Surgery for Cancer: What You Need to Know About Procedures, Risks, and Recovery
When you hear surgery for cancer, a medical procedure to remove tumors or affected tissue to treat or control cancer. Also known as oncology surgery, it's one of the oldest and still one of the most effective ways to fight solid tumors. It’s not just cutting out a lump—it’s a precise, planned step in a bigger treatment plan. For many people, especially with early-stage cancer, surgery is the best chance for a cure.
Not all cancers need surgery. Blood cancers like leukemia rarely do. But for tumors in the lung, breast, colon, skin, or prostate, removing the mass is often the starting point. Surgeons don’t just take out the tumor—they also check nearby lymph nodes to see if cancer has spread. This helps doctors decide if you need more treatment after surgery, like targeted therapy, a type of cancer treatment that uses drugs to attack specific genetic changes in cancer cells, or radiation. The goal isn’t just to remove cancer, but to remove it completely without leaving behind cells that could grow back.
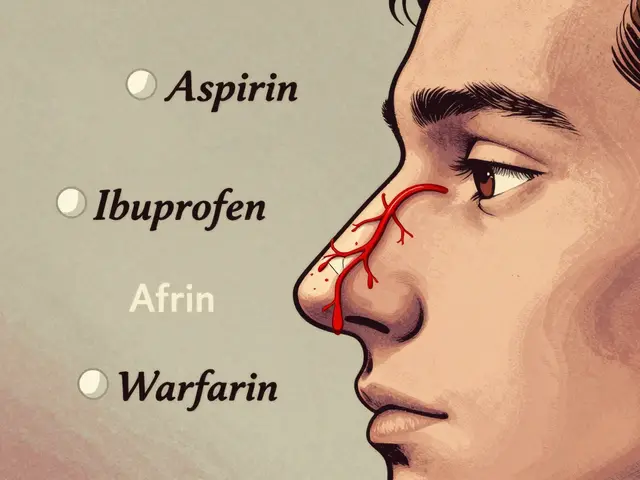
Recovery from surgery for cancer, a medical procedure to remove tumors or affected tissue to treat or control cancer can be tougher than regular surgery. Your body is already under stress from the disease, and the operation adds more. Some people need weeks to heal; others need months. Pain, fatigue, and even changes in how you eat or move are normal. But knowing what to expect helps you prepare. For example, if you’re having bowel surgery, you might need a temporary colostomy. If it’s breast cancer surgery, reconstruction options are part of the conversation. And if you’re on anticoagulants, medications that prevent blood clots, often used before or after major surgery, your team has to carefully time when to pause and restart them to avoid bleeding or clots.
There’s no one-size-fits-all approach. A small skin cancer might need 15 minutes and a stitch. A pancreatic cancer operation can take six hours and require a hospital stay of two weeks. Your age, overall health, and the cancer’s stage all shape the plan. And while surgery can be life-saving, it’s not without risks—infection, scarring, nerve damage, or even complications from anesthesia. That’s why your care team weighs the benefits against the downsides before moving forward.
You’ll find real stories and practical advice below. Some posts explain how to manage side effects after surgery. Others show how blood thinners are handled before an operation. There’s even info on how drug interactions can affect recovery. Whether you’re a patient, a caregiver, or just trying to understand what’s ahead, these articles give you the clear, no-fluff facts you need—not hype, not guesswork.

Radiation and surgery are both effective for early-stage cancer, but they come with very different risks, recovery times, and side effects. Learn how to choose the right local control strategy based on your cancer type, health, and personal priorities.
Continue Reading