Urine leakage: quick, practical help you can use today
Urine leakage (urinary incontinence) is more common than you think — and you don’t have to live with it. This page gives clear, practical steps you can try at home, what treatments your doctor might offer, and the signs that mean you should get medical help. No fancy terms, just stuff that works.
Common causes and types
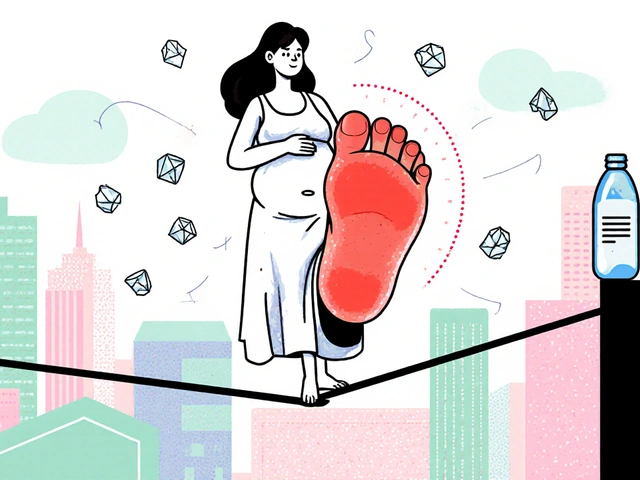
There are a few main types of leakage. Stress incontinence happens when pressure from coughs, sneezes, or lifting causes leaks. Urge incontinence is a sudden, strong need to go and sometimes you don’t make it. Mixed incontinence is both. Other causes include pregnancy and childbirth, menopause, obesity, chronic cough, constipation, certain medicines, and nerve or bladder problems. Knowing the type helps pick the right fix.
Practical steps you can try right away
Start with simple changes that often cut down leaks fast. First: try pelvic floor (Kegel) exercises. Squeeze the muscles you use to stop the flow of urine, hold 3–5 seconds, relax 3–5 seconds. Do 10–15 reps, three times a day. Be consistent — results usually show in 4–8 weeks.
Next: bladder training. Delay going to the bathroom by 10–15 minutes when you feel an urge. Gradually increase the delay. This re-teaches your bladder to hold more and reduces sudden urges.
Watch what you drink. Cut back on caffeine, alcohol, and large evening fluids. Don’t overdo fluid restriction — aim for steady hydration across the day. Also, treat constipation if you have it; a full bowel can push on the bladder and make leakage worse.
Lose extra weight if you can. Even small weight loss can lower pressure on the bladder and reduce stress leaks. Use absorbent pads or underwear to protect clothes while you work on fixes — they’re better than avoiding social outings.
If medicines might be the cause, review them with your doctor. Some blood pressure drugs, muscle relaxants, or sedatives can affect bladder control.
When simple changes aren’t enough, treatments exist. Your doctor may suggest pelvic floor physical therapy, prescription medicines (like anticholinergics or mirabegron), pessaries for women, or procedures such as sling surgery or injections. Each has pros and cons, so ask about risks and recovery time.
See a doctor sooner rather than later if you have sudden new leakage, blood in the urine, pain, fever, trouble emptying the bladder, or if leakage limits your daily life. Those signs need prompt evaluation to rule out infection, stones, or neurological causes.
Small steps add up. Try the exercises and bladder training for a few weeks, cut back on triggers, and talk to a healthcare pro if things don’t improve. You don’t have to accept leaks as normal — help is available and often effective.

As a woman going through menopause, I've recently discovered that urine leakage is a common issue many of us face during this time. It's important to understand that this is not uncommon and is often caused by hormonal changes and weakened pelvic muscles. To manage this, I've found that incorporating pelvic floor exercises and maintaining a healthy weight can help. Discussing this concern with your healthcare provider can provide more tailored advice and treatment options. Remember, you're not alone in this experience, and there's help available to manage this symptom of menopause.
Continue Reading