Medical Malpractice: What It Is, How It Happens, and What You Can Do
When you trust a doctor with your health, you expect competence—not carelessness. Medical malpractice, a failure by a healthcare provider to meet the standard of care, resulting in harm to a patient. Also known as healthcare negligence, it’s not about bad luck—it’s about preventable mistakes that change lives. This isn’t rare. Studies show that over 250,000 people in the U.S. die each year from preventable medical errors. That’s more than car accidents or strokes. And behind every number is someone who trusted the system—and got let down.
Medical malpractice usually shows up in a few clear ways. Wrong diagnosis, when a condition is missed, delayed, or misidentified, leading to harm is one of the biggest. Think of someone with chest pain sent home with acid reflux, only to have a heart attack days later. Medication errors, including wrong dosage, wrong drug, or dangerous interactions are just as common. We’ve seen cases where a patient on blood thinners got a drug that made bleeding deadly, or someone with kidney disease got a dose that turned toxic. Then there’s surgical errors, like operating on the wrong body part or leaving tools inside—things that should never happen in a modern hospital.
It’s not always about a single mistake. Often, it’s a chain: rushed appointments, poor communication between staff, ignored lab results, or lack of follow-up. A patient with thyroid issues might get the wrong dose because their doctor didn’t check for PPI interactions. A preterm baby might suffer side effects because a nurse didn’t adjust the dose for immature kidneys. These aren’t accidents—they’re system failures.
You don’t need to be a lawyer to recognize red flags. If you were told one thing and later found out it was wrong, if your condition got worse after treatment, or if no one explained why something happened—you might be dealing with malpractice. The good news? You’re not alone. Many people have walked this path before, and there are real stories, real data, and real steps you can take.
Below, you’ll find real cases that show exactly how these errors happen—whether it’s a mood swing from prednisone no one warned you about, a drug interaction that spiked blood pressure, or a kidney patient given a toxic dose. These aren’t hypotheticals. They’re documented. They’re preventable. And they matter.
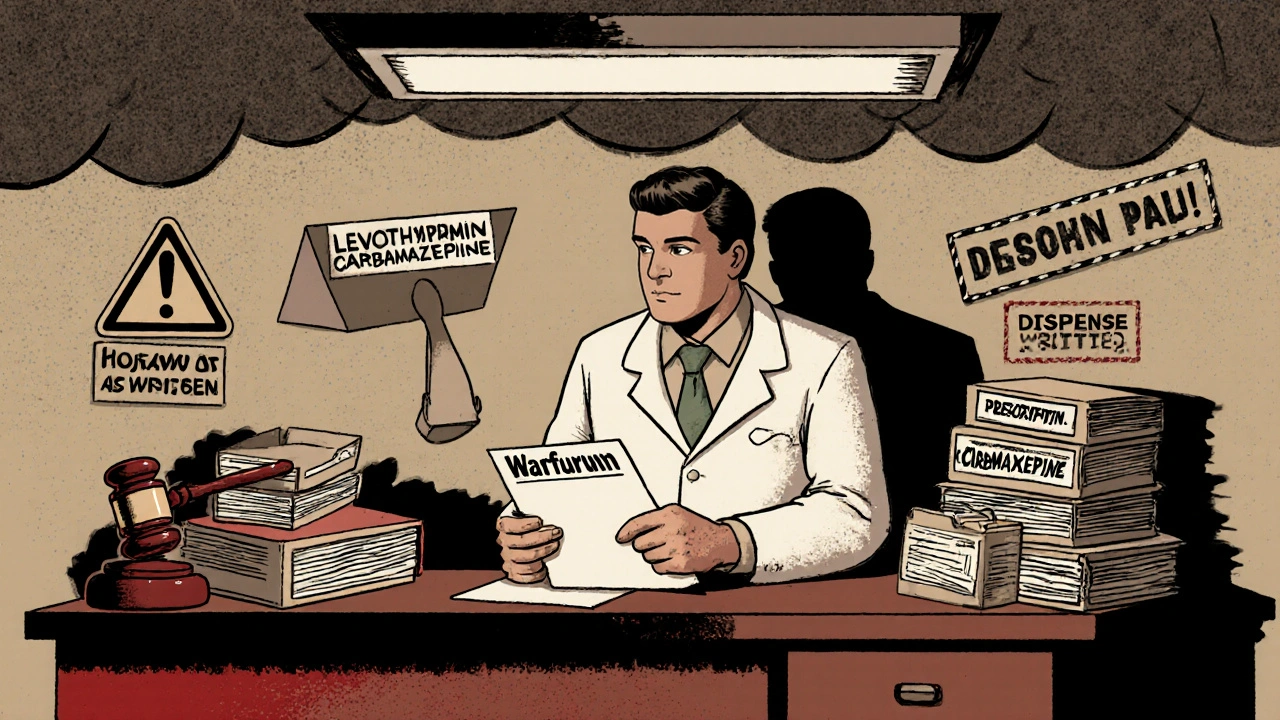
Prescribing generic drugs may save money, but it carries hidden legal risks. With manufacturers shielded from liability, physicians now face increased exposure to malpractice claims when patients are harmed. Learn how to protect yourself.
Continue Reading