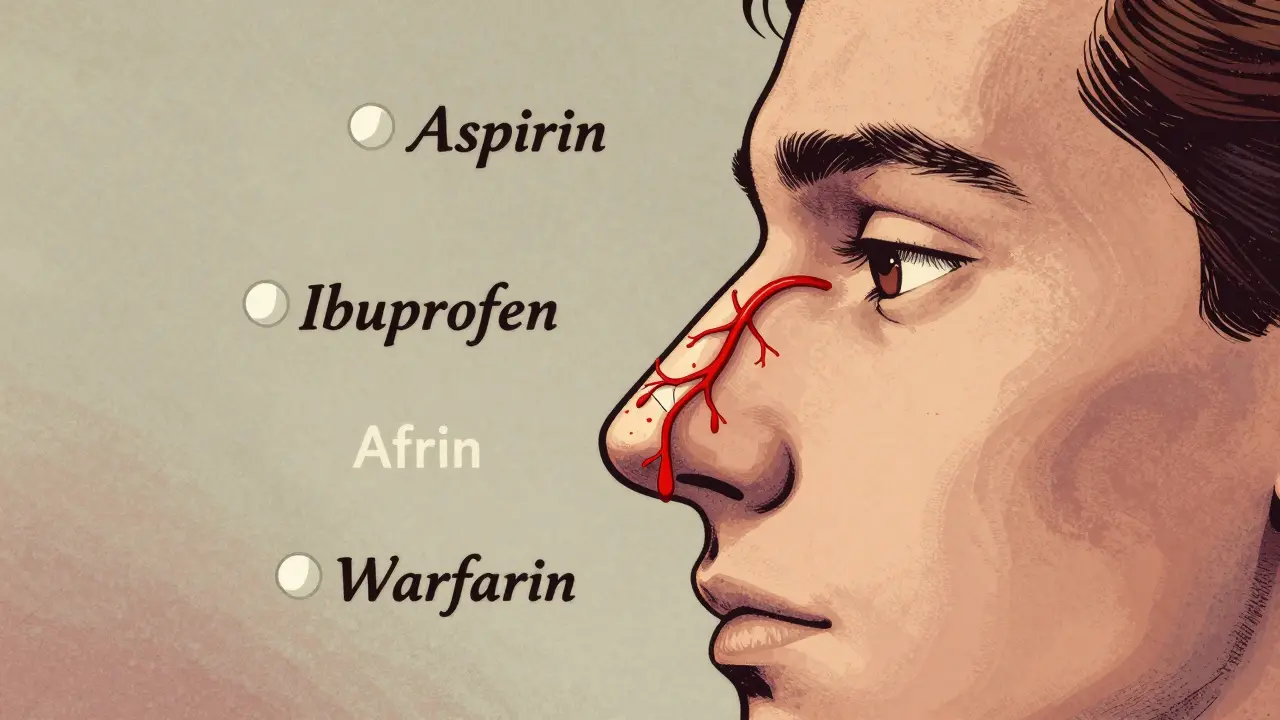
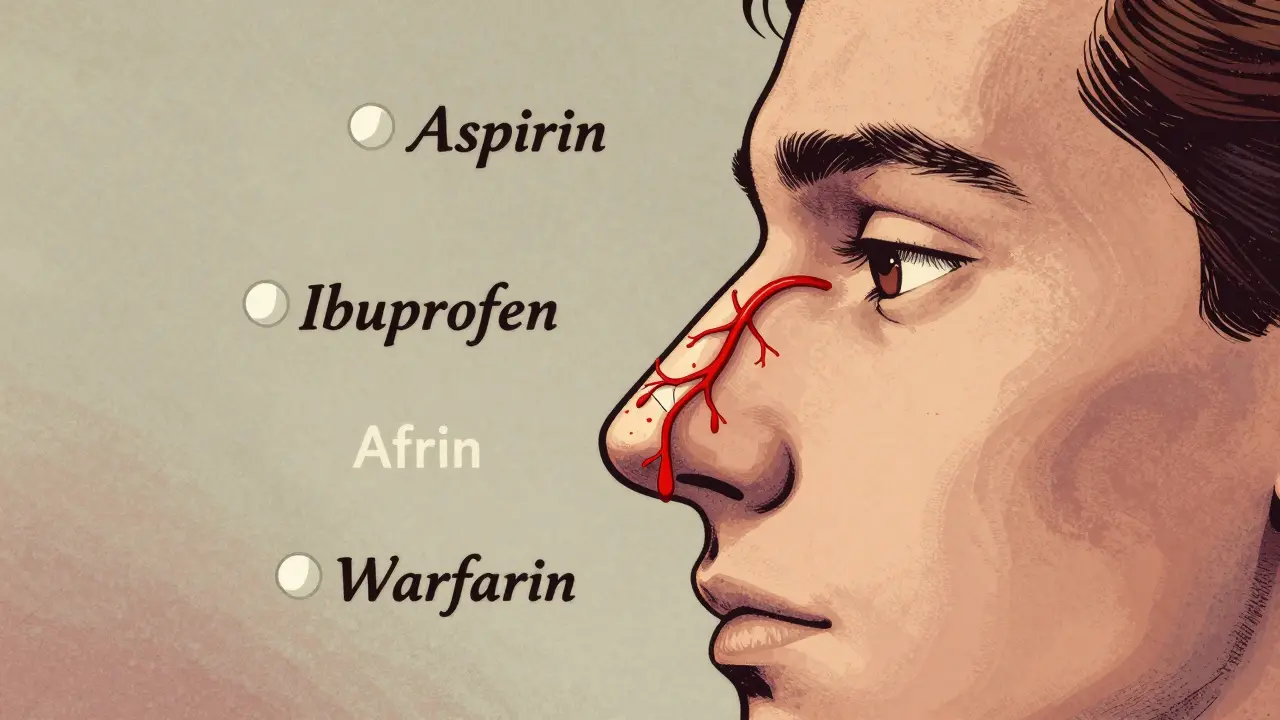
Nosebleeds can be caused by common medications like aspirin, ibuprofen, and blood thinners. Learn how these drugs affect your nasal lining and what simple steps you can take to prevent them without stopping your prescriptions.
Continue Reading

Warfarin and DOACs are both blood thinners, but DOACs are now safer and more convenient for most people. Learn how they differ in bleeding risk, kidney safety, cost, and daily use.
Continue Reading
Learn how to safely pause blood thinners before surgery without increasing the risk of clots or bleeding. Updated guidelines for DOACs, warfarin, reversal agents, and timing based on 2023-2024 evidence.
Continue Reading

Curious about the future of anticoagulation therapy and whether rivaroxaban will keep its spot among top blood thinners? This article dives deep into how rivaroxaban stacks up against newer treatments, what science is saying about its future, and what patients and doctors need to know. You'll get real-world tips, stats, and honest talk about risks and rewards—no sugarcoating, just clear facts.
Continue Reading