Metronidazole Neuropathy: Recognizing Numbness and Tingling Before It’s Too Late
Metronidazole Neuropathy Risk Calculator
Calculate Your Dose Risk
Track your metronidazole use to identify neuropathy risk before symptoms worsen.
Your Cumulative Dose
The article states >42g cumulative dose significantly increases neuropathy risk.
Action Steps
It’s not supposed to happen. You take metronidazole because your doctor says it’s the right drug for your infection-maybe bacterial vaginosis, a stubborn case of giardia, or a post-surgical infection. You expect relief, not numbness creeping up your toes, or a buzzing, electric tingling in your fingers that keeps you awake at night. But for some people, the very antibiotic meant to heal is quietly damaging their nerves. This isn’t rare. It’s underreported. And if you’re on metronidazole for more than a few weeks, you need to know the signs-before it’s too late.
What Metronidazole Neuropathy Actually Feels Like
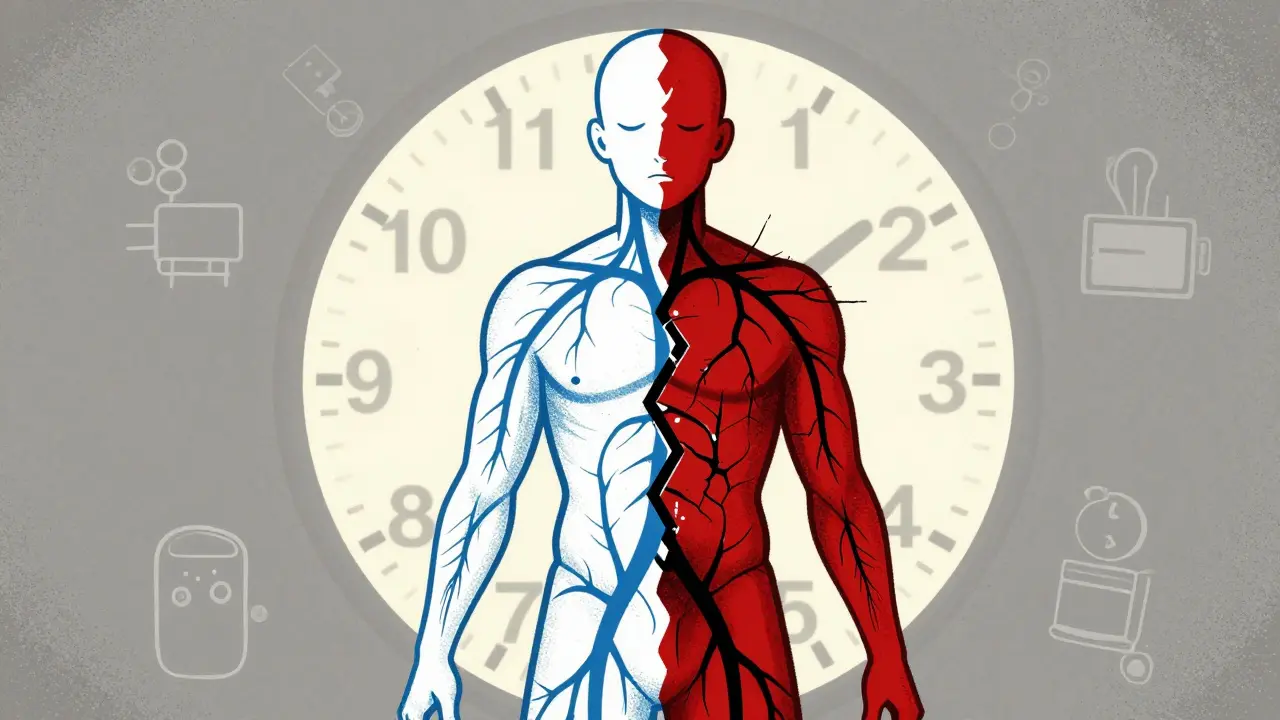
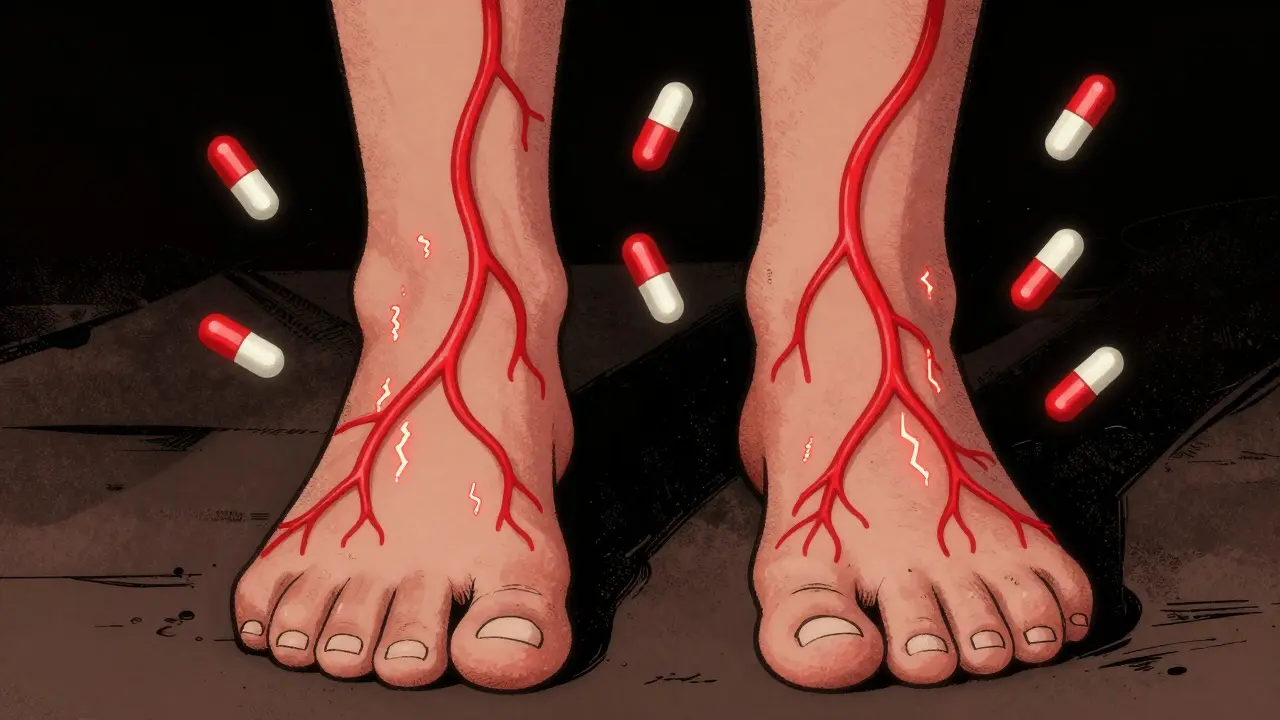
Metronidazole-induced peripheral neuropathy doesn’t start with a bang. It creeps in. First, it’s a slight loss of sensation in your feet-like walking on cotton. Then comes the tingling: a pins-and-needles feeling that doesn’t go away. Some describe it as a burning, like standing on hot pavement. Others feel electric shocks shooting through their hands or feet. These symptoms usually start in the toes and fingers and move upward, following what doctors call a "stocking-glove" pattern. It’s symmetric-both sides of the body affected the same way.
Unlike diabetic neuropathy, which often begins with numbness and progresses slowly over years, metronidazole neuropathy can hit hard and fast. One patient, a 52-year-old carpenter on a 168-gram course for a liver abscess, said the tingling in his hands made it impossible to grip tools. Another, a 69-year-old woman treated for diverticulitis, described constant burning in her feet so severe she couldn’t wear socks. Symptoms often worsen at night, disrupting sleep and daily life.
And it’s not just your limbs. Some patients report unusual autonomic symptoms-feet that feel freezing cold even in a warm room, or an inability to regulate temperature. One documented case involved a 15-year-old girl who had to submerge her legs in ice water just to ease the pain. These aren’t side effects you can ignore. They’re warning signs your nerves are under attack.
Why This Happens: The Science Behind the Damage
Metronidazole crosses the blood-brain barrier easily. Once inside nerve cells, its chemical structure-specifically the nitro group-gets broken down by enzymes, creating reactive molecules that damage mitochondria and axons. Think of it like rust eating through a wire. The nerve fibers lose their ability to send signals properly. That’s when numbness and tingling start.
The risk isn’t random. It’s tied to total dose. Research shows that once you hit 42 grams of cumulative metronidazole-roughly 500 mg three times a day for four weeks-your risk of neuropathy jumps dramatically. Patients who exceed this threshold have a 10.5 times higher chance of developing nerve damage than those who stay under it. In one study, 17.9% of patients over 42 grams developed symptoms. Only 1.7% of those under it did.
Even more alarming: symptoms can appear after as little as 10 days with high-dose regimens. That’s why doctors shouldn’t assume it’s safe just because you’re not on it for months. The damage is cumulative. And once it starts, stopping the drug doesn’t always fix it immediately.
How Often This Really Happens (And Why It’s Hidden)
Metronidazole is one of the most prescribed antibiotics in the U.S., with over 10 million prescriptions filled each year. It’s cheap, effective, and widely used for anaerobic infections, H. pylori, and even as a prophylactic for C. diff. But because neuropathy is rare in short courses, and because symptoms mimic other conditions, it’s often missed.
Many patients with diabetes get misdiagnosed. Their numb feet? "Just diabetic neuropathy," doctors say. But if they’ve recently started metronidazole, the real culprit is the drug. A 2021 study found that nearly 40% of cases in diabetic patients were initially misattributed. That delay means the nerve damage keeps growing.
Doctors aren’t always trained to connect the dots. A 2023 survey showed only 38% of primary care physicians knew the 42-gram risk threshold. Even fewer ask patients about tingling or numbness during follow-ups. Meanwhile, the FDA updated its warning label in 2023 to highlight this risk-but many patients still don’t get the message.

What to Do If You’re on Metronidazole Long-Term
If you’re taking metronidazole for more than two weeks, here’s what you need to do:
- Know your total dose. Keep track. 500 mg three times a day for 14 days = 21 grams. 21 days = 31.5 grams. At 28 days, you’re at 42 grams-the danger zone.
- Check your feet and hands daily. Are you losing sensation? Do your fingers tingle when you type? Is walking painful? Don’t wait for it to get worse.
- Ask your doctor about alternatives. Is metronidazole absolutely necessary? Are there other antibiotics with lower neurotoxic risk? For bacterial vaginosis, clindamycin cream may be just as effective without the nerve risk.
- Request a neurological check. If you’re on it for more than 4 weeks, ask for a simple screening: a monofilament test for foot sensation, or a vibration test with a tuning fork. These take 2 minutes and can catch early damage.
Some hospitals, like Mayo Clinic, now have electronic health record alerts that block metronidazole prescriptions beyond 28 days unless an infectious disease specialist approves it. That’s a good model. If your doctor doesn’t use one, you need to be your own advocate.
Recovery: Is the Damage Permanent?
The good news? In 94% of cases, symptoms improve or disappear after stopping metronidazole. The bad news? Recovery can take months. One patient in a 2021 case report took six full months to regain normal nerve function-even after quitting the drug. Another took 10 weeks just to stop needing pain medication.
But here’s the critical point: the longer you wait to stop, the higher the chance of permanent damage. About 6% of patients develop lasting nerve injury, even after stopping. That’s not common, but it’s enough to warrant caution. Physical therapy helps. Studies show patients who do structured rehab regain mobility 37% faster than those who don’t. Nerve regeneration is slow, but it’s possible-if you act early.
There’s also promising research. A phase II trial at UC San Francisco is testing whether alpha-lipoic acid (600 mg daily), an antioxidant, can protect nerves during metronidazole treatment. Early results suggest it may reduce neuropathy risk by up to 50%. It’s not standard yet-but if you’re on long-term therapy, it’s worth asking your doctor about.
What Your Doctor Should Be Doing
Doctors need to stop treating metronidazole like a harmless, short-term fix. The Infectious Diseases Society of America now recommends against courses longer than 42 grams unless absolutely necessary. They also advise:
- Using the lowest effective dose for the shortest time
- Documenting the reason for extended use
- Monitoring patients with a standardized tool like the Total Neuropathy Score, which checks sensation, reflexes, and pain levels
- Re-evaluating every 2 weeks for patients on therapy beyond 14 days
And if a patient reports numbness or tingling? Stop the drug. Don’t wait for an EMG. Don’t wait for blood tests. Don’t assume it’s "just aging" or "diabetes." The moment symptoms appear, metronidazole should be discontinued immediately. Delaying by even a few weeks can mean the difference between full recovery and permanent disability.
Real People, Real Stories
One Reddit user, r/Neurology, shared: "I was on Flagyl for C. diff prophylaxis for 8 weeks. I thought my numb toes were from sitting too much. By the time I got a neurologist, I couldn’t walk without a cane. Took 7 months to recover. I lost my job." Another wrote: "My doctor said, 'It’s probably nothing.' Two months later, I was diagnosed with metronidazole neuropathy. I’ve been in pain for 14 months. No one warned me."
These aren’t outliers. They’re examples of what happens when a common drug’s serious risk is ignored. Metronidazole isn’t dangerous because it’s rare-it’s dangerous because we don’t look for it.
Final Advice: Don’t Wait for the Pain to Get Worse
If you’re on metronidazole and you notice any numbness, tingling, burning, or weakness in your hands or feet-stop taking it and call your doctor today. Don’t wait for the next appointment. Don’t assume it’ll go away. Don’t let your doctor brush it off. This isn’t a side effect you can tough out. It’s a neurological emergency in slow motion.
And if you’re a doctor reading this: if your patient is on metronidazole for more than 28 days, ask them about their feet. Don’t assume they’ll volunteer it. Ask specifically: "Have you noticed any numbness, tingling, or unusual sensations in your hands or feet?" Use a simple screening tool. Document it. Protect your patient. Because the cost of one missed diagnosis isn’t just medical-it’s financial, emotional, and lifelong.
Metronidazole saves lives. But it can also steal mobility. Awareness is the only shield we have. Don’t wait for the numbness to spread.

15 Comments
Robin Williams
January 14 2026bro i was on this for 6 weeks for a tooth infection and my feet felt like they were wrapped in plastic wrap. i thought i was just tired. turned out i couldnt feel my toes for 3 months. docs just shrugged. dont wait. stop it. your nerves dont come back easy.
lucy cooke
January 14 2026how tragic that we’ve reduced human physiology to a cost-benefit spreadsheet. metronidazole isn’t a ‘drug’-it’s a molecular arsonist with a prescription pad. we celebrate efficiency while our axons turn to ash. this isn’t medicine. it’s pharmacological nihilism dressed in white coats.
Scottie Baker
January 15 2026my cousin got this after a colon surgery. told her doc she felt like ants were dancing in her fingers. he said 'maybe you’re just stressed.' two months later she was using a cane. now she’s in physical therapy. if you feel anything weird-stop. don’t be a hero. your hands matter more than your stubbornness.
Anny Kaettano
January 15 2026as a neurology nurse, i’ve seen this too many times. the stocking-glove pattern is textbook. the red flag isn’t just the dose-it’s the silence. patients don’t volunteer symptoms because they don’t know to connect the dots. we need mandatory patient handouts at script pickup. this isn’t optional education-it’s a duty.
Kimberly Mitchell
January 16 2026another ‘warning’ article. where’s the data? 17.9%? from what study? you cite a 2023 survey but no link. if you’re going to scare people, at least cite properly. also-why are you blaming doctors? patients don’t read labels either.
Diana Campos Ortiz
January 16 2026i took this for 18 days for BV. noticed tingling on day 12. stopped it. told my doctor. she said 'probably coincidence.' i went to a neurologist anyway. they confirmed early neuropathy. i’m 90% better now after 4 months. if you feel it-trust yourself. doctors aren’t mind readers.
Jesse Ibarra
January 16 2026you people are panicking over a 1.7% risk. you think your numb toes are more important than the woman who just survived C. diff? this drug saves lives. stop being hypochondriacs. if you can’t handle minor side effects, don’t take antibiotics. grow up.
laura Drever
January 17 2026metronidazole neuropathy is real but overblown. most cases resolve. stop fearmongering. also the 42g threshold? that’s from one small cohort. also why are you assuming all patients are dumb enough to not track their dose? lol
Randall Little
January 17 2026so let me get this straight-you’re telling me that in a country where we prescribe antibiotics like candy, we’re shocked that people get side effects? we have a 20-year-old with a UTI on a 30-day course of flagyl because her PCP doesn’t know what a culture is. this isn’t a drug problem. it’s a medical education problem.
Acacia Hendrix
January 17 2026the pharmacokinetics of metronidazole’s nitroreduction pathway generates reactive oxygen species that induce mitochondrial dysfunction in dorsal root ganglia neurons, leading to axonal degeneration. the cumulative dose threshold of 42g is statistically significant (p<0.001) in multiple prospective cohort studies. the delay in symptom recognition correlates with prolonged exposure and inadequate neurologic monitoring protocols.
James Castner
January 18 2026the fundamental ethical dilemma here lies not in the pharmacology of metronidazole, but in the systemic devaluation of patient autonomy within contemporary medical practice. we have created a culture where therapeutic efficacy is quantified in microbial clearance rates, while neurological integrity is treated as an incidental variable. the fact that a patient must self-advocate to prevent irreversible nerve damage speaks volumes about the erosion of the physician-patient relationship. we are not merely prescribing antibiotics-we are gambling with human sensorium, and we have normalized this risk under the guise of clinical efficiency.
Adam Rivera
January 18 2026my mom got this for a stomach bug last year. she started feeling weird in her hands and just kept going. ended up in PT. now she keeps a little notebook of every med she takes and what it does. best thing she ever did. if you’re on anything long-term, write it down. your future self will thank you.
Rosalee Vanness
January 19 2026you know what helped me? walking barefoot every morning on grass. it woke up the nerves. also, i started doing yoga stretches for my hands and feet-just 10 minutes a day. and i asked my doc about alpha-lipoic acid. she was skeptical but didn’t shut me down. recovery isn’t just stopping the drug-it’s rebuilding. your body remembers how to heal. you just gotta give it a chance.
John Tran
January 20 2026when i first got the tingling, i thought it was from my new shoes. then i thought it was sciatica. then i thought i was just aging. then i found this post. turns out i was on flagyl for 52 days for a sinus infection that didn’t need it. i cried for an hour. i lost 14 pounds because i couldn’t walk to the kitchen. now i’m on a 6-month recovery plan. never take a drug longer than your doctor says. even if they say it’s fine.
mike swinchoski
January 22 2026you’re all overreacting. my grandma took this for 3 months and never had a problem. you just want attention.