Gallbladder and Biliary Disease: Understanding Stones, Cholangitis, and ERCP
When your gallbladder stops working right, the pain doesn’t just come and go-it hits like a sledgehammer. You might feel it after eating a fatty meal: a deep, steady ache under your right ribs that lasts for hours, sometimes radiating to your back or shoulder. For many, this is the first sign of gallbladder stones, the most common biliary problem affecting nearly 1 in 6 adults in the U.S. But stones are just the beginning. Left untreated, they can trigger life-threatening infections like cholangitis or require a procedure called ERCP to fix. Understanding what’s happening inside your bile system isn’t just helpful-it can save you from unnecessary surgery, prolonged pain, or hospital stays.
What Are Gallstones, and Why Do They Form?
Gallstones aren’t just random lumps. They’re hardened deposits made from bile, the fluid your liver produces to help digest fats. About 80% of them are made of cholesterol. The rest are pigment stones, mostly bilirubin, a waste product from broken-down red blood cells. When your bile has too much cholesterol or bilirubin, or not enough bile salts, crystals start forming. Over time, these crystals grow into stones-some as small as grains of sand, others as big as golf balls.Women are more likely to get them, especially after pregnancy or hormone therapy. Obesity, rapid weight loss, diabetes, and being over 60 all raise your risk. Native Americans, particularly Pima Indians, have the highest rates globally-up to 64% in some groups. In the U.S., around 20.5 million people have gallstones, with women making up 14.2 million of those cases.
The scary part? Most people never know they have them. Around 80% of gallstones are silent. You might live your whole life with them and never need treatment. But if one blocks the cystic duct-the tube that drains your gallbladder-it causes inflammation called acute cholecystitis. That’s when the pain becomes constant, fever kicks in, and your belly feels tender to the touch.
Cholangitis: When the Bile Ducts Get Infected
When a stone moves out of the gallbladder and gets stuck in the common bile duct, things get serious. This duct carries bile from your liver and gallbladder into your small intestine. Block it, and bile backs up. Bacteria that normally live in your gut-like E. coli or Klebsiella-can travel up the duct and cause an infection. That’s cholangitis.It’s not just uncomfortable-it’s dangerous. The classic signs, called Charcot’s triad, are right upper quadrant pain, fever, and jaundice (yellow skin or eyes). If you’re also confused, have low blood pressure, or are shivering uncontrollably, you’ve moved into Reynolds’ pentad. That means you’re septic. Without quick treatment, cholangitis can lead to organ failure or death.
Studies show that 70% of cholangitis patients have pain, 85% have fever, and 60-70% show jaundice. The infection usually happens because a stone blocked the ampulla of Vater-the spot where the bile duct and pancreatic duct meet. That’s also the same spot that can trigger gallstone pancreatitis, another serious complication.
ERCP: The Procedure That Can Fix Both Diagnosis and Damage
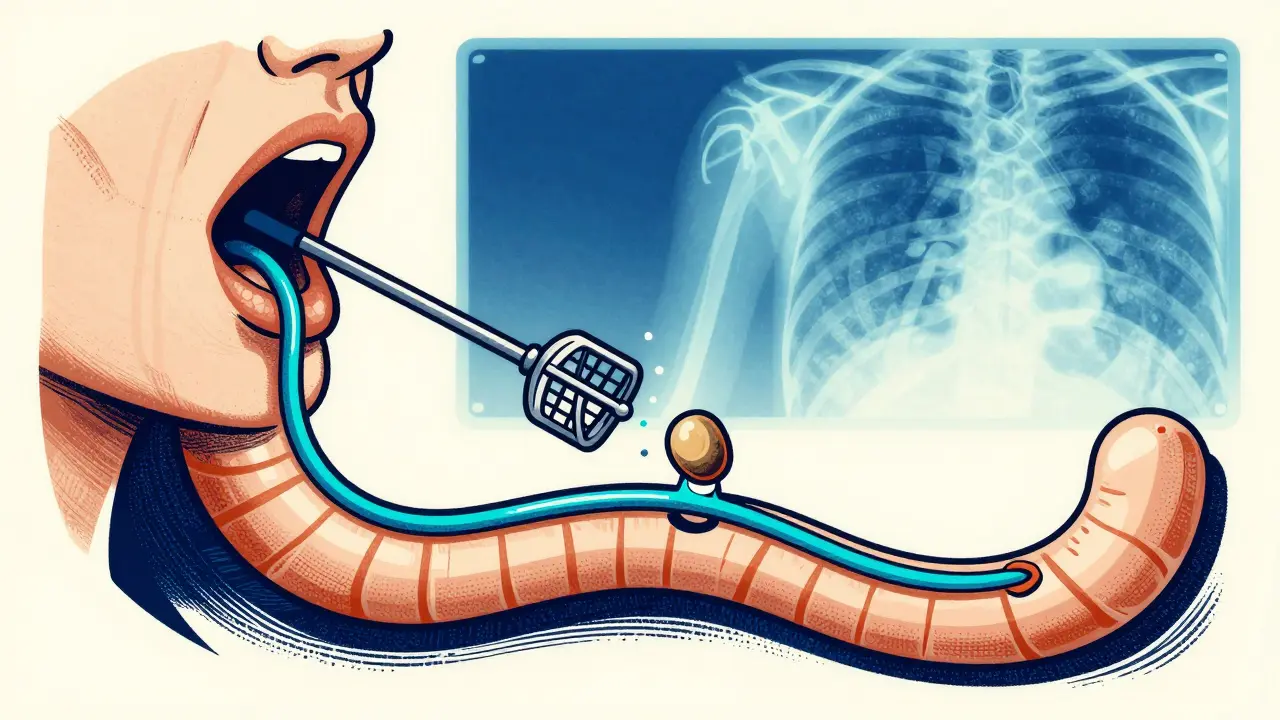
If your doctor suspects a stone in your bile duct, they won’t start with surgery. First, they’ll order an ultrasound-it’s quick, safe, and catches gallstones in the gallbladder with 84% accuracy. But for stones in the bile ducts, they’ll turn to MRCP, a non-invasive MRI scan that’s 95% sensitive and 97% specific. If it shows a blockage, the next step is often ERCP.ERCP stands for Endoscopic Retrograde Cholangiopancreatography. It’s not simple. A thin, flexible tube with a camera (an endoscope) is threaded through your mouth, down your throat, into your stomach, and then into the first part of your small intestine. There, the doctor finds the opening of the bile duct, injects dye, and takes X-rays to see the blockage. Then, they use tiny tools to cut the muscle around the duct (sphincterotomy), remove the stone with a balloon or basket, or place a stent to keep the duct open.
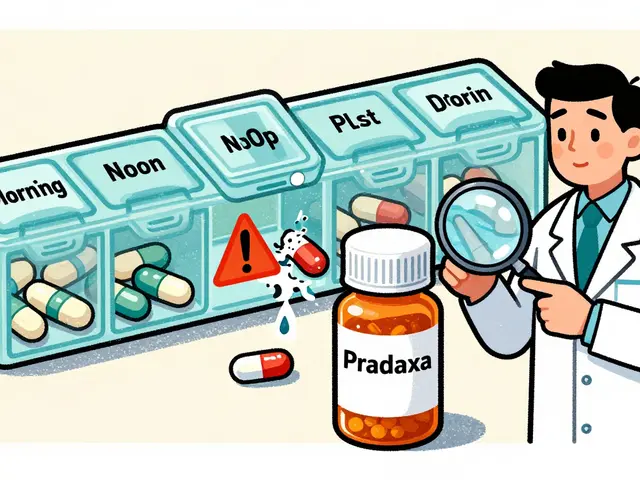
It’s not perfect. About 3-10% of people develop post-ERCP pancreatitis-a painful inflammation of the pancreas that can require hospitalization. The risk is higher if you’ve had it before, have Sphincter of Oddi dysfunction, or if the procedure is done by someone with less experience. High-volume centers-those doing over 100 ERCPs a year-have 20% fewer complications than low-volume ones.
But when it works, it works well. Success rates for stone removal are 85-95%. Many patients are back to desk work in 48 hours. One Reddit user wrote, “ERCP recovery was surprisingly quick-I was back to desk work in 48 hours but the throat soreness lasted about 5 days.”
What Happens After ERCP or Gallbladder Removal?
If you have symptomatic gallstones, the most common treatment is laparoscopic cholecystectomy-removing the gallbladder through small belly incisions. It’s done in 90% of cases today. Recovery is fast: most people go home the next day and are back to normal in 7-10 days. Compare that to open surgery, which used to mean a 4-6 week recovery and a long scar.But removing the gallbladder doesn’t fix everything. About 12% of people still have abdominal pain afterward-called post-cholecystectomy syndrome. Some get diarrhea because bile now flows constantly into the intestine instead of being stored. Loperamide (Imodium) helps some, but not all. One person on Reddit said, “I still need loperamide six months later.”
Medications like ursodeoxycholic acid (UDCA) can dissolve small cholesterol stones, but only in about 30-40% of cases-and only if the stone is under 15mm. It takes 6 to 12 months. It doesn’t work on pigment stones at all. Shock wave therapy used to be tried, but it had a 50% recurrence rate within five years. Today, it’s rarely used.
When to Skip Surgery-And When You Absolutely Need It
Here’s the thing most people don’t realize: if you have gallstones but no symptoms, you probably don’t need surgery. The risk of a future complication is only 1-2% per year. That means for every 100 people with silent stones, only 1 or 2 will ever have a serious problem. Surgery carries its own risks-bleeding, infection, bile leaks. So unless you’re having pain, fever, or jaundice, doctors recommend watchful waiting.But if you’ve had one attack, your chance of another is 70% within 10 years. And each attack increases your risk of complications. That’s why many doctors recommend surgery after the first episode. Especially if you’re young, healthy, and can afford the recovery time.
There’s another gap in care: only 30-40% of patients with bile duct stones get them removed during the same surgery as their gallbladder. Instead, they go home, then come back weeks later for ERCP. That’s extra cost, extra stress, and extra risk. Experts now push for coordinated care-gastroenterologists and surgeons talking before surgery to plan one-time stone removal.
What’s New in Gallbladder and Biliary Care?
Technology is changing fast. In 2023, the FDA approved a new duodenoscope with a fully disposable elevator mechanism. That’s a big deal. Between 2013 and 2018, faulty scopes caused 112 outbreaks of drug-resistant infections. Now, the part that touches inside the body is thrown away after each use.Another advance: intraductal ultrasonography (IDUS). It’s a tiny ultrasound probe you thread through the ERCP scope. It can see stones smaller than 5mm-ones standard X-rays miss. Sensitivity jumps from 75% to 92%. That means fewer missed diagnoses and fewer repeat procedures.
Research is also looking for better drugs to dissolve pigment stones, which currently have no effective medical treatment. And telehealth follow-ups after ERCP are cutting 30-day readmissions by 18% in pilot programs.
But the biggest challenge? Training. ERCP is hard. It takes 150-200 procedures for a doctor to become competent. In rural hospitals, staff might only do 10 a year. Meanwhile, academic centers are doing complex cases with robotic assistance. The gap is growing. Experts warn that without better training standards, outcomes will keep varying wildly.
Living After Gallbladder Removal
You don’t need your gallbladder to live. Your liver still makes bile-it just flows straight into your intestine instead of being stored. Most people adjust within weeks. But for some, it’s trickier. High-fat meals can still trigger diarrhea or bloating. The fix? Eat smaller, more frequent meals. Avoid fried foods, creamy sauces, and heavy desserts for the first month. Most people can return to normal eating in 6 weeks.One study found that 87% of patients reported major symptom improvement within 30 days after surgery. Average satisfaction? 4.5 out of 5 stars. But the ones who struggled? They often didn’t get clear instructions. Patient satisfaction with ERCP jumps from 52% to 78% when doctors take time to explain what to expect-before, during, and after.
Bottom line: if you’ve had one gallbladder attack, don’t wait for the next. Talk to your doctor about imaging, whether you have bile duct stones, and whether surgery is right for you. Don’t assume silent stones are harmless. Don’t assume ERCP is a cure-all. And don’t skip the follow-up. Your bile ducts are delicate. Treat them like the vital system they are.





13 Comments
michelle Brownsea
January 19 2026Let me just say-this is the most responsibly written medical overview I’ve seen in years. No sensationalism, no clickbait, just cold, hard facts wrapped in clarity. People need to understand that gallstones aren’t ‘just a gallbladder issue’-they’re a systemic bile crisis waiting to happen. And yet, so many doctors still treat them like a minor inconvenience. The stats on silent stones? Chilling. And the fact that 70% of cholangitis cases present with Charcot’s triad? That’s not coincidence-that’s biology screaming for attention.
Also, can we talk about how ERCP is still being performed by doctors who’ve done 10 procedures a year? That’s not medicine-it’s Russian roulette with a duodenoscope. The FDA’s new disposable elevator mechanism? Long overdue. I’m glad someone finally said it: training gaps are killing people, and we’re pretending they don’t exist.
MARILYN ONEILL
January 20 2026I had mine out last year. Worst. Decision. Ever. Now I get diarrhea if I look at cheese. Why did they even make this thing if we don’t need it? I feel like my body was tricked. Now I’m just a bile leak waiting to happen. 😭
Kevin Narvaes
January 21 2026bro i got my gallbladder removed and now i just eat pizza like its a religious experience. i dont care if i get diarrhea after. life is short. also i think the liver is just gonna do what it wants anyway. why are we even surgically fixing this? maybe we should just accept that our bodies are messy machines. 🤷♂️
Dee Monroe
January 22 2026There’s something deeply poetic about the human body’s resilience-how it can carry stones for decades without a whisper, then suddenly, one tiny obstruction turns your entire existence into a hospital room. It’s not just anatomy, it’s philosophy. We spend so much time trying to fix what’s broken, but rarely pause to consider why the system failed in the first place. Is it diet? Stress? Genetics? Or are we simply out of sync with the rhythms our bodies evolved to follow? The gallbladder doesn’t hate us-it’s trying to tell us something. Maybe we’re not meant to eat double cheeseburgers three times a week. Maybe our ancestors didn’t have 24/7 access to saturated fats, and our biology hasn’t caught up. We treat symptoms like enemies, but what if they’re messengers?
And ERCP? It’s not just a procedure-it’s a dance between human ingenuity and biological chaos. A camera threading through your throat to reach a duct you didn’t even know existed. It’s terrifying. And beautiful. And we do it because we refuse to let pain win. That’s not medicine. That’s love.
But we must be gentle with ourselves afterward. Post-cholecystectomy syndrome isn’t failure-it’s adaptation. And if you need Imodium for six months? So what. You’re alive. You’re learning. You’re adjusting. That’s not weakness. That’s wisdom.
Jerry Rodrigues
January 22 2026Good breakdown. I’ve had two episodes. First one scared me. Second one I just ate ginger tea and waited it out. Still no surgery. My doc says watch and wait. Makes sense to me.
Barbara Mahone
January 23 2026As someone who grew up in a household where gallbladder removal was the default answer, I’m glad to see nuance here. My mother had hers out in the ‘80s and spent years blaming every stomach ache on it. Turns out, it was lactose intolerance. We need more education, not more surgeries. Also, the part about coordinated care? Spot on. Why make patients jump through hoops?
Samuel Mendoza
January 25 202680% silent? That’s not a disease. That’s a myth. If it doesn’t hurt, it doesn’t matter. Stop scaring people.
Stephen Rock
January 26 2026ERCP is a glorified torture device with a 10% chance of pancreatitis. And they call it ‘minimally invasive’? Please. I’ve seen patients cry from the throat soreness alone. And now they’re pushing disposable scopes? Took them 10 years to fix a design flaw that killed people. Classic.
Amber Lane
January 27 2026I’m so glad this exists. My mom had cholangitis last year. She didn’t know what was happening until she turned yellow. This should be required reading.
Ashok Sakra
January 28 2026in india we just use turmeric and hot water. why do you need all this tech? your body knows what to do. you just need to trust it. i had stones and i drank warm water with lemon for 3 weeks. gone. no surgery. no endoscopy. just faith.
Andrew Rinaldi
January 28 2026It’s interesting how we’ve turned something so natural-bile flow-into a crisis that needs intervention. Maybe the real issue isn’t the stones, but our relationship with food. We eat too fast, too processed, too often. The gallbladder is just the messenger. We’re the ones who need to change.
Gerard Jordan
January 28 2026👏 This is the kind of content we need more of. No fluff, just facts. And the part about high-volume centers having 20% fewer complications? That’s huge. Let’s push for better standards, not just more procedures. 🙌 #HealthcareImprovement
Roisin Kelly
January 29 2026They’re lying about ERCP. The real reason they push it is because insurance pays more for procedures than for education. You think they care about your bile ducts? No. They care about your copay. This whole system is a money machine. And you’re just the product.