Pharmacy Benefit Managers: How They Control Your Prescription Costs
When you pick up a prescription, the price you see isn’t set by your doctor or the pharmacy—it’s often decided by a pharmacy benefit manager, a middleman that negotiates drug prices between insurers, pharmacies, and drug makers. Also known as PBMs, these companies control access to most prescription drugs in the U.S., deciding which medicines are covered, how much you pay, and which pharmacies you can use. You might not know it, but PBMs are behind the confusing stack of co-pays, formularies, and mail-order mandates that make filling a prescription feel like a maze.
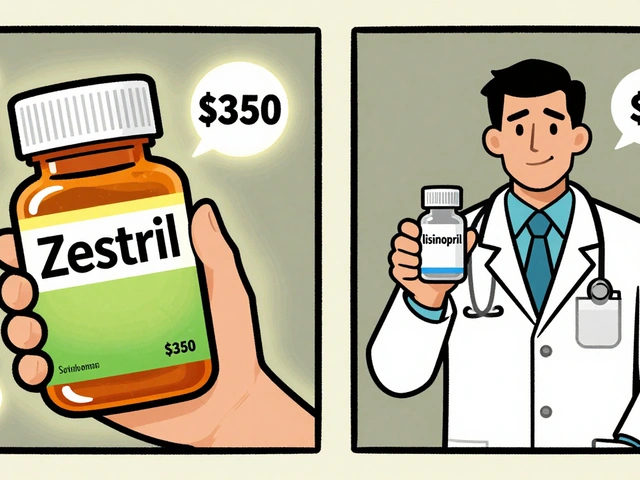
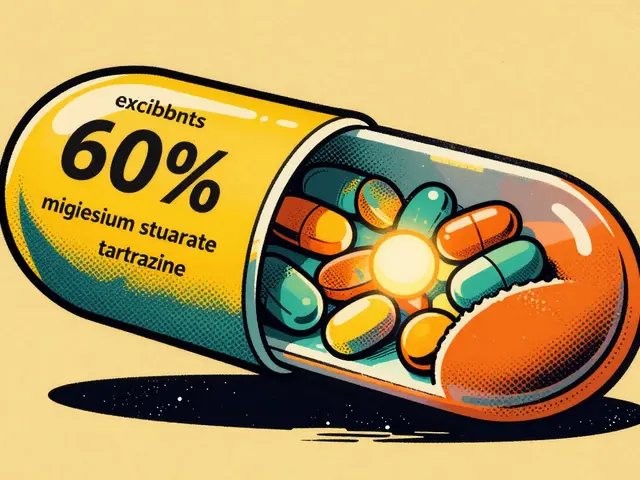
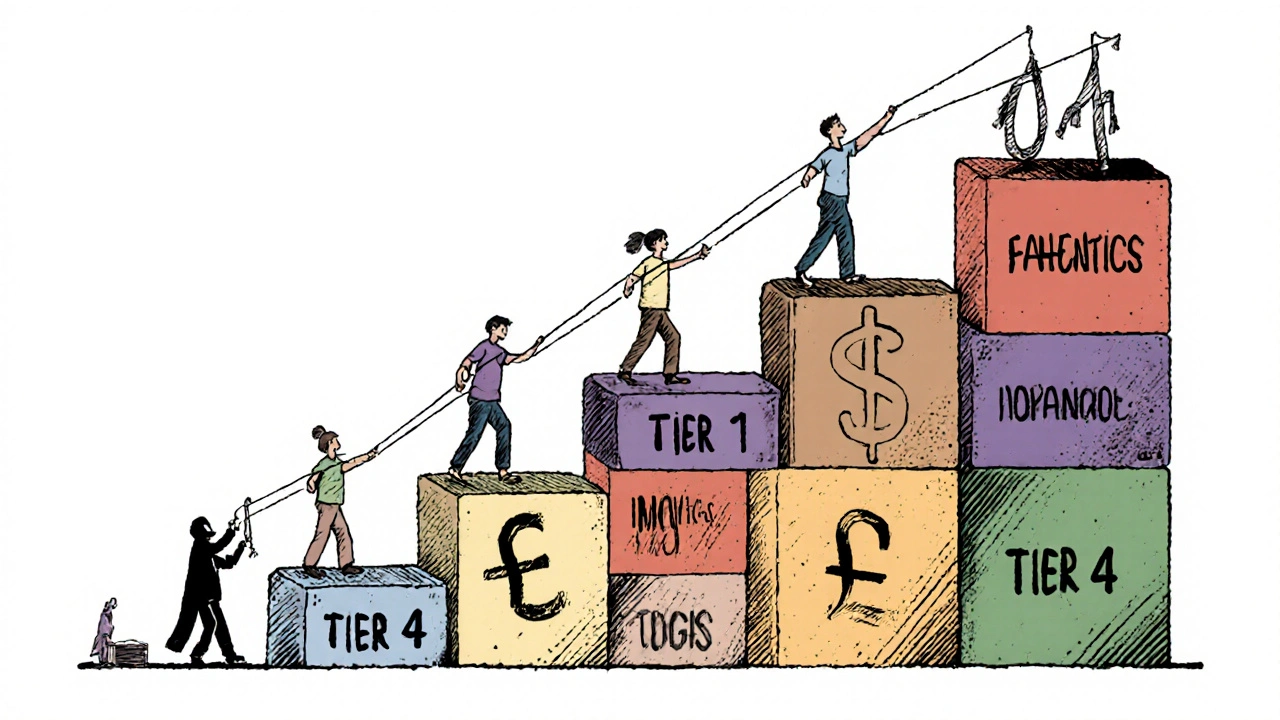
PBMs don’t just negotiate prices—they also collect rebates from drug manufacturers, often keeping a cut for themselves. This system rewards high-priced drugs over cheaper generics, which is why you might pay more for a brand-name drug than a generic version that works just as well. Drug pricing, the cost of medications set through complex negotiations between PBMs, makers, and insurers isn’t transparent, and that’s why your out-of-pocket cost can jump from $5 to $500 for the same pill depending on your plan. Medication access, whether you can get the drug you need at all, often depends on PBM formularies and prior authorization rules. Some patients wait weeks for approval just to get a basic medication, while others are pushed toward mail-order pharmacies they didn’t ask for.
These systems affect real people every day. A diabetic might be forced to switch insulins because their PBM’s rebate deal favors a more expensive version. A senior on fixed income might skip doses because the PBM’s pharmacy network doesn’t include their local drugstore. Even your doctor’s ability to prescribe freely is limited—many PBMs require step therapy, meaning you have to try cheaper drugs first, even if they’re less effective for your condition. Prescription costs, what you actually pay out of pocket for meds are shaped more by corporate contracts than medical need.
That’s why the posts here dig into the real-world impact of these hidden players. You’ll find stories about how PBMs influence everything from thyroid medication absorption to the safety of buying drugs overseas. You’ll see how drug interactions, kidney dosing, and even mental health side effects get tangled up in PBM rules. Whether you’re dealing with prednisone mood swings, GLP-1 agonists for weight loss, or trying to navigate generic drug liability, you’re navigating a system built by PBMs. What you’re about to read isn’t just about pills—it’s about who controls them, why it matters, and what you can do about it.
Insurers prefer generic drugs because they cut costs by up to 95% while maintaining effectiveness. Learn how formularies control prescriptions, why biosimilars are tricky, and what you can do to save money.
Continue Reading