Sleep: Practical tips, what to try tonight, and how medicines affect sleep
Can’t fall asleep or waking up too early? You don’t need fancy gadgets. Small, consistent changes often help more than dramatic overnight fixes. This page gives simple steps you can try tonight, when to get medical help, and what common drugs do to your sleep so you can avoid surprises.
Start with routine. Go to bed and wake up at the same time every day, even weekends. Your body clocks respond to consistency more than long lists of rules. Cut caffeine at least 6 hours before bedtime. If you nap, keep it under 30 minutes and before mid-afternoon. That prevents naps from stealing your night sleep.
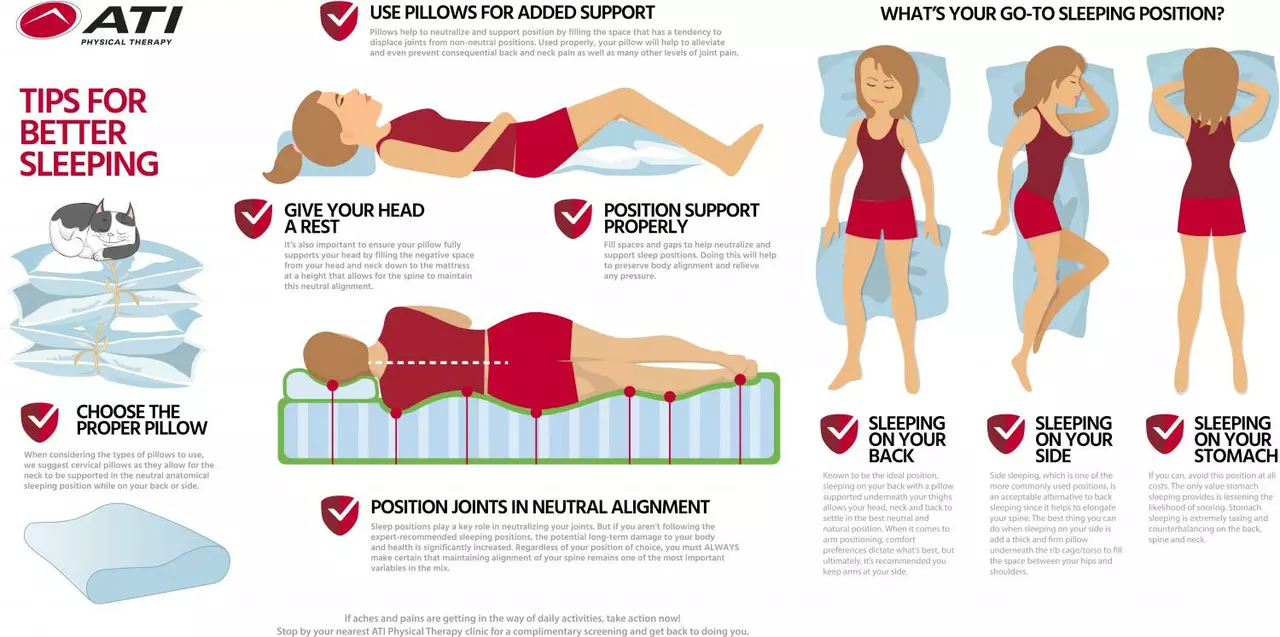
Make your bedroom work for sleep. Keep it cool, dark, and quiet. Use blackout curtains or a sleep mask and try white noise or earplugs if you’re easily disturbed. Reserve the bed for sleep and sex—avoid working or heavy phone use there. Devices with bright screens stimulate your brain; switch to low-light reading or a calming routine like stretching or breathing exercises.
Quick behavioral tips that actually help
If you can’t sleep after 20 minutes, get up. Move to another room and do something calm—read under dim light or practice slow breathing—then return when you feel sleepy. Avoid clock-watching; it raises stress. Try a 10–20 minute relaxation practice before bed: slow breathing (4–6 breaths per minute), progressive muscle relaxation, or a short guided sleep audio.
Watch what you eat and drink. Heavy meals right before bed, lots of sugar, or alcohol can break sleep later in the night. Alcohol may make you fall asleep faster, but it fragments sleep and reduces REM. A light snack with protein and carbs (like yogurt and a banana) can help if hunger wakes you.
Medications, mental health, and when to see a doctor
Some medicines make you sleepy; others cause insomnia. Antidepressants like paroxetine can change sleep patterns—either causing drowsiness or trouble sleeping. Antipsychotics are sometimes used for sleep but can carry serious side effects; if you’re reading about Seroquel alternatives, talk to a clinician before switching meds. Epilepsy and brain-targeting drugs (SV2A-related treatments) can also affect sleep; report new sleep changes to your prescriber.
Use OTC sleep aids sparingly. Melatonin can help with jet lag or shifting schedules but isn’t a cure for chronic insomnia. Diphenhydramine and other antihistamines cause next-day grogginess for many people. Prescription sleep meds work short-term for some people, but they’re not a long-term fix without behavior change.
See a doctor if you: fall asleep during daytime activities, snore loudly with gasping or pauses, have sleep problems lasting more than a month, or if poor sleep affects your mood, thinking, or safety. Ask about sleep apnea testing, CBT-I (cognitive behavioral therapy for insomnia), and medication review if you take drugs that might be the problem.
Want more on how meds and mental health affect sleep? Read our posts: "9 Alternatives to Seroquel", "A Closer Look at Paroxetine's Side Effects", "Panic Disorder and Dating", and "SV2A: Unlocking New Hope for Psychiatric and Neurodegenerative Diseases". If you need help picking an article or want a quick answer about interactions, use our contact page to reach PrescriptionPoint.SU.
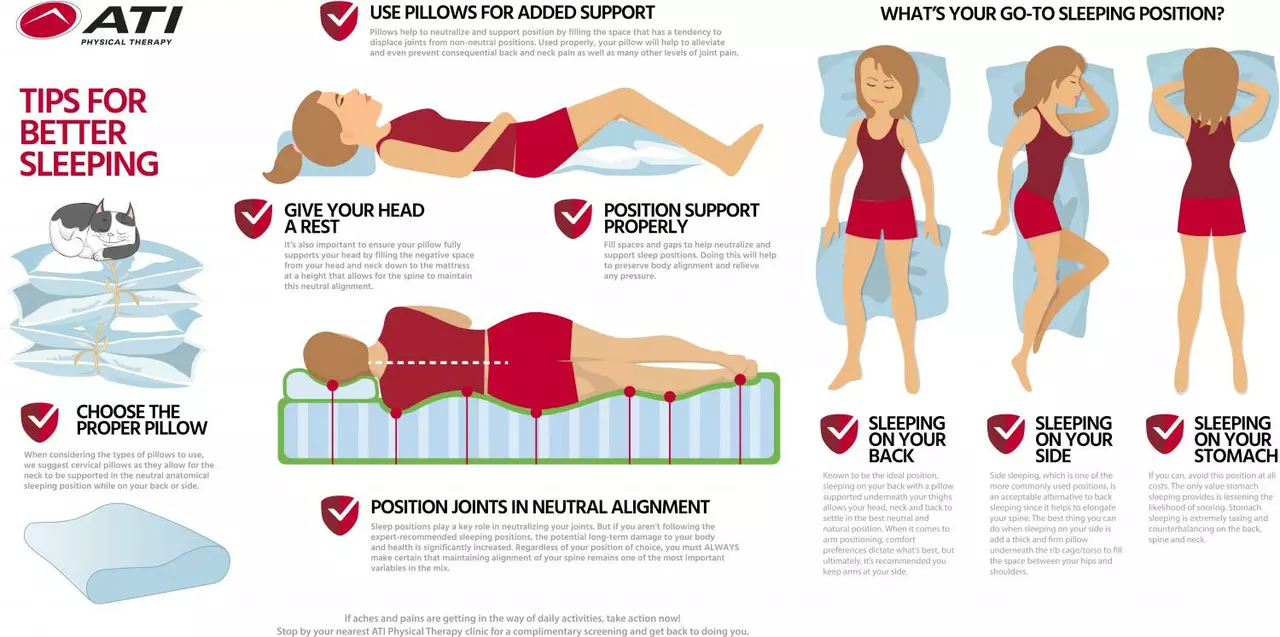
As someone who struggles with ADHD, I understand how difficult it can be to get a good night's sleep. To help combat this issue, I've recently looked into some tips for a better night's rest. I learned that creating a consistent bedtime routine, minimizing distractions in the bedroom, and incorporating relaxation techniques can make a huge difference. Additionally, regular exercise and limiting caffeine intake can also contribute to a more restful sleep. I'm excited to try these tips and hope they can help others with ADHD as well.
Continue Reading