Brand-Name Drugs: What They Are, Why They Cost More, and How They Compare to Generics
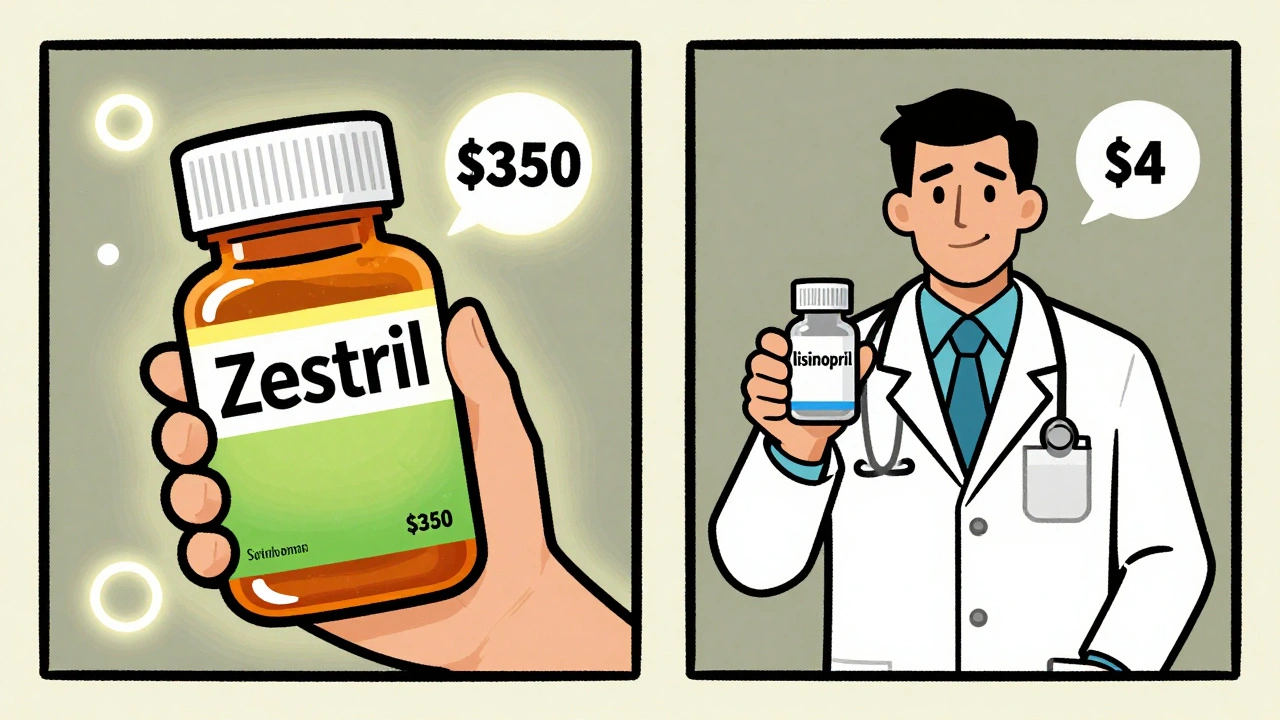
When you hear brand-name drugs, the original, patented versions of medications developed by pharmaceutical companies. Also known as originator drugs, they're the first to hit the market after years of research and clinical trials. These are the pills and injections you see advertised on TV — the ones with catchy names like Lipitor, Nexium, or Dostinex. They’re not just names on a bottle; they represent billions in R&D investment, legal protections, and marketing muscle. But here’s the thing: once the patent runs out, the same exact chemical can be sold for pennies. That’s where generic drugs, chemically identical versions of brand-name drugs made after patent expiry come in. The FDA requires them to work the same way, in the same dose, with the same safety profile. So why do brand-name drugs still cost 10 to 20 times more?
The answer isn’t quality — it’s timing and control. pharmaceutical patents, legal monopolies granted to drug makers for 20 years to recoup development costs are the engine behind high prices. During that window, companies set prices without competition. Once the patent expires, dozens of manufacturers can produce the same drug. That’s when prices crash — sometimes by 95%. But many people don’t realize that the active ingredient in their expensive brand-name pill is the same as the cheap generic next to it. Even medication alternatives, options like biosimilars or authorized generics that offer similar benefits at lower cost are often overlooked. Insurers push generics because they save money. Doctors sometimes default to brand names out of habit. Patients pay more because they assume name equals better.
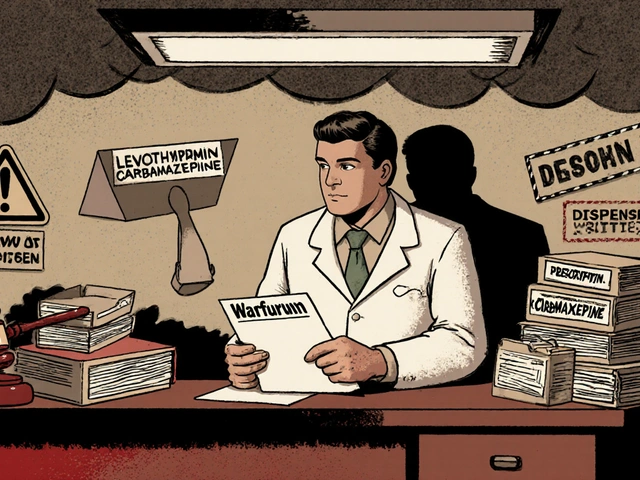
But it’s not that simple. Some drugs — like levothyroxine or warfarin — need extra care when switching, because tiny differences in inactive ingredients can affect absorption. And while most generics are perfectly safe, the FDA’s list of authorized generics is often misunderstood. You might think all generics are the same, but not all are made by the original brand. Some are made by the same factory, just sold under a different label. That’s the hidden truth behind why some people feel different on a generic. It’s not the drug — it’s the packaging, the marketing, or even the placebo effect. Understanding this helps you ask better questions. You don’t need to pay more unless there’s a real medical reason. And if your doctor says the brand is necessary, ask why — and what alternatives exist.
What you’ll find below are real, practical guides on how brand-name drugs fit into the bigger picture of cost, safety, and access. From how patent expiry affects your prescriptions, to why insurers favor generics, to when switching might actually be risky — every post here cuts through the noise. You’ll learn how to spot when you’re paying for a name instead of a medicine. And you’ll see exactly how to make smarter choices without guessing.
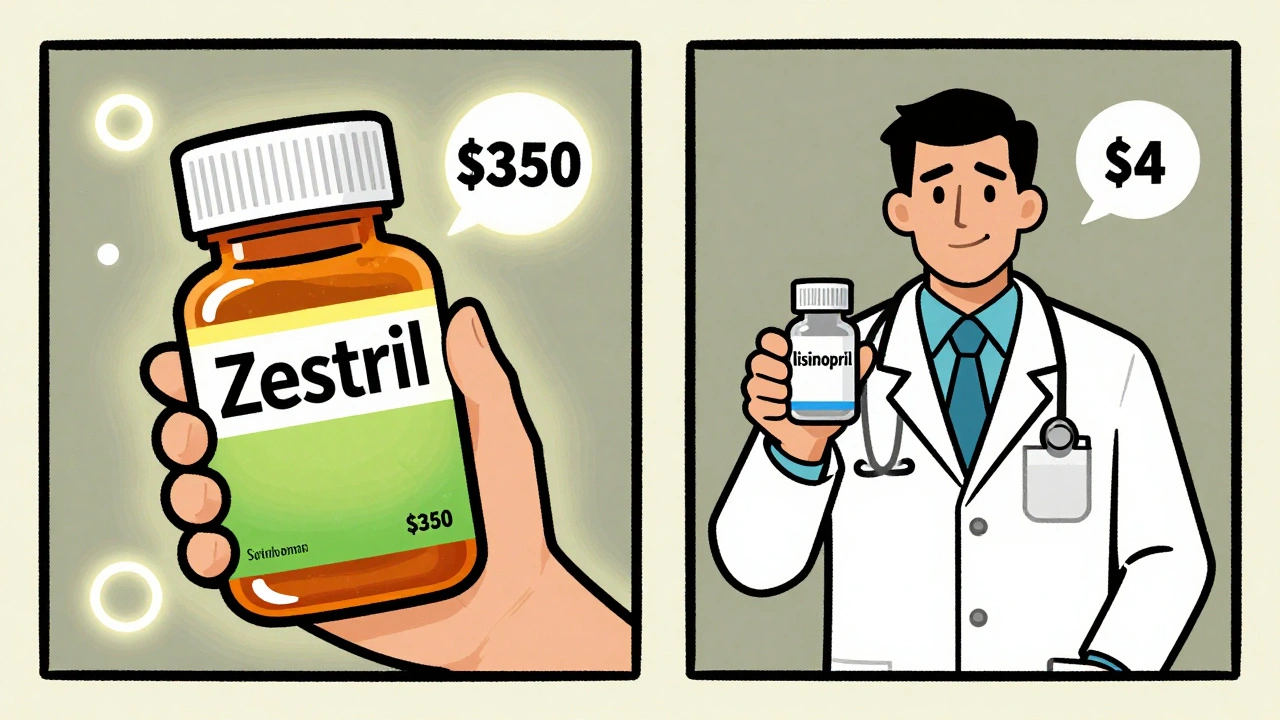
Generics work just as well as brand-name drugs - and save patients up to 90% on costs. Yet many doctors still prescribe brands, and patients refuse generics. Here’s why - and how to overcome the psychology behind the resistance.
Continue Reading