Safe Dosing for Kids: What Parents and Doctors Need to Know
When it comes to safe dosing for kids, the precise amount of medication tailored to a child’s weight, age, and health status to avoid harm while ensuring effectiveness. Also known as pediatric dosing, it’s not just a smaller version of an adult dose—it’s a science that changes with every pound and every month of life. Kids aren’t little adults. Their bodies process drugs differently. Their kidneys and liver are still growing. Their fat and water content isn’t the same. A dose that’s perfect for a 10-year-old could be toxic for a 2-year-old, and too weak for a teenager.
Pediatric medication, drugs prescribed specifically for children, often requiring special formulations like liquids, chewables, or dissolvable tablets. Also known as children’s medicine, it’s one of the most misunderstood areas in healthcare. Many parents guess doses based on age alone, or use adult bottles with measuring spoons. That’s risky. Studies show over 40% of medication errors in children happen because of incorrect dosing—often from misreading labels or using kitchen spoons instead of proper syringes. Even small mistakes can lead to hospital visits. The right dose isn’t just about the number on the bottle—it’s about matching the drug to the child’s body, their condition, and how their organs handle it.
Pediatric dosing guidelines, evidence-based rules used by doctors and pharmacists to calculate safe and effective medication amounts for children based on weight, body surface area, or age. These aren’t suggestions—they’re backed by clinical data. For example, antibiotics like amoxicillin are dosed in milligrams per kilogram of body weight. A child weighing 15 kg gets a different amount than one weighing 25 kg. Even something as simple as acetaminophen needs careful calculation. Too little won’t help the fever. Too much can cause liver damage. And some drugs, like certain painkillers or cold medicines, shouldn’t be given to kids under a certain age at all.
What makes this even trickier is that kids change fast. A dose that worked last month might be too high now. Growth spurts, illness, or even a change in diet can affect how a drug is absorbed. That’s why doctors ask for updated weights at every visit. And why pharmacists double-check every pediatric prescription. It’s not bureaucracy—it’s safety.
You’ll find posts here that dig into real cases: how kidney problems in children change dosing, why some drugs are unsafe for babies, how to spot signs of overdose, and what to do when a child vomits after taking medicine. You’ll see what medications are most commonly misused, which ones require special caution, and how to talk to your doctor about dosing without sounding alarmist. These aren’t theoretical guides—they’re based on real prescriptions, real mistakes, and real outcomes.
Safe dosing for kids isn’t about being perfect. It’s about being careful, informed, and asking the right questions. Whether you’re a parent, caregiver, or healthcare worker, the goal is simple: give the right amount, at the right time, in the right way. And avoid the mistakes that too many families don’t even realize they’re making.

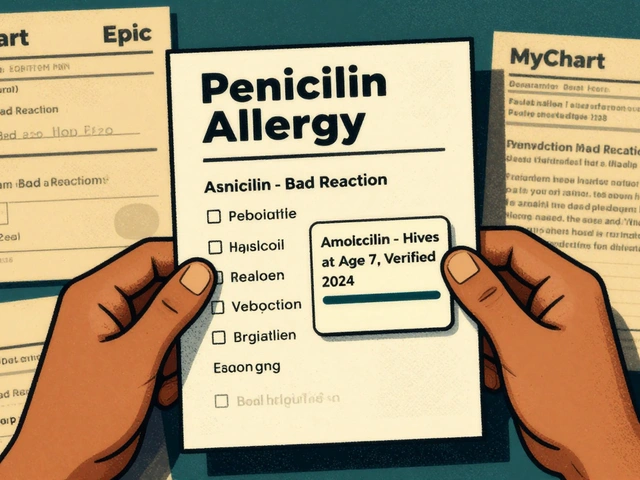
Compounded medications for children can be lifesaving-but only if used safely. Learn how to verify doses, choose accredited pharmacies, and avoid deadly errors that come with unregulated custom drugs.
Continue Reading