International Generic Drug Prices: How U.S. Costs Compare Globally
When you walk into a pharmacy in the U.S. and see a $6 copay for your generic blood pressure pill, it’s easy to think you’re getting a deal. But here’s the twist: generic drugs in America are actually cheaper than in most other wealthy countries. That’s right. While brand-name drugs in the U.S. cost nearly four times more than elsewhere, the generics you rely on every day? They’re often priced lower than in Canada, Germany, or even Japan.
Why U.S. Generic Prices Are Lower
The reason comes down to competition. In the U.S., once a brand-name drug’s patent expires, dozens of companies rush to make the same pill. The FDA approved 773 generic drugs in 2023 alone. When three or more companies start selling the same generic, prices collapse. By the time four manufacturers are in the game, the price often drops to just 15-20% of what the original brand charged. That’s not how it works in most other countries. Many governments limit how many generic makers can enter the market. Some even set fixed prices that don’t drop with competition. In France and Japan, for example, regulators cap prices before competition even begins. The result? Fewer companies make the drug, and prices stay higher. In the U.S., you don’t just get one or two generic options-you get 10, 15, even 20. That’s why the average generic copay is $6.16, compared to $56.12 for a brand-name drug. Over 93% of generic prescriptions cost less than $20. In contrast, countries like the U.K. and Canada often charge $15-$30 for the same generic pill.The Brand-Name Problem
But here’s where things get ugly. While generics are cheap, brand-name drugs in the U.S. are the most expensive in the world. A 2022 RAND study found U.S. brand-name drug prices were 422% higher than in other OECD countries. That means if a drug costs $100 in Germany, you’ll pay $422 for the same one in the U.S. Why? Because the U.S. doesn’t negotiate drug prices like other countries do. Medicare, the largest health program in the country, only started negotiating prices in 2023-and even then, it only picked 10 drugs. The first negotiated price for Jardiance, a diabetes drug, was $204. In Australia, the same drug costs $52. In Japan? $48. That’s more than four times higher. The problem isn’t just Medicare. Private insurers pay even more. Pharmaceutical companies set list prices high, then offer secret rebates to insurers. That’s why the headline price you see is often not what anyone actually pays. But for patients without insurance, or those in the Medicare coverage gap, that high list price is what they’re stuck with.Net vs. Gross Prices: The Hidden Math
You’ll hear conflicting numbers about whether U.S. drug prices are high or low. That’s because people are comparing different things. - Gross prices: What the manufacturer lists on the invoice. These are sky-high in the U.S. for brand-name drugs. - Net prices: What insurers and government programs actually pay after rebates and discounts. A 2024 University of Chicago study found that when you look at net prices-what Medicare, Medicaid, and other public programs pay-the U.S. actually spends 18% less on prescription drugs than Canada, Germany, the U.K., France, and Japan combined. How? Because public programs have massive buying power. Medicare covers over 65 million people. Medicaid covers 90 million. When you negotiate for that many people, you can drive prices down. The U.S. system works like a bulk warehouse: you buy in huge volumes, and you get a better deal. But here’s the catch: that discount doesn’t reach everyone. If you’re uninsured, underinsured, or paying out-of-pocket, you’re stuck with the full list price. That’s why one person pays $6 for a generic, while another pays $500 for a brand-name drug they can’t afford.
How Other Countries Control Prices
Most developed countries use one of two strategies:- Price caps: The government sets a maximum price for each drug, regardless of how many companies make it.
- Reference pricing: They look at what other countries pay and set their price based on the lowest one.
The Real Cost of Innovation
Pharmaceutical companies argue that high U.S. prices fund global innovation. They say if the U.S. lowered prices, drugmakers would stop investing in new treatments. There’s some truth to that. The U.S. does spend more on R&D than any other country. But here’s the flip side: most of that spending goes into marketing, not science. A 2023 study found that drug companies spend nearly twice as much on advertising and administration as they do on research. And here’s another angle: other countries get the same drugs. A cancer drug developed in the U.S. is sold in Germany, Canada, and Australia at a fraction of the price. Those countries benefit from American innovation without paying American prices. That’s called “free riding.” But if the U.S. cuts prices too much, companies might stop launching new drugs here first. They might delay U.S. availability to protect profits elsewhere. That’s what happened with some new biosimilars in 2024.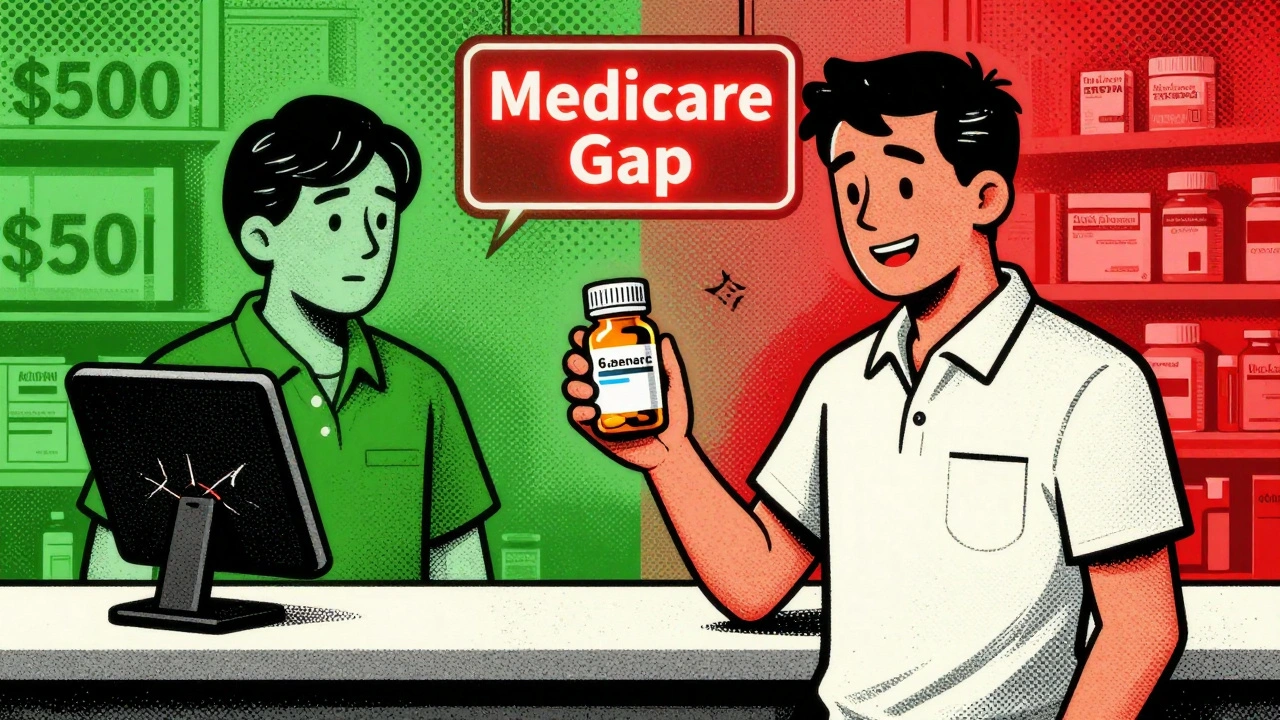
What This Means for You
If you take generics, you’re getting a bargain. You’re paying less than people in most other rich countries. Your $6 pill is cheaper than in the U.K., Canada, or Japan. But if you need a brand-name drug, you’re paying more than anyone else. And if you’re uninsured or underinsured, that gap can be life-changing. Here’s what you can do:- Ask your doctor if a generic is available. It’s not just cheaper-it’s just as effective.
- Use pharmacy discount cards. GoodRx, SingleCare, and others often beat insurance prices for generics.
- Check if your drug is part of Medicare’s negotiation program. The next 15 drugs will be announced in early 2026.
- If you’re on Medicare Part D, know your coverage gap. Some drugs are cheaper after you hit the gap.
What’s Coming Next
The U.S. government is expanding its drug price negotiations. By 2027, Medicare will be negotiating up to 60 drugs. That could bring down prices for high-cost brand-name drugs-but not generics. Meanwhile, more biosimilars (generic versions of biologic drugs) are hitting the market. These are complex drugs like Humira and Enbrel, which used to cost $2,000 a month. Now, biosimilars are selling for 15-30% less. The FDA is also speeding up generic approvals. More competition means lower prices. But there’s a risk: if too many companies enter a market, some go bankrupt. Then, the remaining ones raise prices. That’s happened with antibiotics and older generics like doxycycline. The truth? The U.S. system is broken-but not in the way most people think. It’s not that everything is expensive. It’s that the system protects the rich and punishes the vulnerable. Generics? They’re a win. Brand names? They’re a gamble.Final Take
If you’re taking a generic drug, you’re getting one of the best deals in global healthcare. The U.S. has built the most competitive generic market on Earth. That’s something to be proud of. But if you’re stuck with a brand-name drug, you’re paying more than anyone else for the same medicine. That’s not a feature of the system. It’s a flaw. The solution isn’t to copy Europe. It’s to fix what’s broken: bring negotiation to more drugs, close the coverage gap, and make sure no one pays full price for a pill that costs pennies to make.Are generic drugs in the U.S. really cheaper than in other countries?
Yes. According to the 2022 RAND Corporation study, U.S. generic drug prices are 33% lower on average than in 33 other developed countries. For example, a 30-day supply of generic lisinopril costs around $4 in the U.S., while it’s $12 in Canada and $15 in Germany. This is because the U.S. allows many manufacturers to produce the same generic, driving prices down through competition.
Why are brand-name drugs so expensive in the U.S.?
The U.S. doesn’t regulate drug prices for brand-name medications. Companies set their own list prices, and insurers often pay through secret rebates. Unlike countries like Canada or Japan, the U.S. government doesn’t negotiate prices for most patients. As a result, brand-name drugs cost 3-4 times more than in other wealthy nations. For example, the diabetes drug Jardiance costs $204 in Medicare, but only $52 in Australia.
Does Medicare negotiate drug prices, and does it help?
Yes, since 2023, Medicare has been negotiating prices for the 10 most expensive drugs. The negotiated prices are still higher than in other countries-Jardiance is 3.9 times more expensive than the OECD average-but they’re lower than what Medicare paid before. The program is expanding to 15 more drugs in 2026, and eventually up to 60. It’s a step forward, but not enough to close the gap with global prices.
Can I save money on generics in the U.S.?
Absolutely. Use discount cards like GoodRx or SingleCare-they often beat insurance prices for generics. Many pharmacies also offer $4 or $10 generic lists. For common medications like metformin, atorvastatin, or levothyroxine, you can often pay under $10 for a 30-day supply, even without insurance. The U.S. generic market is so competitive that these deals are common.
Why do some generic drugs suddenly become expensive?
When too many manufacturers leave a market-due to low profits or supply issues-the remaining ones can raise prices. This happened with doxycycline and digoxin in 2022-2023. When only one or two companies make a generic, it becomes a monopoly. The FDA tracks this risk and encourages new manufacturers to enter the market, but it’s not always fast enough.
Is the U.S. paying too much for drugs overall?
Yes, but not because of generics. The U.S. spends more on pharmaceuticals than any other country because of high brand-name prices. Generics make up 90% of prescriptions but only 20% of spending. Brand-name drugs, which make up just 10% of prescriptions, account for 80% of total drug spending. Fixing brand-name pricing would cut costs dramatically.





8 Comments
Kenny Pakade
December 5 2025Wow, so now we’re supposed to cheer because our generic pills are cheaper than Canada’s? Bro, we pay $422 for brand names while everyone else pays $100. That’s not a win-that’s a national shame. You think competition fixes everything? Try telling that to the guy who can’t afford insulin because his ‘cheap’ generic got pulled because the manufacturer went bankrupt from price wars. This system doesn’t work for people-it works for Wall Street.
Ashish Vazirani
December 7 2025Let me tell you something... In India, we pay $0.20 for lisinopril at the local chemist-and no one has insurance! The U.S. has 773 generics approved? Ha! We have 12 companies making the same pill in one city. You call that competition? You call that healthcare? You pay $6 for a pill... but your government lets pharma CEOs buy yachts with your suffering. I’m not mad-I’m just disappointed. 😔
pallavi khushwani
December 8 2025It’s funny how we focus on the $6 pill while ignoring the $500 one. We’re so quick to celebrate the win for generics, but never talk about the people who can’t even get to that counter. It’s like throwing a party in the kitchen while the living room is on fire. Maybe we need to stop calling it a ‘system’ and start calling it a lottery. Some win, most lose. And the house always wins.
Katie O'Connell
December 9 2025While the empirical data regarding net pricing and bulk purchasing power is statistically compelling, one must not conflate economic efficiency with moral equity. The structural asymmetry in access-wherein uninsured individuals are subjected to gross pricing while institutional payers benefit from negotiated discounts-constitutes a profound violation of distributive justice. One cannot celebrate market competition as a panacea when the market explicitly excludes the most vulnerable.
Jackie Petersen
December 11 2025They don’t want you to know this-but the FDA and Big Pharma are in cahoots. The ‘competition’ is fake. They let just enough generics in to keep the price low for middle-class folks, but they kill off the small manufacturers with regulatory delays. That’s why doxycycline spiked. It’s not supply-it’s control. And now Medicare’s ‘negotiating’? Please. They picked 10 drugs that were already cheap. They’re not fixing anything. They’re just spinning.
Kumar Shubhranshu
December 12 2025Generics are cheap because no one makes money on them. That’s why they disappear. Simple.
Geraldine Trainer-Cooper
December 14 2025So we’re proud of a system where the only thing keeping drugs affordable is sheer volume and corporate greed? That’s not a solution. That’s a temporary glitch in a broken machine. We don’t need more competition-we need to stop treating medicine like a commodity. If your life depends on it, it shouldn’t be priced by a spreadsheet.
Nava Jothy
December 14 2025Ugh. Another ‘U.S. generics are cheap’ feel-good article. 🙄 Meanwhile, my cousin in Delhi gets her entire year’s supply of metformin for $3.50. And here we are, patting ourselves on the back for $6? That’s not innovation. That’s survival. And the fact that you think this is normal? That’s the real tragedy. 💔