Lasix alternatives: what works and when to talk to your doctor
Lasix (furosemide) is a powerful loop diuretic used for fluid overload in heart failure, kidney disease, and severe edema. It works fast, but it can also cause bothersome side effects like low potassium, dehydration, lightheadedness, and frequent urination. If Lasix doesn't suit you or causes problems, there are several alternatives worth discussing with your clinician.
Why consider alternatives?
Maybe Lasix makes you dizzy, drops your electrolytes, or isn’t controlling swelling well anymore. Or your doctor worries about kidney function or long-term side effects. Sometimes people want fewer daily trips to the bathroom or a drug that keeps potassium steady. Whatever the reason, the choice of alternative depends on why you’re taking Lasix—edema, heart failure, or high blood pressure.
Common medication alternatives and how they differ
Thiazide diuretics (hydrochlorothiazide, chlorthalidone): These are gentler than Lasix and work well for high blood pressure and mild-to-moderate fluid retention. Chlorthalidone usually lasts longer and may control blood pressure better than hydrochlorothiazide. Watch blood sugar and electrolytes—thiazides can lower potassium and raise uric acid.
Loop alternatives (bumetanide, torsemide): If you need a loop diuretic but Lasix causes side effects or doesn’t work well, bumetanide and torsemide are options. They often have better absorption and more predictable effects. Torsemide may last longer, meaning fewer doses for some patients.
Potassium-sparing diuretics (spironolactone, eplerenone, amiloride): These are useful when low potassium is a problem or as add-ons to reduce potassium loss. Spironolactone also helps in certain heart failure patients. Be careful if you have kidney disease—these drugs can raise potassium too much.
Non-diuretic medicines: For fluid control related to heart failure or blood pressure, ACE inhibitors, ARBs, and newer drugs like SGLT2 inhibitors can reduce hospitalizations and help with symptoms. They’re not direct replacements for diuretics, but they may reduce the need for high diuretic doses.
Lifestyle and simple measures: Salt restriction, wearing compression stockings for leg swelling, weight control, and adjusting fluid intake can make a big difference. Sometimes these steps let you use a lower diuretic dose or switch to a milder drug.
How to decide: Talk with your doctor about the exact cause of swelling, your kidney function, blood tests (electrolytes, creatinine), and daily life needs. Changing diuretics means monitoring—expect follow-up labs and dose tweaks for a few weeks.
Quick safety tips: Never stop or switch diuretics on your own. Report dizziness, palpitations, muscle cramps, or sudden swelling. If you’re on blood pressure meds or potassium supplements, tell your clinician before any change.
Want help preparing for that conversation with your doctor? Make a short list: current symptoms, when they started, all meds and supplements, recent blood tests, and how often you urinate each day. That info speeds up choosing a safer, more convenient option.

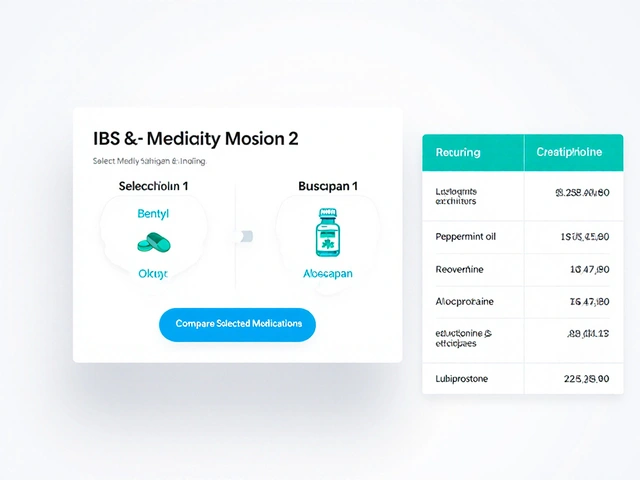
Lasix alternatives, such as Torsemide, Bumetanide, and Chlorthalidone, provide effective treatment for conditions like edema and hypertension. Each option comes with its own set of pros and cons, making it essential to understand which might be most suitable for individual needs. From loop diuretics to potassium-sparing options, these medications significantly impact fluid retention and blood pressure management. Additionally, Valsartan offers a unique approach as an angiotensin II receptor blocker, extending therapeutic choices for heart failure and hypertension. This article provides a comprehensive comparison of these alternatives to aid informed decision-making.
Continue Reading