Off-Target Effects: What They Are and Why They Matter in Medication Safety
When you take a medication, it’s meant to hit one specific target in your body—like blocking a receptor that causes high blood pressure or stopping a protein that feeds a tumor. But sometimes, the drug doesn’t stop there. It bumps into other proteins, enzymes, or cells it wasn’t designed to touch. That’s an off-target effect, an unintended biological reaction caused by a drug interacting with something other than its intended target. Also known as off-target activity, it’s one of the biggest reasons why even well-designed drugs can cause surprising side effects. These aren’t just minor nuisances like a dry mouth or a headache. Off-target effects can lead to serious problems—heart rhythm issues, liver damage, or even rare but deadly conditions like thrombotic thrombocytopenic purpura, which shows up in some of the posts below.
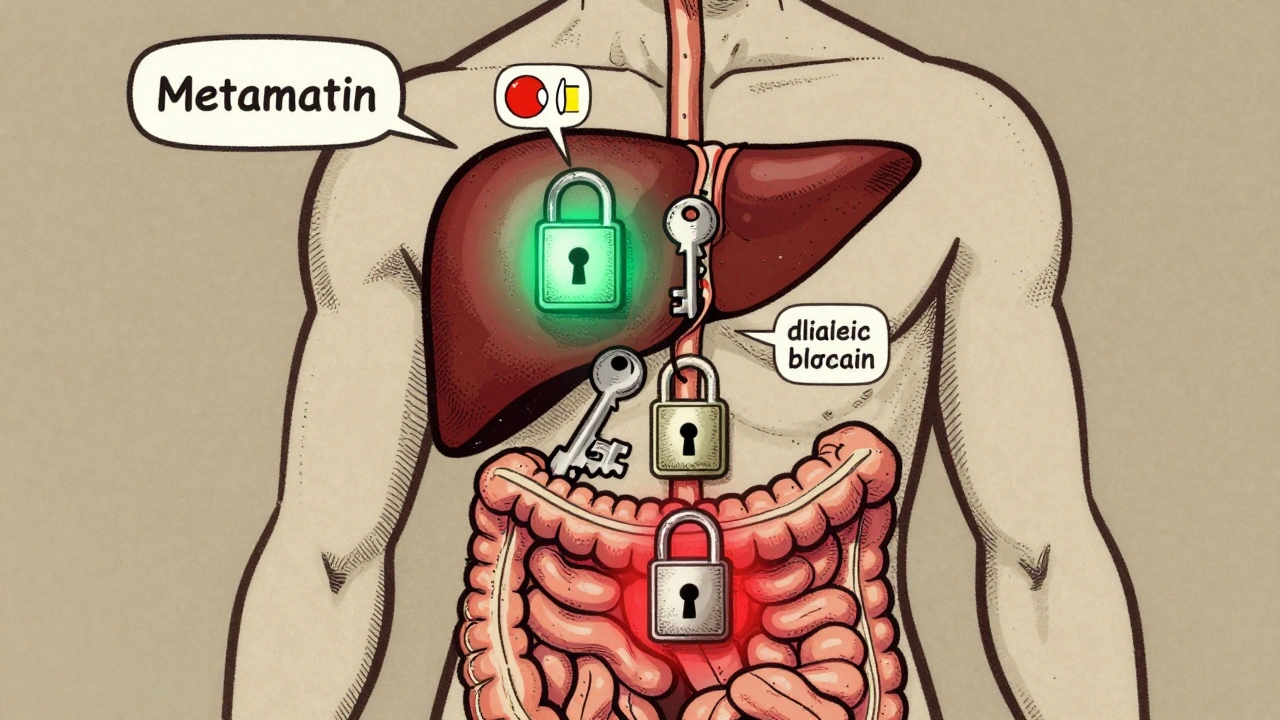
Off-target effects aren’t random. They happen because drugs are molecules, and biology is messy. A drug meant to calm nerve signals might accidentally bind to a heart cell receptor. A cancer drug targeting one mutated gene might also block a similar protein in your gut. That’s why pharmacokinetic interactions, how your body absorbs, moves, and breaks down drugs matter so much. If your liver can’t clear the drug fast enough, it builds up and starts hitting more places it shouldn’t. And when you’re on multiple medications, like someone managing diabetes, high blood pressure, and depression, the chances of one drug interfering with another’s path grow. That’s where adverse drug reactions, harmful responses to medications that go beyond expected side effects come from—not always because the drug is bad, but because the system it’s in is too complex.
You’ll find real examples in the posts below. Methadone can stretch out your heart’s electrical cycle when mixed with other drugs. Prednisone messes with your brain chemistry, not just your inflammation. Even something as simple as levothyroxine can fail to work if you’re also taking acid reducers. These aren’t edge cases. They’re common enough that doctors have to check for them every time they write a prescription. And while manufacturers test drugs for years, they can’t predict every interaction—especially in older adults, kids, or people with kidney or liver problems. That’s why knowing about off-target effects isn’t just for scientists. It’s for anyone taking meds, because the difference between a safe treatment and a dangerous one often comes down to whether you understand what else your drug might be doing.
Below, you’ll see how these hidden risks show up across different medications—from cancer therapies to sleep aids to blood thinners. Each post breaks down real cases, real risks, and real ways to protect yourself. No theory. No fluff. Just what you need to know to ask the right questions and stay safe.
Learn how on-target and off-target drug effects cause side effects, why some drugs fail in trials, and how scientists are predicting toxicity before patients take them. Real examples from cancer, heart, and diabetes meds.
Continue Reading