Medication Hemorrhage: Risks, Causes, and What You Need to Know
When a medication hemorrhage, uncontrolled bleeding caused or worsened by drugs. Also known as drug-induced bleeding, it isn’t rare—it’s often preventable. This isn’t just about warfarin or aspirin. It’s about how everyday prescriptions, even ones you think are safe, can quietly turn dangerous when they interact with your body or other meds.
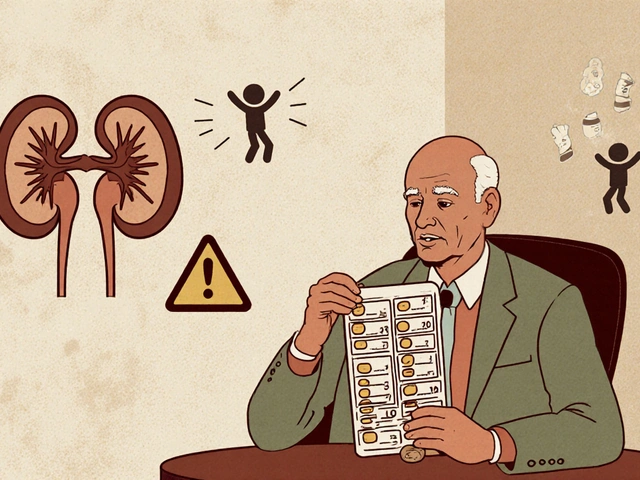
Think about anticoagulants, medications that prevent blood clots but increase bleeding risk. Drugs like warfarin, apixaban, or rivaroxaban are prescribed to protect your heart or brain from clots. But if your kidneys aren’t clearing them properly, or if you take them with NSAIDs, nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen that also affect blood clotting, the risk spikes. One study found that people on blood thinners who took daily NSAIDs had nearly triple the chance of serious bleeding. And it’s not just the dose—it’s the combo. Even a single extra pill can tip the scale.
Then there’s medication toxicity, when drugs build up in the body because organs like kidneys or liver can’t process them. This happens often in older adults or people with chronic kidney disease. Drugs like sulfonylureas for diabetes or certain antibiotics can turn toxic, and one side effect? Internal bleeding. You might not feel it until you’re bruising easily, passing dark stool, or feeling dizzy. No pain. No warning. Just a slow leak inside.
It’s not always about the drug itself. Sometimes it’s how you take it. Levothyroxine and PPIs interfere with absorption—but that’s not bleeding. Yet when someone’s on multiple meds, and their doctor doesn’t check for interactions, the system breaks down. A person on clopidogrel for a stent might also be taking omeprazole for heartburn, not realizing it reduces clopidogrel’s effect. So they get a clot. Or worse—they get a bleed because their doctor switched them to a different drug without knowing the full picture.
What you’ll find in these posts isn’t theory. It’s real cases. People who bled after starting a new pill. Elderly patients who didn’t know their kidney function had dropped. Nurses in the NICU watching preterm babies react to drugs meant for adults. Doctors facing lawsuits because a generic drug substitution went wrong. These aren’t outliers. They’re patterns. And they’re avoidable—if you know what to look for.
Some of the posts here show how a simple change—like switching from one nasal spray to another—can cut bleeding risk in sensitive patients. Others reveal how common drugs like prednisone or amitriptyline can silently weaken blood vessels over time. You’ll see how methadone can mess with heart rhythms, and how that connects to bleeding risk in people on multiple meds. You’ll learn how to spot the signs before it’s an emergency. And you’ll find out who’s most at risk—and why.

Severe bleeding from blood thinners like apixaban or warfarin can be life-threatening. Learn the warning signs, who’s at highest risk, and exactly what to do in an emergency-backed by 2025 clinical guidelines and real patient data.
Continue Reading