Elderly Renal Impairment: Medication Risks and Safe Management
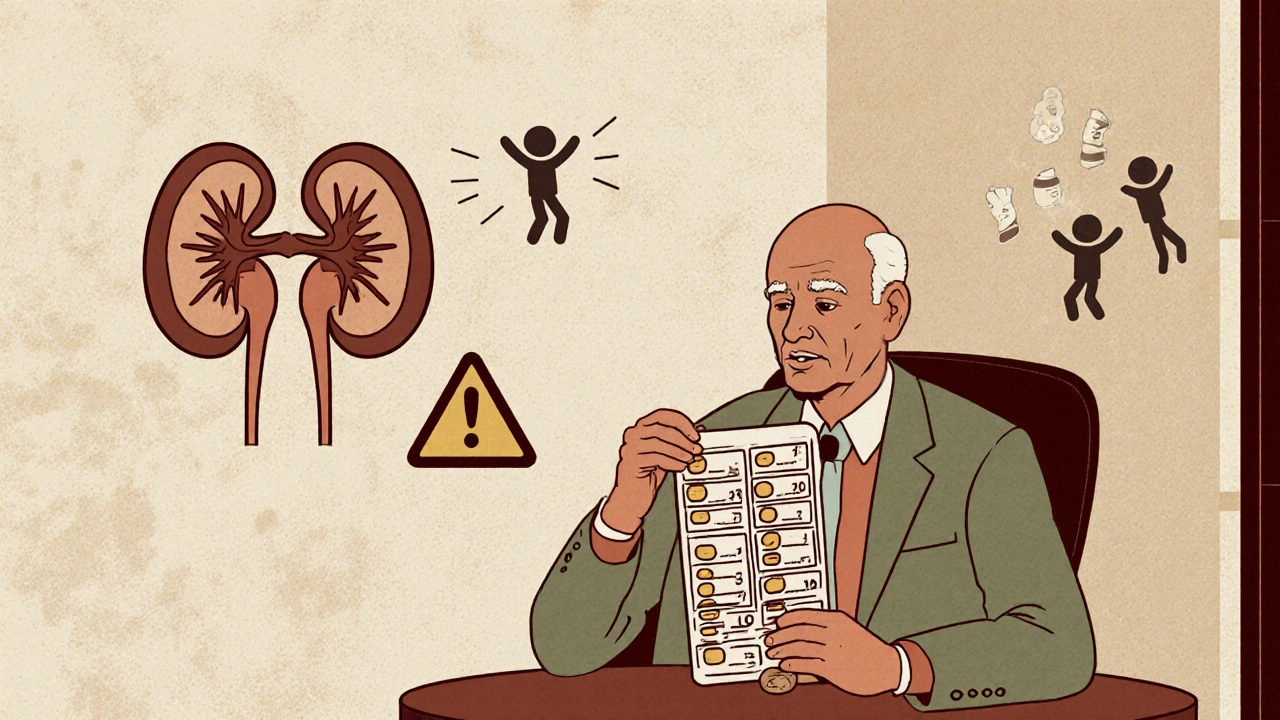
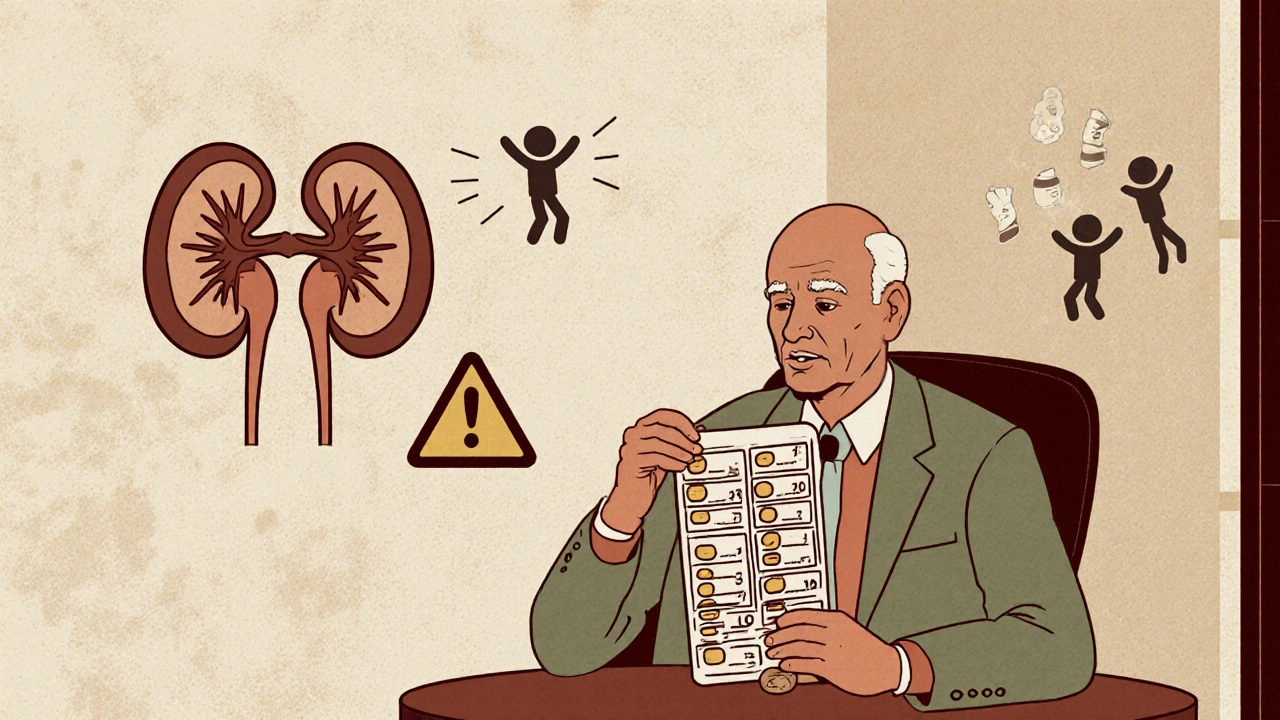
When elderly renal impairment, a decline in kidney function common in older adults that reduces the body’s ability to clear drugs. Also known as chronic kidney disease in seniors, it means even standard doses of common medications can build up to dangerous levels. Your kidneys don’t work like they used to—by age 70, most people have lost nearly half their kidney function, even if they feel fine. That’s not normal aging; it’s a silent change that turns everyday pills into potential poisons.
This isn’t just about one drug. It’s about the whole system. medication toxicity, when drugs accumulate because the kidneys can’t filter them out. Also known as drug buildup in renal failure, it’s behind many hospital visits in older adults. NSAIDs for arthritis, sulfonylureas for diabetes, blood thinners like warfarin—these aren’t dangerous because they’re bad drugs. They’re dangerous because the same dose that works for a 40-year-old can overload a 75-year-old’s kidneys. And doctors often don’t adjust the dose. Neither do patients. They just keep taking it because the label says once daily.
And then there’s renal dosing, the practice of lowering medication amounts based on kidney function, not age or weight. It’s not optional. It’s basic safety. But it’s rarely explained. A pill that’s safe for someone with healthy kidneys can cause confusion, falls, or internal bleeding in someone with reduced kidney function. The fix isn’t stopping the drug—it’s changing the dose. Sometimes it’s as simple as switching from daily to every other day, or cutting the tablet in half. But you won’t know unless you ask.
What’s worse, many seniors are on five, six, even ten medications. Each one adds up. A heart pill here, a sleep aid there, a painkiller for the knees. None of them are meant to be taken together long-term, especially with weak kidneys. That’s where drug accumulation, the gradual buildup of medication in the bloodstream due to slow clearance. becomes a real threat. It doesn’t happen overnight. It creeps in. One day you feel fine. The next, you’re dizzy, nauseous, or confused—and no one connects it to your meds.
There’s no magic test to spot this early. But there are red flags: new fatigue, loss of appetite, swelling in the ankles, trouble thinking clearly, or sudden changes in urination. If you’re over 65 and on any prescription, especially for high blood pressure, diabetes, or pain, you need to know your kidney numbers. A simple blood test—creatinine and eGFR—tells you more than any symptom ever could. And if your doctor hasn’t checked them in the last year, ask. Don’t wait for a crisis.
The posts below aren’t just about drugs. They’re about survival. You’ll find real stories and clear advice on how common medications like Lasix, prednisone, amitriptyline, and even Omeprazole can turn harmful when kidneys slow down. You’ll learn how to spot the signs of toxicity, how to talk to your pharmacist about dosing, and which over-the-counter pills to avoid. This isn’t theoretical. It’s daily life for millions. And it doesn’t have to end in the ER.
Elderly patients with kidney impairment are at high risk of drug toxicity. Learn how to adjust medication doses using GFR, avoid dangerous errors, and use the latest guidelines to keep seniors safe.
Continue Reading