Patient Allergy Records: What You Need to Know to Stay Safe
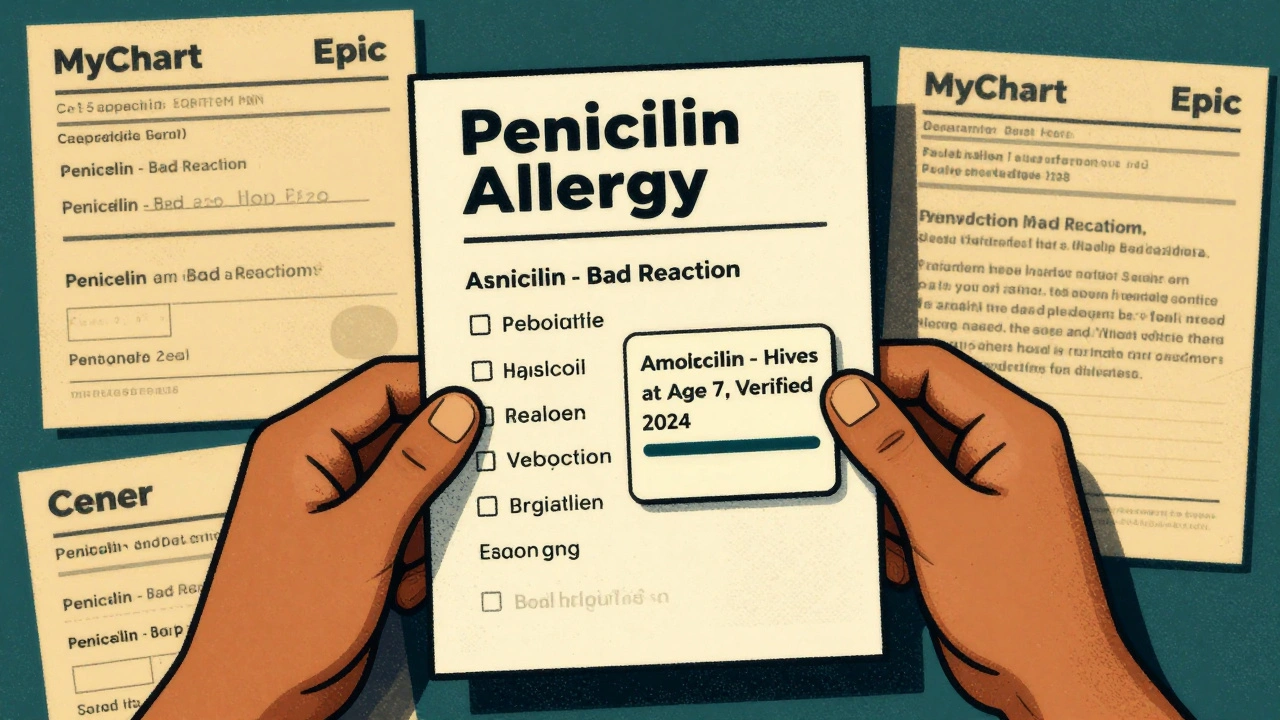
When you walk into a clinic or hospital, your patient allergy records, a documented history of adverse reactions to medications, foods, or environmental triggers that helps prevent life-threatening responses. Also known as allergy history, it’s not just a note in your chart—it’s your personal safety shield. Too many people assume their doctor already knows about their allergies, but studies show over 30% of hospital adverse events linked to allergies happen because the info was missing, outdated, or misrecorded.
These records aren’t just about penicillin or peanuts. They include reactions to drug interactions, how one medication affects another, sometimes triggering allergic or toxic responses even if the drug itself isn’t an allergen, like bile acid sequestrants blocking thyroid meds or PPIs messing with levothyroxine absorption. They cover medication-induced TTP, a rare but deadly blood disorder triggered by certain drugs like clopidogrel or quinine, and even dysosmia, when meds change your sense of smell, which can signal a neurological reaction. Your allergy record should list not just what you’re allergic to, but how bad it was—rash, swelling, trouble breathing, or anaphylaxis. Vague entries like "allergic to antibiotics" don’t help. Specifics do.
Doctors rely on these records to avoid prescribing drugs that could harm you, especially when managing complex conditions like kidney disease, heart issues, or cancer. A wrong dose of Lasix or prednisone in someone with undiagnosed allergies can spiral fast. Even compounded medications for children, custom mixes made for kids who can’t swallow pills, need accurate allergy data—wrong ingredients can be deadly in tiny bodies. And if you’re buying meds overseas or using mail-order pharmacies, your allergy history is your only protection against counterfeit or unlabeled drugs.
Keeping your records updated isn’t just your doctor’s job—it’s yours. Did a new rash show up after starting a supplement? Did you feel dizzy after a vaccine? Write it down. Tell your pharmacist. Update your phone’s health app. Bring a list to every appointment. The more accurate and complete your patient allergy records are, the safer your care becomes. Below, you’ll find real-world examples of how overlooked allergies led to dangerous outcomes, how to document them properly, and what to do when a reaction slips through the cracks.
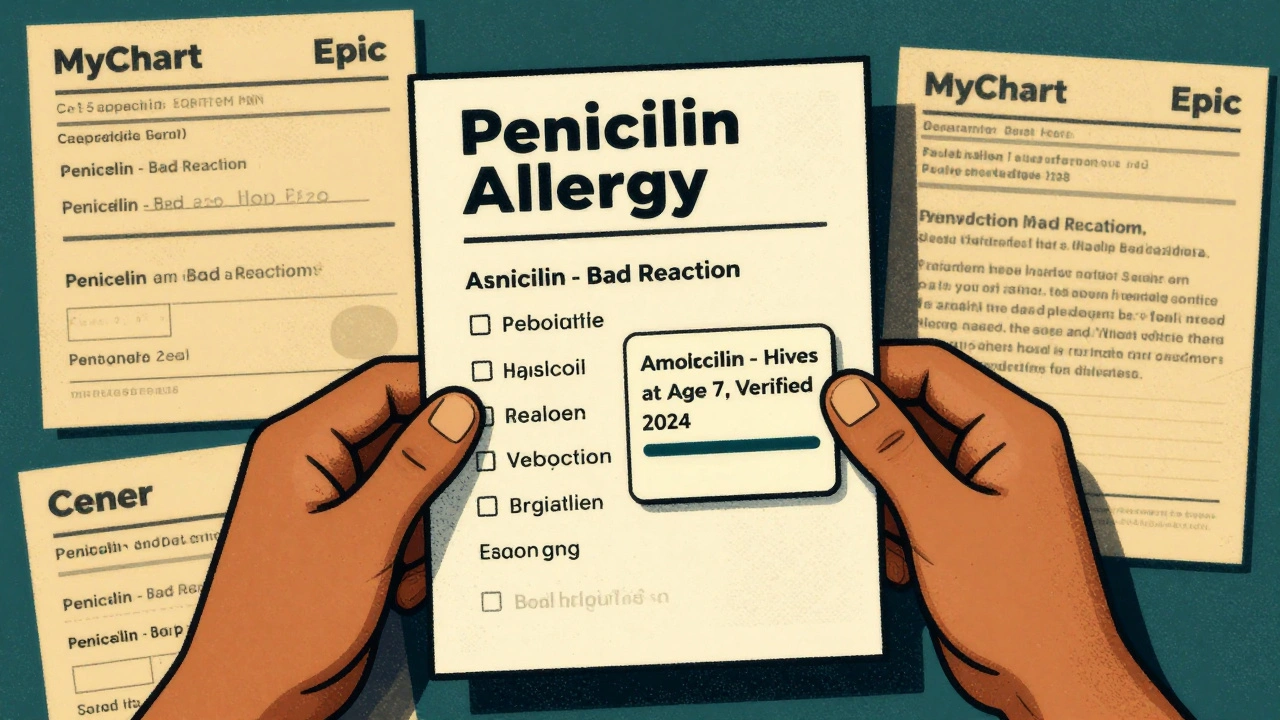
Learn how to update your allergy list across all healthcare providers to prevent dangerous medication errors. Follow a step-by-step guide to verify, correct, and sync your drug allergy records using patient portals and federal standards.
Continue Reading