Drug Substitution: Safe Swaps, Risks, and What You Need to Know
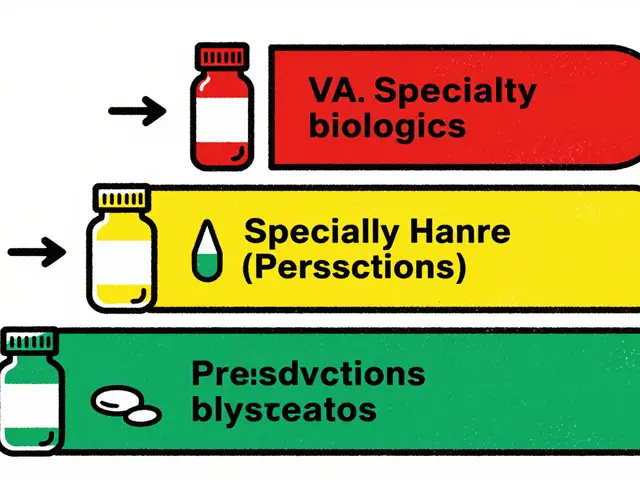
When your pharmacy gives you a different pill than what your doctor wrote, that’s drug substitution, the practice of replacing a prescribed medication with a chemically similar alternative, often a generic version. Also known as therapeutic substitution, it’s meant to cut costs without losing effectiveness—but it’s not always harmless. Many people assume generics are just cheaper copies of brand-name drugs, and in most cases, they are. But when you’re taking multiple meds, or have a chronic condition like thyroid disease or kidney problems, even small differences in how a drug is absorbed or processed can throw your whole treatment off track.
Not all drug substitutions, the replacement of one medication with another that has a similar effect, often used in cost-saving pharmacy practices. Also known as therapeutic substitution, it is commonly applied in chronic disease management. are equal. For example, swapping levothyroxine brands can raise your TSH levels, even if both are labeled the same. That’s because fillers, coatings, and release rates vary. The same goes for blood thinners like warfarin and DOACs—switching brands or generics without monitoring can lead to dangerous bleeding or clots. And if you’re on methadone, a small change in formulation might increase your risk of heart rhythm problems. These aren’t theoretical risks. Real patients have ended up in the ER because a substitution went unnoticed.
Some substitutions are safer than others. Generic versions of statins like atorvastatin or antibiotics like amoxicillin usually work just fine. But when you’re dealing with drugs that have a narrow therapeutic window—like seizure meds, antidepressants, or heart drugs—even a 5% difference in absorption can matter. Your kidneys or liver might handle the new version differently. If you’re pregnant, elderly, or have liver or kidney disease, your body’s ability to process the new drug changes too. That’s why it’s not just about the name on the bottle—it’s about how your body reacts.
Drug substitution isn’t just a pharmacy decision. It’s something you should be part of. Ask your pharmacist: Is this a generic version of my usual drug, or a different drug altogether? Check your prescription label. If the name changed, ask why. If you feel different after the switch—more tired, dizzy, nauseous, or even more anxious—don’t brush it off. That’s your body telling you something’s off. Keep a simple log: what you took before, what you got now, and how you felt. Bring it to your doctor. You’re not being difficult—you’re being smart.
What you’ll find below are real stories and science-backed facts about when drug substitution works, when it doesn’t, and how to protect yourself. From how PPIs mess with thyroid meds, to why switching antidepressants can trigger side effects, to how kidney disease changes the game—these posts cover the hidden risks and smart moves you won’t hear from a pharmacy counter.
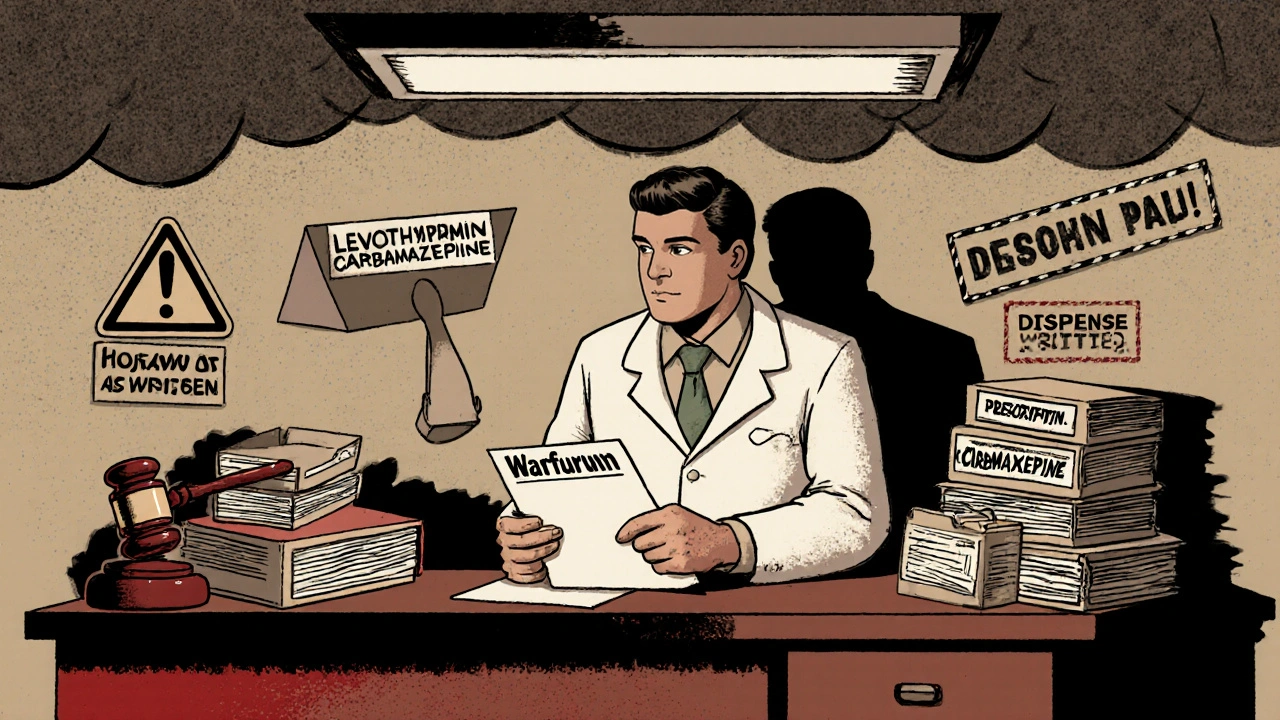
Prescribing generic drugs may save money, but it carries hidden legal risks. With manufacturers shielded from liability, physicians now face increased exposure to malpractice claims when patients are harmed. Learn how to protect yourself.
Continue Reading