Allergy List Update: Key Triggers, Medications, and Recent Changes
When you hear allergy list update, a revised compilation of substances and medications that trigger immune responses in sensitive individuals. Also known as allergen list revision, it’s not just a paperwork change—it’s a safety alert that can prevent hospital visits. Every year, new drugs, food additives, and environmental agents show up in reports because more people are reacting to them. Some reactions are mild—itchy skin, runny nose—but others? They can turn deadly in minutes. That’s why tracking these updates isn’t optional. It’s survival.
One big reason the list keeps changing? drug-induced allergies, allergic reactions triggered by medications, not just pollen or peanuts. Also known as pharmacological hypersensitivity, this category has grown fast. Drugs like Dostinex and prednisone, which many take without thinking, are now flagged for causing rashes, swelling, and even anaphylaxis in rare cases. Even common ones like ibuprofen or antibiotics can flip from safe to dangerous depending on your genetics or other meds you’re taking. And it’s not just pills—some topical creams, IV fluids, and even vaccine preservatives show up on updated lists.
Then there are the allergy triggers, substances that cause immune overreactions, from dust mites to mold spores to hidden food additives. Also known as allergens, they’re not always obvious. A new study found that sulfites in dried fruit and wine are causing more reactions than ever, especially in people with asthma. And don’t forget cross-reactivity—someone allergic to birch pollen might suddenly react to apples or almonds because the proteins look similar to the immune system. These connections are being mapped faster now, thanks to better testing and patient reporting.
What’s missing from old lists? antihistamines, medications used to block allergic reactions, but sometimes part of the problem. Also known as H1 blockers, they’re supposed to help—but in rare cases, the drugs themselves cause itching, dizziness, or even a rebound reaction when stopped. That’s why doctors now check if your "allergy relief" is actually making things worse. And if you’re on long-term meds like prednisone, your body’s natural response to allergens can get suppressed, making you more vulnerable when you finally stop.
The latest updates aren’t just about adding new items. They’re about removing false positives. Some substances were listed because a few people reported reactions—but later studies showed it was a coincidence, not a true allergy. That’s why smart patients now ask: "Is this confirmed by testing, or just guessed?" Blood tests and skin prick tests are more accurate than ever, but they’re still not perfect. The best defense? Keep a symptom diary. Note what you ate, took, or touched before a reaction. Share that with your doctor. It’s the fastest way to get your personal allergy list updated.
Below, you’ll find real cases and updates from recent reports—what’s new, what’s been removed, and which meds are now being watched closely. No fluff. Just what you need to know to stay safe, avoid surprises, and talk to your doctor with confidence.
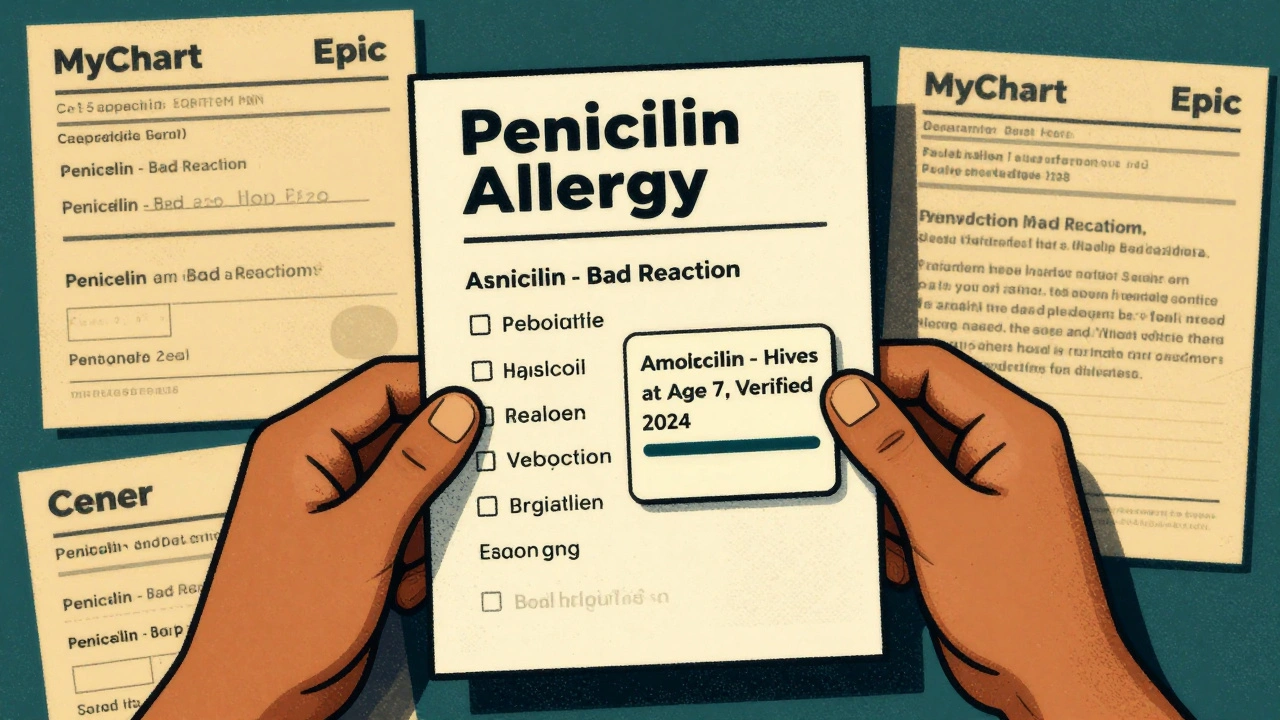
Learn how to update your allergy list across all healthcare providers to prevent dangerous medication errors. Follow a step-by-step guide to verify, correct, and sync your drug allergy records using patient portals and federal standards.
Continue Reading