Carbamazepine Generics: Enzyme Induction and Drug Interactions Explained
When you take carbamazepine for epilepsy or nerve pain, you’re not just taking a pill-you’re managing a complex biological system. The drug works by calming overactive nerves, but its real challenge lies in how it changes your body’s chemistry. Carbamazepine doesn’t just sit there. It triggers your liver to produce more enzymes that break down not just itself, but also other medications you might be taking. This is called enzyme induction. And when you switch from one generic version to another, even if the label says the same thing, your body might respond differently. That’s why carbamazepine generics aren’t as interchangeable as people think.
How Carbamazepine Induces Enzymes
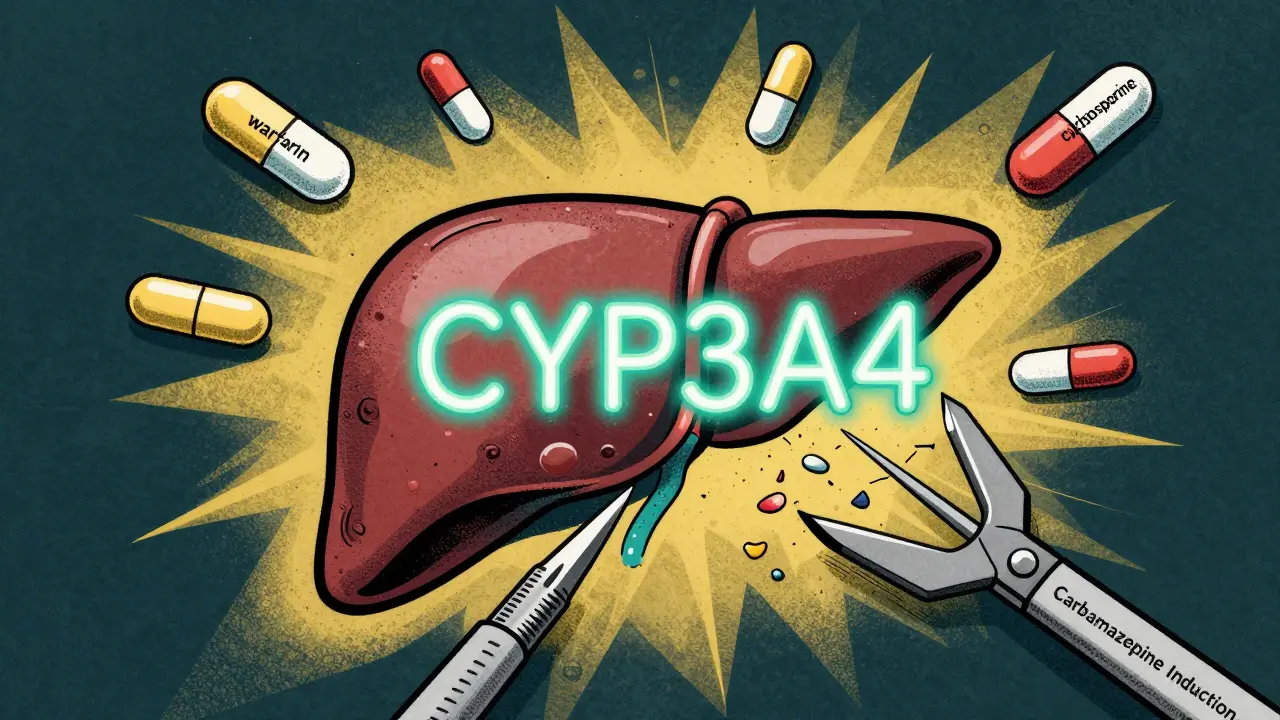
Carbamazepine is one of the strongest inducers of the CYP3A4 enzyme in the liver. This enzyme handles about half of all prescription drugs. When carbamazepine enters your system, it tells your liver to make more of this enzyme. Within 48 hours, the process starts. By two to three weeks, it’s at full force. And here’s the catch: it doesn’t just speed up its own breakdown. It speeds up the breakdown of other drugs too.
That means if you’re on warfarin for blood thinning, your INR might drop suddenly. If you’re taking cyclosporine after a transplant, your levels could crash, risking organ rejection. Even birth control pills can become less effective. The FDA lists over 20 medications with reduced effectiveness when taken with carbamazepine, including antifungals, HIV drugs, and blood pressure pills like amlodipine. The problem isn’t the dose-it’s that your body is now processing those drugs faster than before.
What makes this worse is that carbamazepine also induces UGT enzymes and P-glycoprotein, which help clear drugs from your gut and brain. So even if your liver isn’t the only issue, your body’s entire drug-clearing system is being turned up. This isn’t a minor side effect. It’s a systemic shift that can change how every other medication works in your body.
Why Generic Versions Aren’t Always the Same
All generic carbamazepine must meet FDA standards: they must deliver 80% to 125% of the brand’s absorption. That sounds precise, but it’s not enough for a drug with a narrow therapeutic window. Carbamazepine’s effective range is only 4 to 12 mcg/mL. A drop below 4 means seizures might return. A rise above 12 can cause dizziness, nausea, or even toxicity.
Studies show that when patients switch between different generic versions-even ones that are technically “bioequivalent”-about 12% experience problems. Some have more seizures. Others develop new side effects like rashes or confusion. In one study, 7.8% of those switched ended up in the emergency room. Why? Because bioequivalence is tested in healthy volunteers on a single dose. Real patients? They’re often older, on multiple drugs, or have liver or kidney issues. Their bodies handle the drug differently.
Extended-release formulations add another layer. The way the beads dissolve in your gut matters. One generic might release the drug slowly over 12 hours. Another might release it faster. For someone with gastroparesis or a slow digestive system, that difference can mean the difference between control and crisis. A nurse on Reddit noticed that one generic’s beads were larger than others, which affected how they dissolved in patients with delayed stomach emptying. That’s not something a standard bioequivalence test catches.
Gender, Genetics, and How Your Body Reacts
Men and women metabolize carbamazepine differently. Women tend to break it down faster because they have higher levels of CYP3A4. That means women often need slightly higher doses to stay in the therapeutic range. But here’s the twist: hormonal changes during the menstrual cycle, pregnancy, or while using birth control can shift that metabolism again. A 2021 study found women of childbearing age had 22% more breakthrough seizures after switching generics-likely because their enzyme activity fluctuated with hormones.
Genetics play a huge role too. About 15% of people of Asian descent carry the HLA-B*1502 gene. If they take carbamazepine, they have a 10 times higher risk of developing Stevens-Johnson Syndrome-a life-threatening skin reaction. That’s why screening is required before starting. But even beyond that, other gene variants affect how fast you process the drug. One variant, CYP3A4*22, means you need 25% less carbamazepine to reach the same blood level. Most doctors don’t test for this. But if you’ve had trouble with generics before, it might be worth asking.
Therapeutic Drug Monitoring: Your Best Defense
If you’re on carbamazepine, especially a generic version, you need regular blood tests. Not once a year. Not just when you feel off. You need them after any switch, any dose change, or if you start or stop another medication. The ideal time to test is 7 to 14 days after switching. That’s when levels stabilize.
A drop of more than 15% in your blood concentration is a red flag. It doesn’t mean the generic is bad. It means your body is handling this version differently. Your doctor might need to adjust your dose-even if you’re on the same number of milligrams. A patient on Epilepsy Foundation’s forum saw her level drop from 7.2 to 4.8 mcg/mL after switching generics. She was still on the same dose. But 4.8 is near the bottom of the safe range. No wonder her seizures increased.
Doctors who manage epilepsy know this. The American Epilepsy Society recommends keeping patients on the same manufacturer whenever possible. If you’ve been stable on one generic, don’t let your pharmacy switch you without telling you. Ask for the brand name or specific manufacturer on your prescription. Use the “dispense as written” code (DAW 1). That stops automatic substitution.
What You Can Do Right Now
- Check your current brand. Look at your pill bottle. Note the manufacturer name. If you’ve been switched before, write it down.
- Ask for a blood test. If you’ve switched generics recently, request a carbamazepine level check in 7-10 days.
- Don’t assume all generics are equal. Just because two pills say “carbamazepine 200 mg” doesn’t mean they act the same in your body.
- Tell your pharmacist. If you’ve had issues before, say so. Pharmacists can flag your profile to prevent future switches.
- Watch for new symptoms. Dizziness, rash, nausea, confusion, or more seizures? These aren’t normal. They could mean your levels dropped-or spiked.
There’s no perfect solution yet. The FDA is working on better testing methods for drugs like carbamazepine. But until then, the burden is on you and your doctor to stay vigilant. You’re not just taking a generic drug. You’re managing a delicate chemical balance. And that balance can shift with a simple pharmacy change.
What to Do If You’re Starting Carbamazepine
If you’re new to carbamazepine, start low and go slow. Your doctor should begin with a low dose and increase gradually. Monitor for side effects. Get your first blood level check at 2 weeks. If you’re of Asian descent, ask for HLA-B*1502 screening before starting. If you’re positive, carbamazepine might not be the right choice. Alternatives like levetiracetam or lacosamide don’t carry the same enzyme-inducing risks.
And if you’re on other medications? Bring your full list to every appointment. Even over-the-counter drugs like St. John’s Wort can interfere. Your pharmacist can run a drug interaction screen-but only if they know what you’re taking.
Looking Ahead: Precision Dosing
The future of carbamazepine treatment isn’t just about which generic you get. It’s about personalizing the dose based on your genes, your sex, your weight, and your other medications. Researchers are already building algorithms that predict how you’ll metabolize the drug. One study showed these models could reduce adverse events by 30-40%. In five years, we might not just ask, “What generic are you on?” We might ask, “What’s your CYP3A4 genotype?”
Until then, awareness is your best tool. Know your numbers. Know your manufacturer. Know your body. Because with carbamazepine, the smallest change can have the biggest consequence.
Can I switch between different generic carbamazepine brands safely?
Switching between different generic carbamazepine brands carries risk, especially if you have epilepsy or a narrow therapeutic index. Studies show about 12% of patients experience therapeutic failure or new side effects after switching-even when the products meet FDA bioequivalence standards. This is because bioequivalence is tested in healthy adults on single doses, while real patients often have comorbidities, polypharmacy, or altered metabolism. If you’ve been stable on one generic, avoid switching unless monitored with blood tests. Always consult your neurologist before changing manufacturers.
Why does carbamazepine reduce the effectiveness of other drugs?
Carbamazepine strongly induces the CYP3A4 enzyme in the liver, which is responsible for breaking down about half of all medications. This includes anticoagulants like warfarin, immunosuppressants like cyclosporine, HIV drugs, birth control pills, and even some blood pressure medications. When carbamazepine boosts this enzyme, your body clears those other drugs faster, lowering their blood levels and reducing their effect. This induction starts within 48 hours and peaks in 2-3 weeks. Always review all medications with your doctor when starting or stopping carbamazepine.
How often should I get my carbamazepine level checked?
If you’re on carbamazepine, especially a generic version, get your blood level checked at baseline, then 7-14 days after any dose change or manufacturer switch. A second check at 4 weeks helps confirm stability. The therapeutic range is 4-12 mcg/mL, but individual needs vary. If your level changes by more than 15% after a switch, your dose may need adjustment-even if the milligram amount is the same. Patients with epilepsy, liver disease, or those on multiple medications should be monitored more frequently.
Are there genetic tests I should take before starting carbamazepine?
Yes. If you’re of Asian descent (particularly Han Chinese, Thai, Malaysian, or Filipino), you should be tested for the HLA-B*1502 gene before starting carbamazepine. Carriers have a 10-fold higher risk of developing Stevens-Johnson Syndrome, a life-threatening skin reaction. Screening is recommended by the FDA and is now standard practice in many clinics. Even if you’re not Asian, some genetic variants like CYP3A4*22 affect how you metabolize the drug, so pharmacogenetic testing may be useful if you’ve had unexpected side effects or poor response.
Can women on birth control take carbamazepine safely?
Carbamazepine reduces the effectiveness of hormonal birth control by increasing the breakdown of estrogen and progesterone. This raises the risk of unintended pregnancy. Women on carbamazepine should use non-hormonal contraception (like IUDs) or a backup method (like condoms). Even if you’ve been on the same birth control for years, carbamazepine’s enzyme induction can lower hormone levels over time. A 2021 study found women on carbamazepine had 22% higher rates of breakthrough seizures during certain phases of their cycle due to hormonal effects on metabolism. Always discuss contraception with your neurologist and OB-GYN.