How to Use Compounded Medications for Children Safely
When your child can’t swallow a pill, or the only available medicine has sugar, alcohol, or dyes that trigger allergies, compounded medications can feel like a lifesaver. But here’s the hard truth: compounded medications for children are not FDA-approved. That means no independent testing for strength, purity, or safety. And for kids-especially babies and toddlers-that gap can be deadly.
Why Compounded Medications Are Used for Kids
Most kids don’t need custom drugs. But some do. Compounded medications are made when nothing off-the-shelf works. For example:- A child with a severe allergy needs a dye- and alcohol-free version of their antibiotic.
- A toddler with reflux can’t tolerate the bitter taste of liquid amoxicillin, so the pharmacist adds cherry flavor and removes alcohol.
- A premature baby in the NICU needs a tiny dose of morphine, diluted from an adult vial.
- A diabetic child needs sugar-free levothyroxine because the commercial version contains glucose.
The Hidden Risks in Every Dose
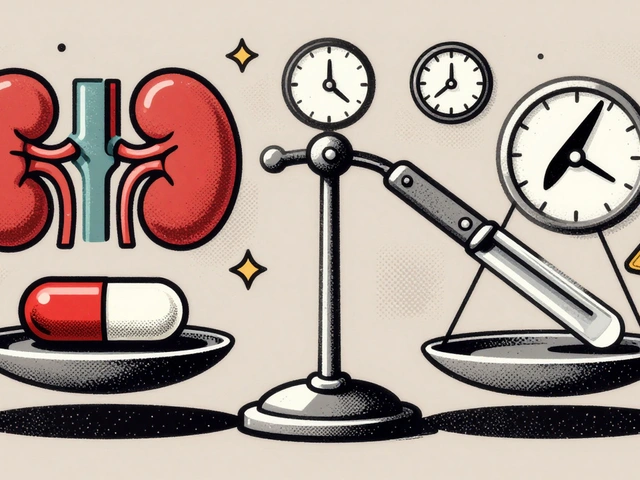
The biggest danger isn’t the drug itself-it’s the dose. Kids aren’t small adults. A milligram too much can cause seizures. A milligram too little can mean the medicine doesn’t work at all. In 2024, the Institute for Safe Medication Practices found that 14-31% of pediatric medication errors involve compounded drugs. Most of those are dosing mistakes. Why?- Concentration confusion: A bottle labeled "10 mg/mL" might actually contain 1 mg/mL. That’s a 90% underdose.
- Wrong unit: A pharmacist writes "5 mL" but the parent reads "5 tsp" (which is 25 mL).
- Expired or unstable formulas: Some liquid compounds lose potency after 14 days, but labels don’t always say so.
What Makes a Compounding Pharmacy Safe?
Not all pharmacies are equal. Some follow strict rules. Others cut corners. Here’s how to tell the difference:- Look for PCAB or NABP accreditation. Only about 1,400 of the 7,200 compounding pharmacies in the U.S. have this. It means they’ve passed independent audits for cleanliness, training, and accuracy.
- Ask if they use gravimetric analysis. This is a high-tech scale that measures ingredients by weight, not volume. It’s far more accurate than using syringes or measuring cups. Only 7.7% of U.S. hospitals use it-mostly because it costs $25,000 to $50,000 per station. But if your child’s medication is sterile or life-critical, this isn’t optional.
- Check if they do double-checks. Every pediatric compound should be verified by two trained pharmacists before it leaves the lab. Ask if they do this. If they say "no," walk out.
- Verify their state license. All compounding pharmacies must be licensed by their state board. You can look up their license online through your state’s pharmacy board website.

What You Must Do as a Parent
You’re the last line of defense. No pharmacist or doctor will be with your child 24/7. You have to ask the right questions-and know what to look for.- Ask for the exact concentration. Don’t settle for "this is the dose." Ask: "What is the strength in mg/mL?" Write it down. Compare it to the prescription.
- Confirm the dosing instructions with both the doctor and pharmacist. If they give different answers, stop. Call the doctor’s office. Ask them to clarify in writing.
- Check the label. Does it say "For external use only" but you’re giving it by mouth? Does it say "Refrigerate" but you left it on the counter? Read every word.
- Ask about expiration. Liquid compounds often expire in 7-30 days. If the bottle doesn’t list an expiration date, don’t use it.
- Use the right measuring tool. Never use a kitchen spoon. Use the syringe or cup that came with the medication. If none was provided, ask for one. A standard syringe is the most accurate.
- Watch for side effects. If your child vomits, has diarrhea, seems unusually sleepy, or develops a rash after starting a new compounded med, call the doctor immediately. Don’t wait.
When to Avoid Compounded Medications Altogether
Sometimes, the safest choice is to say no. The FDA says: "Unnecessary use of compounded drugs may expose patients to potentially serious health risks." That applies to kids more than anyone. Avoid compounded versions if:- A commercial version exists-even if it’s unflavored or harder to swallow. You can mix it with applesauce or use a pill crusher (with your pharmacist’s approval).
- The drug is for weight loss, hormone therapy, or anti-aging. These are often sold as "compounded" to bypass FDA rules. They’re not safe for children.
- The pharmacy doesn’t have accreditation or refuses to answer questions about their process.
- The medication is being made in bulk because of a "drug shortage." That’s a red flag. The FDA has warned that some pharmacies are exploiting shortages to mass-produce unapproved drugs.

The Bigger Picture: Why This Keeps Happening
The compounding industry is growing fast-$11.3 billion in 2024. But safety hasn’t kept up. Most pharmacies still use manual methods: syringes, measuring cups, and human judgment. That’s how errors happen. The technology to fix this exists. Gravimetric analysis reduces dosing errors by 75%. But it’s expensive. And training takes weeks. So most pharmacies skip it. The Emily Jerry Foundation was started after a 2-year-old died from a compounded chemotherapy error in 2006. The same technology that could’ve saved her was available then. It’s still not standard today. Twenty-eight states are now considering laws requiring gravimetric verification for pediatric sterile compounds. That’s progress. But until it’s federal law, the burden falls on parents.Final Advice: Trust But Verify
Compounded medications have a place in pediatric care. But they’re not safer just because they’re made "just for your child." They’re riskier-because they’re untested, unregulated, and often made in conditions that aren’t sterile. Your job isn’t to avoid them entirely. It’s to demand proof of safety. Ask questions. Write down concentrations. Double-check doses. Use a syringe. Don’t trust labels. Don’t trust assumptions. And if something feels off-stop. Call the doctor. Call the pharmacist. Call again. Your child’s life depends on your attention to detail. No one else is watching as closely as you are.Are compounded medications FDA-approved?
No. Compounded medications are not FDA-approved. The FDA does not test them for safety, effectiveness, or quality before they’re given to patients. This means the strength, purity, and stability of the drug aren’t guaranteed. That’s why it’s critical to use only accredited pharmacies and verify every dose.
How do I know if my child’s compounded medication is safe?
Check if the pharmacy is accredited by PCAB or NABP. Ask if they use gravimetric analysis for dosing. Confirm they perform independent double-checks on every pediatric compound. Ask for the exact concentration (in mg/mL) and verify it matches the prescription. If they can’t answer these questions clearly, find another pharmacy.
Can I use a kitchen spoon to measure my child’s liquid medicine?
Never. Kitchen spoons vary in size and are extremely inaccurate. A teaspoon can hold anywhere from 3 to 7 milliliters. Always use the syringe or dosing cup provided by the pharmacy. If none was included, ask for one. A 1 mL syringe is the most precise tool for small pediatric doses.
What should I do if my child has a bad reaction to a compounded medication?
Stop giving the medication immediately. Call your child’s doctor and the pharmacist. Report the reaction to the FDA’s MedWatch program. Save the medication bottle and packaging-this will help investigators trace the issue. Document symptoms, timing, and dosage. Many adverse events from compounded drugs go unreported, but your report could help prevent another child’s harm.
Is it okay to use a compounded version of a drug that’s available commercially?
Only if the commercial version truly doesn’t work for your child. For example, if your child has a severe allergy to dyes or preservatives in the brand-name version, then a compounded alternative may be necessary. But if it’s just because the taste is bad or the pill is hard to swallow, try other solutions first-like mixing with food, using a pill crusher, or asking for a different formulation. Compounded drugs carry higher risks, so avoid them unless absolutely needed.
How long do compounded medications last?
It varies. Oral liquids usually expire in 14 to 30 days, depending on ingredients and storage. Sterile injectables may expire in just 7 days. The pharmacy should label the bottle with an expiration date. If they don’t, ask for it. Never use a compounded medication past its expiration date-even if it looks fine. Potency drops over time, and contamination can grow.
Can I get a compounded medication from any pharmacy?
Technically, yes-but you shouldn’t. Most pharmacies don’t have the training or equipment to safely compound for children. Only use pharmacies accredited by PCAB or NABP. These pharmacies undergo strict audits for cleanliness, accuracy, and staff training. Avoid online pharmacies or those that offer bulk compounding for non-prescription uses like weight loss or hormones.




14 Comments
Chris Taylor
November 29 2025My kid had a reaction to a compounded antibiotic last year. We didn't know the difference between a syringe and a teaspoon. Ended up in the ER. Never again. Always ask for the exact concentration. Write it down. Seriously.
Sean Slevin
November 30 2025Wow. Just... wow. I never realized how many ways this can go wrong. The dose confusion thing? Like, a 90% underdose? That's not a mistake, that's a catastrophe waiting to happen. And why aren't we forcing every pharmacy to use gravimetric analysis? It's not expensive compared to a child's life. I mean, come on. We have robots that can assemble iPhones, but we're still using measuring cups for kids' meds? This is insane. We need a national standard. Like, now. Like, yesterday. Please? Someone? Anyone?
Melissa Michaels
December 2 2025As a pediatric pharmacist for 18 years, I can confirm the risks outlined here are real and underreported. Accreditation matters. Double-checks are non-negotiable. We use gravimetric analysis for every pediatric compound, even if it takes twice as long. The cost is worth it. Parents must demand this. If a pharmacy hesitates or refuses, find another. Your child's safety is not a negotiation.
Nathan Brown
December 3 2025It's funny how we trust a pill from a billion-dollar pharma company but freak out about a custom mix from a local pharmacy. But here's the truth-we don't trust the system. We trust the person. The pharmacist who looks you in the eye and says, 'I double-checked this myself.' That's the real safety net. Not the label. Not the accreditation. The human being behind the counter. And if that person is rushed, distracted, or underpaid? We're all just one bad day away from tragedy. We need to pay them better. And listen to them.
Olivia Currie
December 4 2025I read this with my hands shaking. My daughter almost died from a compounded thyroid med. The pharmacy said it was 'just a little weaker.' A LITTLE? She stopped growing. Stopped talking. We thought it was autism. It was a 40% underdose. I screamed for weeks. I still cry when I see that bottle. If you're using compounded meds-ASK. WRITE. VERIFY. DON'T LET THEM TELL YOU IT'S FINE. IT'S NOT.
Curtis Ryan
December 4 2025So many typos in this post but so much truth!! I'm not a doctor but I'm a dad and I learned the hard way-never use a kitchen spoon. EVER. Got a syringe from the pharmacy, labeled it with masking tape, and taped it to the fridge. My kid's life is worth the extra step. Seriously, people. Just use the syringe.
Rajiv Vyas
December 4 2025They're lying to you. The FDA doesn't regulate compounding because they're in bed with Big Pharma. Why? Because generics and compounding cut into profits. They want you to buy expensive brand-name pills even if your kid is allergic. This is all a scam. You think they care about your kid? They care about their stock price. Go to Canada. Or Mexico. Or find a compounding pharmacy that doesn't use 'FDA-approved' ingredients. That's the real safety.
farhiya jama
December 6 2025Ugh. I don't even know why I'm reading this. I just want my kid to take medicine without a whole documentary. Can't we just give them a gummy? Why does everything have to be so dramatic? I'm tired.
Astro Service
December 7 2025Why are we letting some foreign pharmacist make our kids' medicine? We have the best scientists in the world. Why not just make a real pill? This is why America is falling apart. We outsource everything. Even our kids' medicine. Get a real pharmacy. Get a real drug. Stop this nonsense.
DENIS GOLD
December 7 2025Oh wow. Another 'parent panic' article. Next they'll tell us not to let our kids breathe unfiltered air. Compounded meds are fine. If you're too lazy to crush a pill or mix it with jelly, that's your problem. Stop blaming the pharmacist. Blame yourself for not reading the label. And for crying out loud, stop using emojis when you're talking about your kid's life.
Ifeoma Ezeokoli
December 7 2025This is why I always ask my pharmacist to explain everything twice. I'm from Nigeria, and here, we know that medicine is sacred. You don't just mix things and hope. You check. You verify. You honor the life you're trying to heal. This post? It's a prayer. Read it. Share it. Don't let your child become a statistic.
Daniel Rod
December 8 2025My son’s compounded insulin was off by 20%. We didn’t know until his glucose spiked. I still have the bottle. I keep it on my nightstand. Not as a reminder to be scared. But as a reminder to be loud. If you see a pharmacy that won’t show you their accreditation? Call the state board. Post it on Reddit. Tag your rep. This isn’t just about medicine-it’s about dignity. Every child deserves to be measured with precision, not guesswork. 🙏
gina rodriguez
December 9 2025I just wanted to say thank you for writing this. I was so scared to ask questions when my daughter’s med was compounded. I thought I’d sound dumb. But I asked-and the pharmacist gave me a whole handout. Now I always ask. And I always write it down. You’re not being difficult. You’re being a hero.
Matthew Stanford
December 9 2025Let’s be real: this isn’t just about pharmacies. It’s about how we value care. We pay $100 for a coffee maker that measures water to the milliliter, but we let a $20 medication be mixed by hand with a syringe? That’s not negligence. That’s a cultural failure. We need to treat pediatric compounding like we treat airplane safety. No shortcuts. No compromises. No exceptions. Because children aren’t ‘small adults.’ They’re everything.